The US Department of Health and Human Services (DHHS) has substantial experience planning for and supporting the medical and public health needs for large civilian gatherings and mass casualty incidents in the United States and globally. Presidential directives,1 statutes,2 and other regulations specify DHHS leadership in public health and medical response. DHHS has supportive responsibilities as a partner with other government agencies and departments and the private sector. The National Response Framework2 and assignments in Emergency Support Function #8 “Public Health and Medical Services”3 are among the key documents outlining DHHS responsibilities. The Nuclear/Radiological Incident Annex4 outlines the roles of federal agencies for a nuclear incident.
To help all federal entities focus and coordinate their planning efforts, 15 specific types of incidents are specified in the National Planning Scenarios document, an abridged version of which is publicly available.5 The concept was that effective plans for these 15 events would be relevant and scalable with modifications for most of the kinds of incidents. It is expected that these plans would be updated as needed. National interagency drills and exercises, often with state and local partners (“state and local” includes state, regional, local, tribal, and territorial medical and public health planners and responders), typically focus on 1 or more of these scenarios. Medical planning for scenario number 1, a ground-level detonation of a 10-kiloton (kT) improvised nuclear device (IND) in a US city, is addressed in the series of articles in this special issue of Disaster Medicine and Public Health Preparedness.Reference Coleman, Knebel and Hick6Reference Knebel, Coleman and Cliffer7Reference Casagrande, Wills and Kramer8Reference Coleman, Weinstock and Casagrande9Reference Hick, Weinstock and Coleman10Reference Caro, DeRenzo and Coleman11Reference Sherman12Reference Dodgen, Norwood and Becker13Reference DiCarlo, Maher and Hick14 Of note, the Scarce Resources for a Nuclear Detonation Project uses the newer physical infrastructure damage concept in the Planning Guidance for Response to a Nuclear Detonation 15 and the casualty models developed for this project.Reference Knebel, Coleman and Cliffer7
Although presidential directives, statutes, and regulations specify generally what DHHS must do, how DHHS accomplishes those tasks demands detailed, intricate planning with both all-hazard and specific-hazard elements. Having appropriate, usable, realistic, effective, and easily understood plans is critically important, given the number, size, complexity, and diversity of possible incidents; the number of staff engaged; expected turnover of staff over time; the range of partners participating (federal, state, and local levels and the private sector); and the range and extent of needs that must be met for people affected by the blast in many types of venues.
DHHS has developed guidance documents, procedures, training programs, and tools for its own planning and response efforts. One of those tools, developed by the Office of the Assistant Secretary for Preparedness and Response, is the “playbook,” which is part of all-hazards preparedness. A DHHS playbook has been created for each of the 15 National Planning Scenarios. Redacted DHHS playbooks for several scenarios are available to the public.16 Although they were designed to be used by senior leadership at DHHS, the playbooks also serve to focus staff efforts at all levels and to guide planning and response. The goals of publishing these documents are to provide transparency and facilitate response-planning efforts by others who will be DHHS partners, so that they will know what to expect from HHS.
Playbooks have both all-hazards elements and elements that are specific for each type of mass casualty event, and they undergo revision regularly. These playbooks have been used at DHHS during weapons of mass destruction exercises and responses to actual incidents such as hurricanes and pandemic influenza. They have also been developed in collaboration with the federal Emergency Support Function #8 partners, with generally excellent reviews.
Each of the DHHS playbooks is tailored to the specific scenario, but all of them use the same basic format, including the following:
• Introduction
• Scenario
• Concept of operations
• Actions and issues
• Prescripted mission assignments
• Essential elements of information
• Briefing and decision papers for senior leadership
• Acronyms
Several state and local government partners of DHHS have suggested that they would like to adopt elements and organization of the playbook model to assist with their own medical response planning. In preparing the Hick et alReference Caro, DeRenzo and Coleman11 manuscript for this Project, it became apparent that there were sector-oriented approaches unique to state and local planners whose activities were intertwined with one another and with federal responders such as emergency medical services (EMS), initial health care facility response, public health, medical system response, evacuee medical care and fallout-related radiation illness, and recovery.
To help meet the needs of the state and local planners and enhance communication and coordination among nonfederal and federal planners, this article provides for the first time a template that state, local, regional, tribal governments and nongovernment sectors may find useful in developing their own plans for a medical response to a nuclear detonation. (For additional guidance in planning and developing an emergency operations plan, the Department of Homeland Security developed the Federal Emergency Management Agency Comprehensive Preparedness Guide.17)
This template focuses primarily on technical background information and concept of operations relevant to senior planners and responders for nonfederal entities, most of whom have limited experience with radiation incidents. All DHHS-specific sections noted above are not included because not all of them are relevant to state and local entities. Providing concise but useful information in the playbook to guide state and local planning efforts was a priority. This playbook includes the following:
• Concept of operations
• Actions and issues
• Prescripted mission assignments
• Additional information links
Presented below are excerpts from the State and Local Planners Playbook, which provide a general understanding of the organization of the playbook and the information available within. (A complete electronic version is available on the Radiation Emergency Medical Management (REMM) Web site.18 We expect that the user will modify it to suit his or her needs. This is a living document that will be updated when there are substantive additions or modifications.)
THE PLAYBOOK
Casualties caused by a nuclear detonation result from blast, heat (thermal energy), and ionizing radiation. The distribution and severity of injuries seen depend on device yield (kilotons), height of burst (air vs ground burst), atmospheric conditions (weather, wind pattern), and protection afforded by shelter/topography of the terrain (eg, urban landscape vs rural open spaces, robustness of buildings construction).15
Rescue efforts after a nuclear detonation are complex because of dangerously high radiation levels, severe infrastructural damage, the number and severity of causalities, and the inaccessibility of many victims, at least initially. A summary of the key principles of the medical and public health response of the nuclear detonation is found below.
Concept of Operations: Using Damage Zones to Organize Response Activities15
Response tasks (including search and rescue) that are likely to be safe and effective are organized by 4 concentric physical damage zones around ground zero, some of which also include radiation. Starting at ground zero and working outward, the 4 damage zones (Figure) are the following:

FIGURE Representative dangerous fallout zones for 0.1, 1.0, and 10 kT detonations in which an early and direct threat from fallout radioactivity exists.
A radiation exposure rate of 10 R/h is used to delimit this zone. Zone shapes are idealized for illustration only; actual zones are likely to be less circular in shape and boundaries between zones are less distinct. (Reprinted with permission from the Lawrence Livermore National Laboratory.)
• Severe damage (SD) zone
• Moderate damage (MD) zone
• Light damage (LD) zone
• Dangerous (DF) fallout
The following is a brief description of the expected damage zones for a 10-kT IND ground detonation and recommended rescue tasks within each zone.15
SD (no-go) zone:
• Description: few buildings structurally sound or standing; radius on the order of 0.6 mi (1.0 km) from ground zero
• Access by rescuers will be limited by massive physical damage and high radiation levels.
• Survivors in this zone will be few.
MD Zone:
• Description: at the inner boundary (entry into SD/no-go zone), all of the buildings are fallen or structurally unstable; at the outer transition from the MD to the LD zone, there will be significant structural damage approximately 1 mi (1.6 km) from ground zero. Sturdier (eg, reinforced concrete) buildings are likely to be standing; lighter commercial and multiunit residential buildings will be unstable; houses are likely to be destroyed.
• Limited rescue activities will be possible here.
LD zone:
• Description: inner boundary with MD zone will have more substantial building damage; outer boundary with the DF zone will have damage defined by the prevalence of broken windows (approximately 25%) out to 3 mi (4.8 km) from ground zero; window damage tapering out to 5 mi (8 km). As responders move inward toward ground zero, windows and doors will be blown in; gutters, roofs, and lighter-weight construction will have increasing amounts of damage; the amount of litter and rubble will increase; and more automobiles will be stalled and crashed, making emergency vehicle passage difficult.
• Many people will self-evacuate; some response efforts will be useful but difficult and dangerous due to high radiation levels.
DF (hot) zone:
• Description: The DF zone is distinguished not by structural damage, but by radiation levels from fallout. A radiation exposure rate of 10 R/h delimits the “hot zone” exterior boundary. Inside the boundary, responder operations are severely limited by the need to limit responder exposure time. The hot zone will shrink rapidly in size as the fallout decays, although the boundaries of the original DF zone are important for predicting initial radiation exposure. The radioactive decay rule of thumb: exposure rate from fallout declines 90% every 7 hours.
• Fallout particles may be visible as fine sandy material, either actively falling out as the plume passes or visible on clean surfaces. Visible fallout provides strong evidence of dangerous levels of radioactivity, but fallout may not be noticeable on rough or dirty surfaces, and no method is available to reliably estimate radiation dose rates based on the quantity of visible fallout. Therefore, visible fallout may possibly be used as an indicator of a direct radiation hazard, but the lack of apparent fallout should not replace appropriate radiation measurements.
• Responders should refrain from undertaking missions in areas where radioactivity may be present until radiation levels can be accurately determined and readily monitored. Any response operations within the hazardous DF zone must be justified, brief, and well planned.
• Before an incident, local protocols should be created that define operations in radiation-contaminated areas and optimize exposure risk vs the benefits of the potential missions.
A fifth zone, circumscribed by a “line” reflecting an environmental exposure rate of 0.01 R/h, is also useful in managing the response. It has also been called a radiation caution zone. This line and the zone within it will enlarge initially as fallout is deposited but will then contract quickly as radiation levels decrease due to rapid radioactive decay in the hours and days after a blast. This is not a damage zone per se, but it is the area outside the DF zone where response activities can be conducted. Responder time will be limited by federal protective action guides (PAGs)19 or recommendations adopted by the local incident commander. The as low as reasonably achievable (more commonly known as ALARA) principle20 will also apply in keeping radiation levels for responders as low as reasonably achievable.19
Casualty recovery will be a challenge because of both physical obstacles and high radiation levels within the MD and SD zones. The wide spectrum and severity of injuries will also pose challenges to emergency response personnel, and altered triage principles will need to be adopted to consider the impact of radiation on triage priority.
Number and Spectrum of Injuries
There will be hundreds of thousands of casualties. Injuries will vary by type and severity. Many people will have trauma only (especially in and beyond the LD zones), whereas others will have radiation exposure only (especially in the DF zone), and some will have both. The list below reflects the major kinds of injuries expected:
• Blast: Injuries from pressure wave, tumbling, and crush injuries. Puncture injuries from flying debris rather than pressure-related injuries dominate because those who would have sustained classical blast injuries are likely to have been killed by the exceptional radiation doses or burns levels in the zone where classical blast injuries would be sustained.
• Burns: Thermal energy from the detonation and burns from secondary fires and contact with hot materials during the failure of a building. It may be difficult to distinguish superficial thermal from radiation burns without a patient history.
• Radiation: Injuries from prompt radiation (instantaneous and high dose rate from detonation) and fallout (lower dose rate with most of dose being given in first few hours); depends on location and duration of exposure. Sheltering in place in the hours after the detonation is important to reduce radiation dose.
• Combined injury: Defined as radiation plus blast and/or burn. This has a worse prognosis than either blast or burn alone.
• Multiple blunt trauma and lacerations: Resulting from motor vehicle accidents that are a consequence of flash blindness from detonation (the blindness lasts a few minutes, and is worse at night when the pupils are dilated); this may occur miles away, especially at night.
• Punctures and lacerations: Punctures and lacerations from glass breakage may be occur at distances up to miles from ground zero.
Radiation Contamination
• Prompt radiation from the detonation will produce high instantaneous doses, but will not contaminate people.
• Contamination comes from radioactive fallout alighting on the individual. People inside shelters will not experience superficial contamination unless they go outside. Individuals evacuating from shelters later may contaminate their shoes and clothing in transit through the DF zone.
• Lifesaving interventions by responders take precedence over decontamination, as long as they occur in areas that are considered safe for responders.
• Decontamination is the responsibility of state and local responders and individuals. The need for decontamination as soon as possible after the incident and the time it takes federal assets to arrive make it crucial for state and local entities to manage this function, although guidance may be available from federal authorities.
• Removal of outer garments and shaking out hair removes ≥90% of external contamination. Thus, control of removed clothing is a priority for containment of radiation.
• Management of internal contamination from inhalation or ingestion is not considered a significant part of the initial response. Therefore, there is no initial role for potassium iodide, Prussian Blue, or chelating agents (eg, diethylene triamine pentaacetic acid).
Response Worker Safety
Search and rescue operations will be markedly impeded by the relatively high levels of radiation in and around the MD zone. PAGs and the ALARA principle will guide actions.151920 Safeguards for responders include, but are not limited to, the following:
• Personal protective equipment will protect emergency workers from contaminants, but it will not protect against external radiation doses.
• Respirator or self-contained breathing apparatus will protect workers from breathing in radioactive particulates.
• Real-time personal electronic dosimeters will provide readings to alert emergency workers to when exposure levels are about to exceed worker safety limits (PAGs).
• By knowing radiation levels in the work area, one can calculate turnaround times to account for worker entry, time on task, and worker exit from the radiation zone.
Triage
When working in areas approved for search and rescue, EMS workers will use their customary field triage system, which is based initially on the physical injury (eg, simple triage and rapid treatment assessment [START], jumpSTART [a variant of START for pediatric patients], sort-assess-lifesaving interventions-treatment and/or transport [SALT], and Delayed, Immediate, Minimal or Expectant [DIME] used by the Department of Defense). If resource adequacy is limited, the standard order for triage and transportation (sickest first) may need to change, as noted in the next section. Given the magnitude of the incident and the limited size of the EMS response assets available, most people will reach medical care without having been screened in the field.
The radiation dose can be estimated roughly by the physical location of the individual at the time of detonation and afterward. When available, blood counts or the clear presence of cutaneous radiation burns can be used to define precise dose estimates. Many individuals will not have been exposed to any radiation. Time to vomiting after exposure is 1 simple way to estimate the dose. However, because vomiting has numerous etiologies besides radiation, time to vomiting is not considered to be a particularly accurate method.
Acute radiation syndrome and its organ subsyndromes are diagnosed as follows:
• Hematological syndrome: Clinically relevant acute injury occurs typically at doses above 2 to 3 Gy, although lower doses may be detectable with complete blood counts and other tests. For affected individuals receiving doses >2 Gy, immediate treatment with myeloid cytokines is indicated (eg, granulocyte colony-stimulating factor). The best effects occur when administered within 24 hours of exposure. Hematologic injury may become detectable 1 to 3 weeks after exposure, after a latent phase without signs or symptoms.
• Gastrointestinal syndrome: Gastrointestinal syndrome usually results after receiving doses >5 to 6 Gy. The syndrome occurs within a few days of exposure and can be managed with aggressive treatment.
• Neurovascular syndrome: Neurovascular syndrome typically results from doses >10 Gy. It is almost always fatal, but affected individuals will benefit from palliative/compassionate care.
The general principles of triage and management by dose of whole-body exposure to radiation (with the understanding that precise dose estimation initially may be difficult) are as follows:
• <2 Gy: follow-up only (possibly for biodosimetry assessment later)
• 2 to 4 Gy: evaluation and expert monitoring within 1 to 3 weeks of exposure, with myeloid cytokines if supplies are adequate
• >4 Gy: immediate medical attention, including myeloid cytokine treatment as soon as possible
• >10 Gy: palliative/compassionate care
Combined injury is defined as significant physical trauma (and burns covering more than 20% of the total body surface area) in conjunction with a radiation dose of >2 Gy; this has much worse prognosis than either injury alone. People with only minor trauma plus radiation will be triaged and managed in the same way as those with radiation only using radiation dose as outlined above.
The scarcity of medical resources (eg, staff, space, equipment, medicines) will vary greatly by location of the medical care facility and time after the incident; this will affect the ways in which people exposed to radiation are triaged and cared for. Conventional triage attends to “the sickest first.” Resource scarcity after an IND detonation will result in a change of triage priority to provide the greatest good to the greatest number, which includes providing palliative/compassionate care. In cases of severe scarcity, the sickest victims who require intensive rescue resources may no longer be assigned first priority (see Casagrande et alReference Casagrande, Wills and Kramer8 and Coleman et alReference Coleman, Weinstock and Casagrande9).
The standards of care that are available to victims will be affected by resource scarcity. It is expected that at least initially in nearby locations the provision of care may need to change from conventional to contingency (functionally equivalent) to crisis for some period of time.21 Each institution should have a plan in place to determine when and how it will transition from normal or conventional triage guidelines and standards of care. It is crucial that these decisions be made by senior management and the reasons be communicated promptly and effectively to staff and the public. This will help to minimize chaos, inconsistency, and excessive stress in decision making, and to ensure adequate liability protections for practitioners.
It is essential that victims be reassessed and retriaged iteratively because resource adequacy may change rapidly over time. It is expected that facilities close to ground zero will experience marked resource limits initially, followed by subsequent improvement, as assets begin to arrive after 24 to 48 hours.
Background information and triage tools for use in a scarce resource setting can be found in the other articles in this issueReference Coleman, Knebel and Hick6Reference Knebel, Coleman and Cliffer7Reference Casagrande, Wills and Kramer8Reference Coleman, Weinstock and Casagrande9Reference Hick, Weinstock and Coleman10Reference Caro, DeRenzo and Coleman11Reference Sherman12Reference Dodgen, Norwood and Becker13Reference DiCarlo, Maher and Hick14 and on the REMM Web site. Planners and responders should consult these resources in advance to be able to implement their plans effectively and efficiently.
Venues for Medical Response
The radiation treatment, triage, and transport system (RTR system)Reference Hrdina, Coleman and Bogucki22 presents a functional approach to the various activities of the medical response (detailed information about the RTR structure is included in the electronic version of the Playbook).
The following list illustrates the various kinds of activities and where they would likely be located in relation to the zones of response noted above and regional assets.
• Phase 0: Preincident: Preparation (and possible ramp up based on intelligence, although there may be no notice for a terrorist event like an IND detonation)
• Phase I: Early phase: 0 to 24 hours
• Phase II: Intermediate phase: 24 to 96 hours (in addition to ongoing 24 hours starting in Phase I)
• Phase III: Later phase: >96 hours
There will likely be multiple RTR 1, 2, and 3 sites, each with different types of activities. Using this terminology allows responders to collaborate using common language for situational awareness, deployment or resources, and planning.
The medical response after a nuclear detonation requires the identification of assembly centers and medical care centers that are equipped to handle medical surge and have the ability to assess where the damage zones are located relative to the assembly centers and medical care sites. The medical response is organized following the RTR system and MedMap.23
Response Actions/Issues and Information Resources
Table 1 is adapted for this article from the DHHS IND Playbook. It lists selected tasks and issues for the Phase 0: preincident phase. Phases I through III will be on or linked to the REMM Web site.
TABLE 1 Action Steps/Issues Emergency Support Function-8: Preincident Preparedness Activities for a Nuclear Detonation
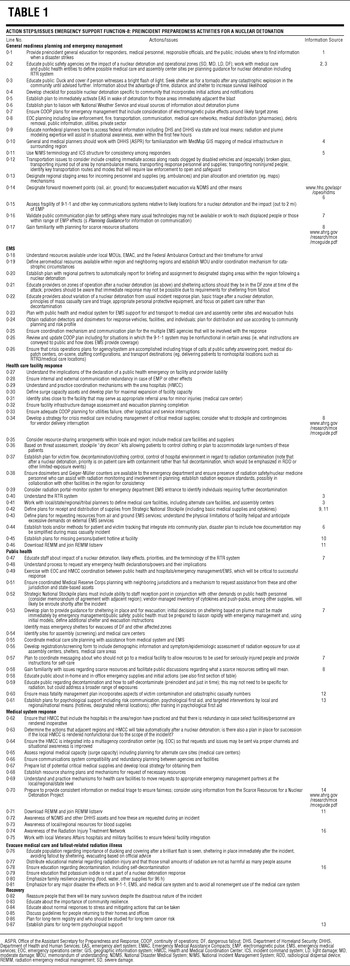
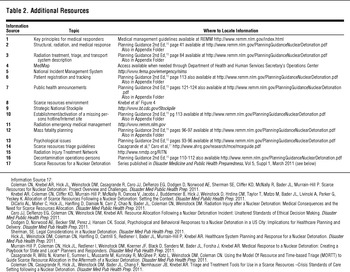
Table 2 provides additional information resources that inform the activities of the medical response. These resources help responders to know where to find the background documents supporting administrative and medical activities.
TABLE 2 Additional Resources
Author Disclosures: The author reports no conflicts of interest.
Acknowledgment: The authors acknowledge the contribution of Alicia Livinski, biomedical librarian, National Institutes of Health Library, for assistance with the preparation of this manuscript.





