The use of head-mounted virtual reality (VR) devices has revolutionized simulation-based learning in health professions education.Reference Barteit, Lanfermann and Bärnighausen 1 , Reference Kyaw, Saxena and Posadzki 2 These advanced devices are wearable as a headset, and immerse the student in a world where knowledge and practice blend seamlessly.Reference Jiang, Vimalesvaran and Wang 3 The hands-on nature of these simulations, guided by intuitive VR controls, provides a tactile understanding of medical procedures and scenarios. Thus, the individual learning experience is enhanced, which helps students prepare for real-world practice.Reference Tudor Car, Kyaw and Teo 4
Head-mounted VR devices are well suited to training for radiation emergency medicine preparedness.Reference Veenema, Lavin and Schneider-Firestone 5 Traditional on-the-job training is limited for radiation emergency scenarios due to the infrequency and unpredictability of such events.Reference Dallas, Klein and Lehman 8 , Reference DiCarlo, Homer and Coleman 9 VR technology addresses these challenges by providing a controlled, immersive environment in which medical trainees can systematically develop and improve their emergency response and preparedness skills.Reference Kyaw, Saxena and Posadzki 2 In a virtual space, the trainees can engage in lifelike simulations that replicate various scenarios.Reference Jiang, Vimalesvaran and Wang3 These simulations not only allow for repeated practice of critical procedures, but also provide a platform for examining decision-making skills under the pressure of a crisis.Reference Tudor Car, Kyaw and Teo4, Reference Veenema, Lavin and Schneider-Firestone 5 Previous studies have suggested that VR simulation training enhances medical students’ readiness for subsequent clinical exposure and improves their clinical performance in real-world situations.Reference Zackoff, Real and Sahay 6 , Reference Birrenbach, Zbinden and Papagiannakis 7 By using VR for radiation disaster preparedness training, trainees can develop a heightened sense of preparedness, confidence, and competence in dealing with the unpredictable and high-stakes nature of emergency situations.
In the field of medical education in Japan, a critical emphasis is placed on teaching radiation exposure medicine because of its critical importance in the aftermath of natural disasters. The Great Tohoku Earthquake is a poignant reminder of the need for health professionals to have specialized knowledge and skills in managing the health effects of radiation exposure.Reference Akashi, Kumagaya and Kondo 10 It has been reported that inadequate knowledge of radiation medicine and misunderstanding of radiation exposure among health professionals may have led to a shortage of specialized personnel able to provide medical care to patients and residents in the Fukushima nuclear power plant area.Reference Vano, Ohno and Cousins 11 , Reference Akabayashi, Takimoto and Hayashi 12 Therefore, Japanese radiation medicine stakeholders developed a well-structured radiation emergency medicine training curriculum after the Great Tohoku Earthquake; however, the training has been implemented in a limited number of undergraduate and postgraduate programs in schools with experienced faculties.Reference Ohtsuru, Tanigawa and Kumagai 13 , Reference Yasui, Kimura and Kamiya 14 Educating medical students in the intricacies of assessing and responding to the health challenges posed by radiation exposure is essential to ensuring a prepared and resilient health care workforce. However, teaching radiation medicine to medical students presents significant challenges, primarily due to the complex and resource-intensive nature of the subject. The lack of comprehensive educational resources, including realistic simulations, specialized training facilities, and experienced faculty, is a significant barrier. Given the multifaceted aspects of radiation emergency medicine, there is an urgent need for increased investment in diverse and tailored VR tools that can effectively prepare medical students for the unique challenges associated with emergency crisis situations.Reference Tomisawa, In and Ota 15
The emotions of health professional trainees have recently been recognized as important indicators of outcome in medical simulation research, including in VR-based trainings. In addition, the control value theory of achievement emotion works is considered the paramount framework for interpreting the emotions of medical trainees learning to deal with critical situations in simulation trainings. Therefore, the aim of this study is to evaluate the effectiveness of a head-mounted VR tool for teaching basic radiation emergency medicine skills to medical students.
Methods
Study Design and Learning Context
We conducted a virtual simulation study using head-mounted VR devices (Meta Quest 2, also known as Oculus Quest 2) along with an application designed to teach radiation emergency medicine to medical trainees. Obtaining radiation measurements in the conventional manner requires precise (and expensive) instruments. To address this limitation while also providing an intuitive learning experience for the trainees, the application enables visualization of the invisible radiation and progresses to identification of contaminated areas.
The NUP: RI Survey application developed by the authors was used in the present study (Figure 1). Using the application, trainees learn measurement procedures using a Geiger–Müeller survey meter and practice identifying contaminated areas displayed in VR.Reference Tomisawa, Hosokawa and Kudo 16 –Reference Tomisawa, Osanai and Hosokawa 18 In an integrated 3-step process, trainees search for contaminated areas by selecting appropriate settings, identifying these areas, and inputting the measured radiation levels. This method of training overcomes the limitations of traditional methods and enhances learning effectiveness by enabling trainees to visualize and experience simulated real-world scenarios.

Figure 1. Example image from the NUP: RI Survey application.
Participants
The participants were fifth-year medical students at Hirosaki University, Japan, who were on clinical rotation training at the emergency department during the study period (June 2022–December 2022). Sixty-four students underwent a 3-hour training session in radiation emergency medicine delivered via head-mounted VR devices. They completed a self-reported online survey just before starting the session and again after completion of the session.
Data collection
Measurement of emotions
All participants completed the Japanese version of the J-MES, a Japanese translation of the Medical Emotion Scale originally developed in English.Reference Nomura, Wiseman and Sunohara 19 The J-MES includes 20 items containing adjectives describing discrete emotions, which the user scores using a 5-point Likert scale (Figure 2). The items are categorized into subscales according to the valence (positive/negative) and arousal level (activating/deactivating) of the emotions: (a) positively activating (e.g., hope, joy); (b) positively deactivating (e.g., relaxed, relieved); (c) negatively activating (e.g., anger, anxiety), (d) negatively deactivating (e.g., sadness, boredom), or (e) neutral (i.e., surprise) (Figure 3). In addition, the “during” J-MES questionnaire was administered immediately after the session to prevent interference with the task.

Figure 2. The 20 items of the Medical Emotion Scale.
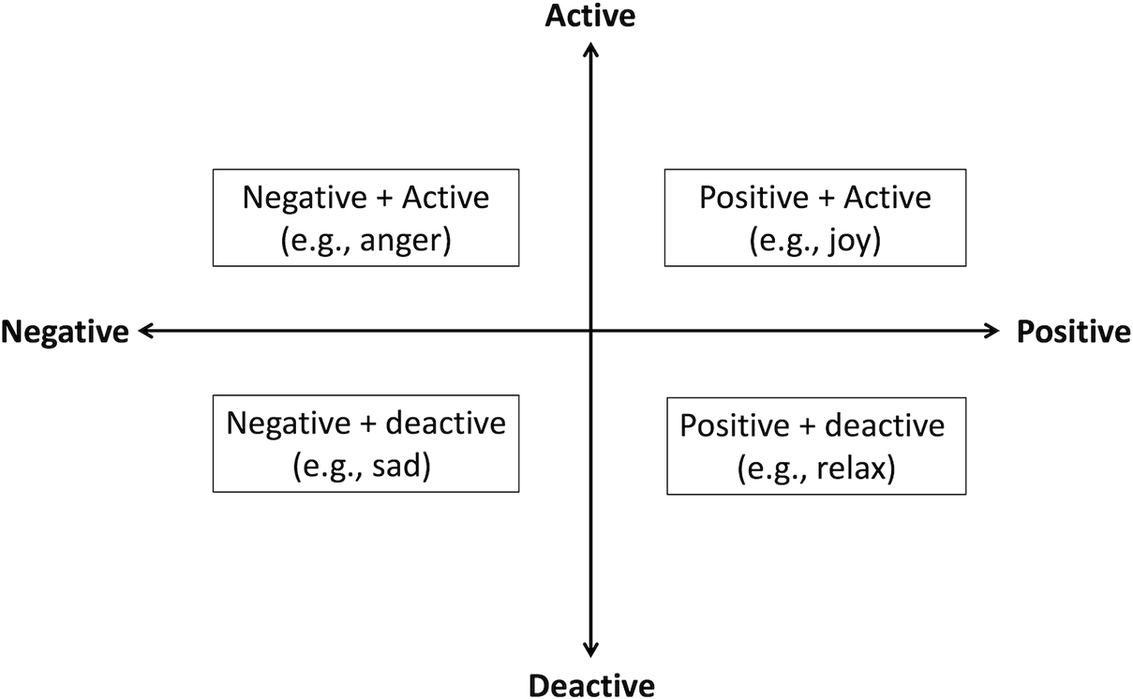
Figure 3. Subscale categories of the Medical Emotion Scale.
Post-task self-performance
Perceived self-performance was evaluated using a 5-point Likert scale (1 = very poor, 5 = excellent).
Post-task self-efficacy
Post-task self-efficacy was assessed after task completion using a single item adapted from Bandura’s scale to measure participants’ confidence when performing a similar task in the future. Confidence levels were measured using a 100-point Likert scale (0 = no confidence to 100 = complete confidence) with 10-point intervals.Reference Bandura, Pajares and Urdan 20 , Reference Mori, Nomura and Takei 21
Data analysis
Medians with 25–75 percentiles were calculated for continuous variables. Friedman’s test was used to compare scores before, during, and after virtual simulation study. We initially conducted Friedman’s test for repeated comparison across these 3 time points. Post-hoc Bonferroni test was then carried out for comparison of scores at the three time points (before, during, and after). These analyses were then stratified according to median performance and self-efficacy scores. A P value < 0.05 was considered statistically significant. All analyses were performed using R software (version 4.3.0).
Ethics
The study protocol was reviewed and approved by the Ethics Committee of Hirosaki University Graduate School of Health Sciences (approval No. 2021-033). Written informed consent was obtained from all participants.
Results
Table 1 lists the descriptive statistics of the participants. The median (25–75 percentiles) performance and self-efficacy scores were 4 (3–4) and 60 (45–65), respectively. Negative activating emotions (P < 0.001), negative deactivating emotions (P = 0.004), and neutral emotions (P = 0.011) were significantly different across the three time points. The post-hoc test revealed significant differences in negative activating emotions between before and during (P < 0.05), and between before and after (P < 0.05) the VR simulation. In addition, negative deactivation and neutral emotions were different before and after the simulation.
Table 1. Participants’ demographics (n=59)
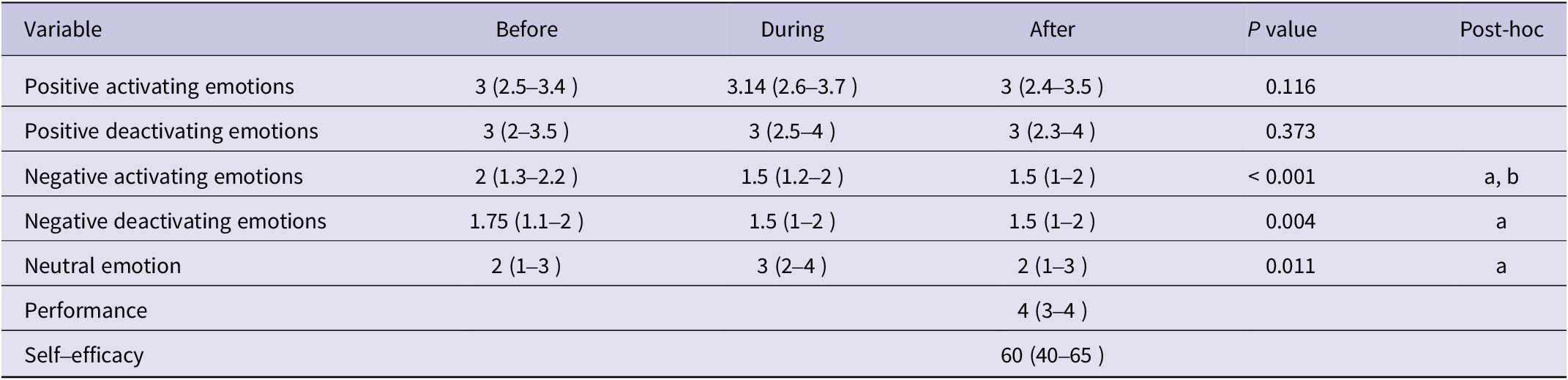
Data are presented as the median (25–75 percentiles).
P values were calculated using Friedman’s test.
Post-hoc Bonferroni correction was conducted for the results of Wilcoxon signed-rank test for the comparisons (a) before–during and (b) before–after.
Table 2 shows the change in each factor over time according to stratified self-performance score. Negative activating emotions (P < 0.001), negative deactivating emotions (P = 0.006), and neutral emotion (P = 0.036) were significantly different across the time points in the high self-performance group. The post-hoc test revealed significant differences in negative activating emotions between before and during (P < 0.05), and before and after (P < 0.05) the VR simulation. Similarly, a significant difference between the before and during scores was found for negative deactivating emotions. Although no significant significance was noted, positive deactivating emotions increased slightly between before and after the VR training.
Table 2. Survey scores at each time point according to performance group
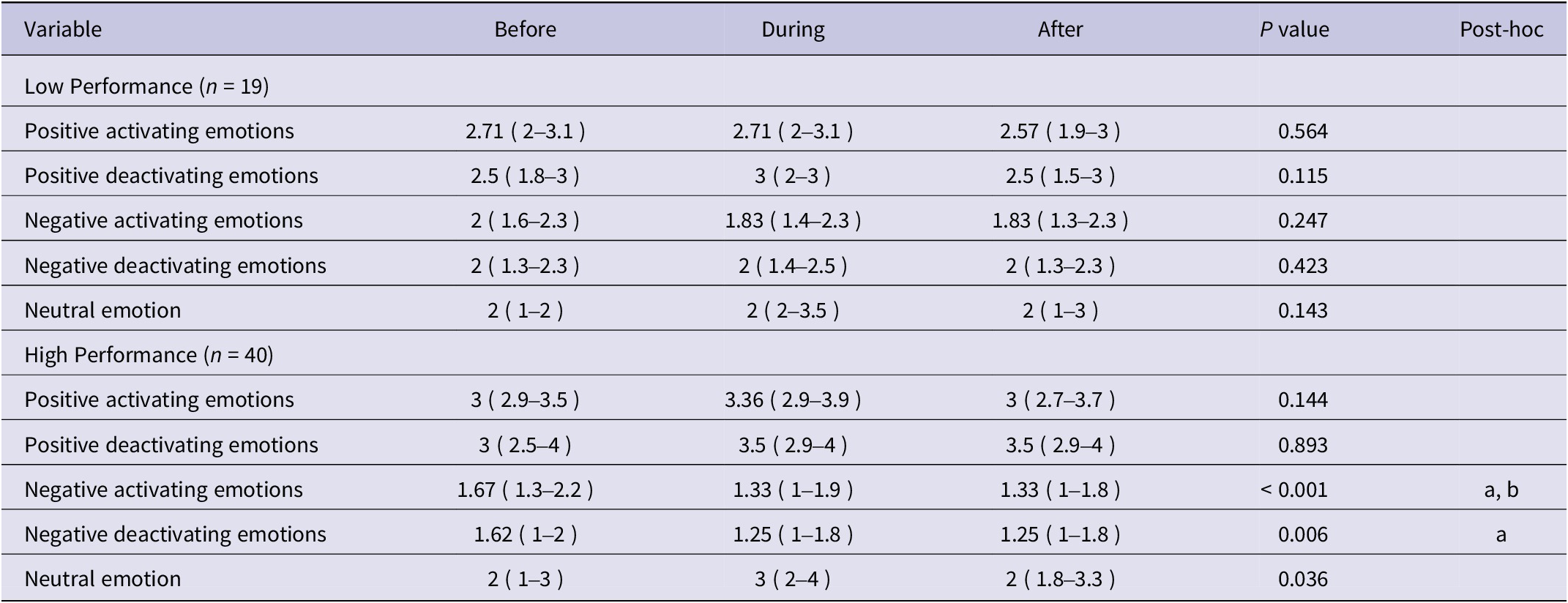
Data are presented as the median (25–75 percentiles).
P values were calculated using Friedman’s test.
Post-hoc Bonferroni correction for the results of Wilcoxon signed-rank test was conducted for the comparisons (a) before–during and (b) before–after.
Table 3 shows the change in each factor over time, stratified by self-efficacy score. Among participants with low self-efficacy (low self-efficacy group), there were significant significances in negative activating (P = 0.011) and deactivating (P = 0.035) emotions. Among participants with high self-efficacy (high self-efficacy group), a significant difference was found in negative activating emotions (P = 0.001). The post-hoc test revealed significant differences between the before and after scores for negatively activating emotions in both of the self-efficacy score groups (P < 0.05). Although no significant significance was noted, positive deactivating emotions increased slightly between before and after the VR training.
Table 3. Survey scores at each time point according to efficacy group
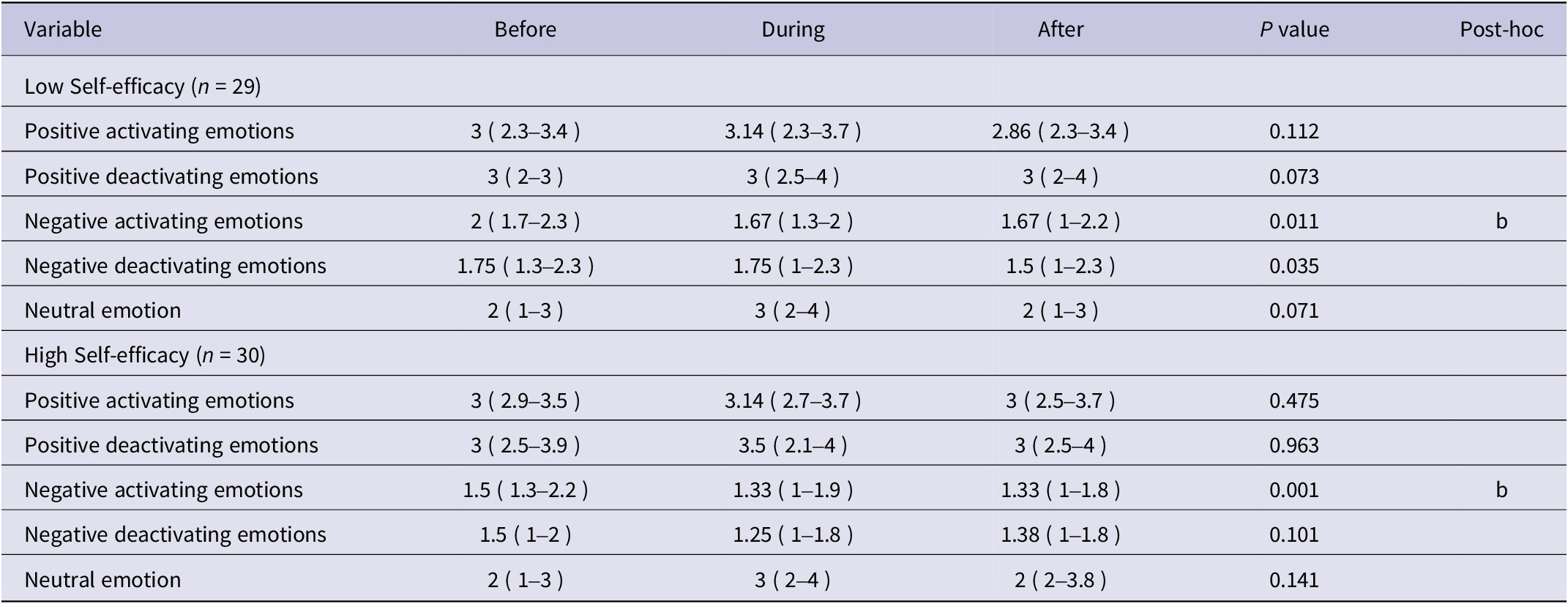
Data are presented as the median (25–75 percentiles).
P values were calculated using Friedman’s test.
Post-hoc Bonferroni correction for the results of Wilcoxon signed-rank test was conducted for the comparisons (b) before–after.
Discussion
To the best of our knowledge, the present study is the first to investigate the effect of using head-mounted VR devices on emotional change in medical students taking part in radiation emergency medicine training. Compared with those before the sessions, scores for the emotion of surprise (i.e., neutral emotion) increased and those for negative emotions decreased after the sessions. In addition, the high-performance group showed slightly higher positive emotions during the VR training sessions than those perceived before the sessions and successfully reduced negative emotions after the session started.
According to the control value theory of achievement emotions, emotions act as a predictor of learners’ performance in their training.Reference Pekrun 22 Specifically, positive emotions can improve medical students’ performance, whereas negative emotions have a negative impact on their learning. Previous reports have suggested that surprise is a neutral emotion that can be either positive or negative depending on the learning situation.Reference Pekrun 22 For example, a learner might experience positive surprise when they receive an award for an excellent achievement, but the same learner might experience negative surprise when their mark is lower than expected. Therefore, to analyze the function of the surprise element in a given learning context, it is useful to examine the pattern of change in other positive and negative emotions. In other words, for the current learning context of head-mounted VR simulation, the change in pattern for the surprise item was synchronized with an increase in positive emotions, i.e., both positive emotions and surprise showed increases between the pre survey and the post survey.
In the high-performance group, the pattern of emotional change was consistent with the control value theory. Namely, positive emotions increased and negative emotions decreased after the start of the VR simulation session in the high performers, which indicates that these emotions might have promoted learning performance in the VR training. From the perspective of emotional regulation in the medical field, this finding may provide valuable insights into the impact of VR simulation training on improving trainees’ performance in real-world contexts. Emotion regulation, such as increasing positive emotions and decreasing negative emotions, is one of the vital skills required for health care professionals and trainees who work or will work in critical situations.Reference Tamir, Ito and Miyamoto 23 Thus, the students in the current study experienced the process of effective emotion regulation using head-mounted VR devices and may have learned how to regulate their emotions in such situations. When making critical decisions, effective self-management and emotional regulation are crucial skills that can help prevent subsequent mental illness among health professionals.Reference Dionne, Gooty and Yammarino 24 The present study showed that the use of head-mounted VR was effective in modulating medical students’ emotions, which in turn contributed to improving their self-confidence in radiation emergency medicine, and potentially facilitated their readiness to respond to the challenges associated with emergency crisis situations.
This study has several limitations. First, there is a risk of type II error due to the small sample size, and we did not calculate a required sample size for this study because there are no previous studies on VR simulation using the Medical Emotion Scale. Second, we assessed and compared only emotion variables and did not compare other outcome variables such as self-performance and self-efficacy due to possible reporting bias. Third, this is a single-arm design without a control group and the effect of VR training on medical students’ performance were not examined in a real-world situation; therefore, the design of this study is not robust enough to provide strong evidence. Nevertheless, the current study provides new evidence on the emotional outcomes of VR simulation for medical students. Further studies with larger samples, more robust design, and multiple variables are needed to address these limitations.
Conclusions
Use of head-mounted VR devices during training in radiation emergency medicine had the effect of modulating medical students’ emotions and contributed to improvements in their perceived performance.
Acknowledgements
We are greatly indebted to all of the medical students who participated in this survey and to Kotetsu Tanaka, RN., Daishi Sato, RN., Misato Kasai, RN., Junko Mikami, RN., and Ms. Rumiko Narita for their support in data collection and Ms. Sayaka Susuta for her manuscript preparation.
The English-language editing of this manuscript was conducted primarily using Chat GTP 3.0 and DeepL Write. A native-English-speaking professional editor has proofread the final English version of the manuscript.
Author contribution
Conceptualization, O.N.; methodology, M.O. and S.H.; formal analysis, Y.S.; investigation, O.N. and Y.I.; data curation, O.N. and T.T; writing—original draft preparation, O.N. and Y.S.; writing—review and editing, T.T. and K.I.; supervision, H.H. and T.T; project administration, O.N.; funding acquisition, O.N., H.T. and T.T. All the authors have read and agreed to the published version of the manuscript.
Funding statement
This work is supported by the Toyota Foundation 2021 Co-Creating New Society with Advanced Technologies (Project: Creating an “Emotion Mobile Laboratory” for Preventing Burnout of Health Professionals, D21-ST-0003) to Osamu Nomura.
Competing interest
This research project was also supported by the Tohoku Initiative for Fostering Global Researchers for Interdisciplinary Sciences (TI-FRIS) of the MEXT Strategic Professional Development Program for Young Researchers.








