Introduction
During Major Incidents and Disasters (MID) and with the increasing myriad of crises such as epidemics, pandemics, war, and conflict, civilian hospitals are expected to be functional, receive, and manage victims with a variety of injuries as well as continue the local and referral population in need of emergency or non-emergency care. Reference Stander, Wallis and Smith1-Reference Khorram-Manesh, Angthong and Pangma3 A major aim of a hospital disaster plan is to provide professional and material resources to receive as many victims as possible from the affected area, and by targeting all 4 elements of the surge capacity, i.e., Staff, Stuff, Structures, and Systems. Reference Barbisch and Koenig4-Reference Verheul and Dückers6 As the response chain to MID consists of many units, the interaction between these entities at all levels may proceed more efficiently with a central coordination center. Reference Khorram-Manesh, Hedelin and Örtenwall7 These coordinated actions between collaborating partners create the foundation for a plan, which should be tested and validated before MID. Reference Khorram-Manesh, Berlin and Carlström8
In recent years, it has become clear that hospitals may be the targets of both natural and man-made MID. Reference Bagaria, Heggie, Abrahams and Murray9-Reference De Cauwer, Somville and Sabbe31 Vulnerabilities of a medical facility/hospital vary between countries due to the type of event and the geographical conditions. In some countries, e.g., South American countries, more than 50% of healthcare facilities (hospitals and primary care) are in high-risk areas for natural disasters. In comparison, the figure is much lower (8-9%) for other countries such as the United Kingdom. Several potential events such as hurricanes, earthquakes, floods, landslides, tornados, storms, volcanos, cyclones, tsunamis, fires, explosions, CBRN (Chemicals, Biological, Radionuclide threats), cyberterrorism, terrorism, armed attacks and bombings, as well as rapidly changing technological issues within hospital infrastructure can result in a mandatory hospital evacuation. Reference Khorram-Manesh, Angthong and Pangma3,Reference Bagaria, Heggie, Abrahams and Murray9-Reference De Cauwer, Somville and Sabbe31 Some factors such as increasing population numbers and density, rapid unsustainable urbanization, biodiversity losses, and climate changes may complicate the outcome of these events. Indeed, the latter changes are increasingly accelerating infectious disease outbreaks, epidemics, and pandemics. Reference Haines, Kovats and Campbell-Lendrum32 Although each event may have a particular impact on a hospital, it affects either hospitals ‘structural’ or ‘non-structural’ components and, consequently, its functionality. According to the Sendai Framework for Disaster Risk Reduction 2015-2030, substantial reduction of disaster damage to critical infrastructure and disruption of basic services should take place globally. Healthcare and educational facilities are particularly encouraged to develop their resilience by 2030. Although a hospital evacuation might be unavoidable, planning for hospital evacuation will make it more resilient during the future events. 33
Compared to a disaster plan, a hospital evacuation plan has a reverse pattern, i.e., instead of creating more space and surging capacity within the hospital, all patients should be evacuated and transported to other areas or medical facilities to receive continuous care. An evacuation does not need to be total and patients might be sheltered in place, evacuated horizontally or vertically, within the same hospital. However, although rare, whenever a decision for total evacuation is made, the situation will be more complicated and the task more complex. An extensive/total evacuation of a hospital is associated with several medical and non-medical difficulties such as insufficient internal and external logistics, lack of routine for tracking patients, diverse ethical issues, as well as unattended injury or deaths to patients and staff alike during evacuation. Reference Khorram-Manesh, Angthong and Pangma3,34-38
There is conceptual confusion in available literature about the word ‘EVACUATION,’ which is used to describe the need to transfer, move, or drain materials, equipment, or people from an existing building. Many languages may have different words for evacuation with a different meaning, e.g., ‘EXIT’ and ‘EVACUATION.’ The former correctly indicates the need for time-limited escape from danger (e.g., fire). The term ‘EVACUATION’ might then mean a need for the exit, transport, and final placement in another facility. Reference Wapling, Heggie, Murray, Bagaria and Philpot13 Such a situation may take a longer time and have a higher impact on patients’ health and outcome. In this report, we aim to study the result of total evacuation. The aim of this paper is 2 fold:
1) To determine the significant difficulties in the management of hospital evacuation through a review of the literature.
2) To confirm the current readiness for evacuation among some European and non-European countries.
Methods
Review
This study consists of 2 steps. In the first step, a systematic review of the subject matter, according to the PRISMA flow diagram was performed. Reference Moher, Liberati, Tetzlaff and Altman39 Using Scopus, PubMed, and Gothenburg University´s search engine, the following keywords were used to review the current and related literature about hospital evacuation. The terms ‘hospital evacuation’ or ‘healthcare facilities’ and ‘evacuation’ were searched as MeSH (Medical Subject Heading) terms alone or in combination. Obtained articles were manually searched. Inclusion criteria were articles in English describing evacuations between January 1995 and February 2020. Partial evacuations, healthcare facilities not identifiable as a hospital, and narrative reports were excluded. Figure 1 shows the process of search according to the PRISMA flow diagram. Reference Moher, Liberati, Tetzlaff and Altman39

Figure 1. Systematic review of the subject matter, according to the PRISMA flow diagram.
Questionnaire
The main author (AK) assembled a group of 3 independent professionals (1 physician, 1 hospital nurse, and 1 prehospital nurse, not included as authors), all academically and clinically active within the hospital and prehospital preparedness and disaster management. AK performed the literature review, and presented the results in 3 different rounds, based on the Nominal Group Technique. Reference Harvey and Holmes40 In the first round, a list of obtained documents was presented by AK, and the group agreed on the literature which should be included for further evaluation. In the second round, the abstracts of chosen literature were presented and literature for the in-depth study was chosen. Finally, in the third round, 2 members of the group studied the selected documents and presented their findings to the whole group. These findings were then sorted and inserted in Table 1. Together, the group summarized these findings into 10 statements/questions based on qualitative saturation of thematic areas. A qualitative content analysis of the manifest content was performed manually by 1 of the authors (EC). Reference Sandelowski41,Reference Graneheim and Lundman42 First the thematic contents were identified and then condensed into core contents. At a point where no new novel information was extracted from the data, the statements were outlined. Question, number 11, was added to provide all participants a possibility to comment/add other items needed. The questions were sent to 20 professionals, representing 15 different countries in the second step. The respondents (physicians, nurses, or PhDs educated and actively involved in MID management), were asked to answer the questionnaire individually or in collaboration with the responsible units in their countries. Respondents participated voluntarily and were recruited either by showing a direct interest in the topic or indirectly by being recommended as researchers registered in ResearchGate, a European social networking site for scientists and researchers, which is the largest European academic network in terms of active users. Scientists and researchers share papers, ask and answer questions, and find research collaborators. Reference Nicholas, Clark and Herman43 The questions were;
1) Incident Command System is a vital element in the successful management of MID. It is especially essential to see whether various countries have collaboration between hospitals and a management/coordination center. In this perspective, the role of private hospitals should be explored.
a) Central command vs. independent hospital
b) Plans for surge capacity
c) The role of private hospitals
2) Communications, collaboration, coordination with other agencies are attractive measures in all levels of action, including the private sector.
a) Different managerial levels
b) Private organizations
3) Ethical perspectives of hospital evacuation are directly related to the decision-making process and information delivery, information sharing. How transparent are decisions? How aware are staff and the public? Are there any guidelines/protocols?
a) Awareness of difficult medical decision-making
b) Who makes the final decision (Administrators, Medical Staff, combination, etc.?)
c) Staff and public awareness
d) Any guidelines?
4) Legal perspectives on hospital evacuation may put different agencies in different zones and create difficulties in collaboration between various agencies? How to act? How to respect duties and responsibilities vs. willingness to work?
a) Multi-agencies?
b) Guidelines?
5) An internal logistics plan is a prominent issue to follow regarding internal resource management.
a) Staff
b) Stuff
6) An external logistics plan is a prominent issue correlated with resource utilization.
a) Central dispatch
b) Reserve staff and stuff
c) Ability to move staff, sending stuff
d) Known receiving-hospitals/facilities and whether they are electronically compatible and easily transferable within your system.
7) The lack of specific plans for vulnerable groups may have a significant impact on the outcome.
8) Insufficient or absence of procedures for removing critically sick patients, e.g., ICU patients, is an obstacle.
9) Knowledge about reverse triage/triage (The evacuation triage algorithm uses mobility and dependency to determine the evacuation triage priority, categorizing patients into the groups; Very Dependent, Dependent, and Independent. Independent patients evacuating first)34,35 is decisive in resource utilization and survival outcome.
10) Training and exercise is a parameter always written but never performed.
11) Any comments/missing issues or subjects.
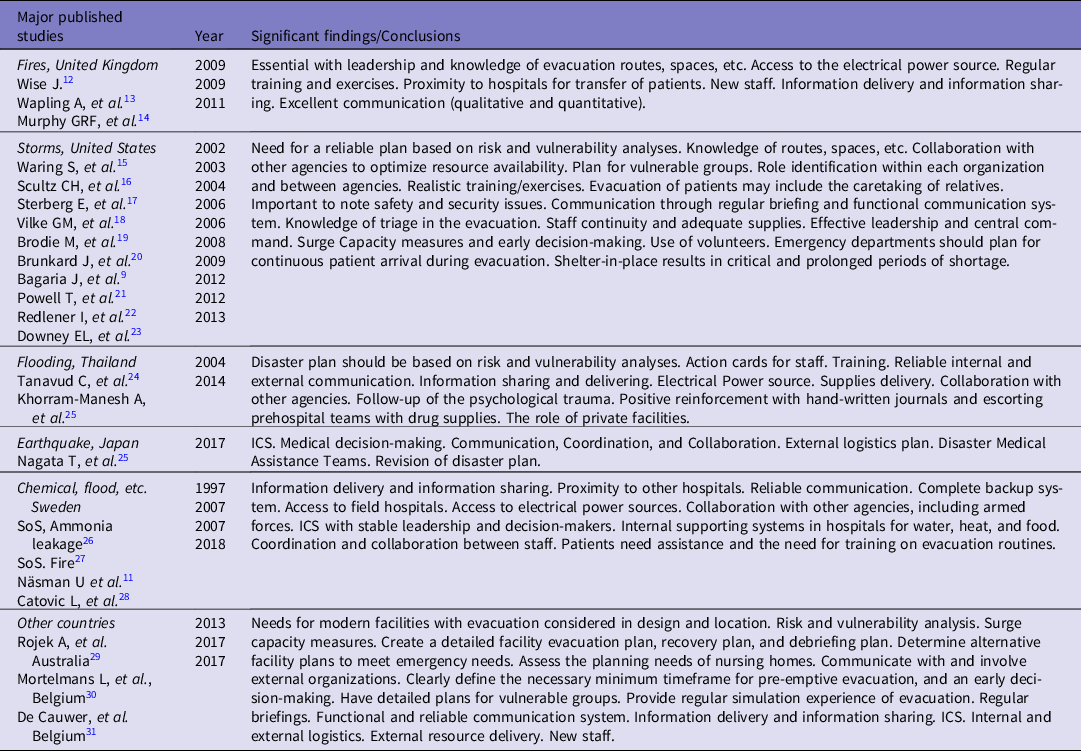
Table 1. Findings/notions from historical evacuation incidents and some simulation exercises. The results are grouped based on the notions, type of disaster, and country of publication
The first 10 questions could be organized as; Command and Control, Ethical and legal perspectives of hospital evacuation, Logistics, Systems-rules-guidelines, Training, and exercises.
Results
Literature Review
Table 1 presents the summary of the findings from the systematic literature review, presented as significant findings or lessons learned, based on studies from 1997-2018. Reference Khorram-Manesh, Angthong and Pangma3,Reference Bagaria, Heggie, Abrahams and Murray9-Reference De Cauwer, Somville and Sabbe31 The results were grouped after the country of publication and thematically. they covered: 1) The importance of leadership, and the difficulties and lack of awareness in medical decision-making and its medical, ethical and, legal consequences, 2) Unprepared and untrained command and control, 3) The lack of proper communication, and 4) The shortcoming in logistics planning. Table 1 was not presented to the respondents.
Questionnaire
Representatives of 15 countries: Belgium (MD), Croatia (MD), Germany (MD), Iran (MD and PhD), Italy (MD), Netherlands (PhD), Norway (PhD), Philippines (2 MDs), Poland (PhD), Portugal (MD), Saudi Arabia (PhD), Sweden (MD, and PhD), Switzerland (MD), Thailand (MD), and UK (MD) received the questions. A total of 18 (out of 20 = 90%) professionals from 13 (out of 15 = 87%) countries replied. Although 2 more requests were sent to the representatives of Croatia and Germany, they did not respond due to the lack of time. The answers obtained by all countries included in this study are summarized and presented in Tables 2-7 (ICS, C3, and ethics in Tables 2 and 3; legal and logistics in Tables 4 and 5; vulnerable groups and triage in Tables 6 and 7).
Table 2. Presence of Incident Command System (ICS) regarding hospital evacuation in 10 countries. (NSE=Not specifically for Hospital Evacuation, OP=Own Plan)

Table 3. The status of inter-organizational collaboration, coordination, and communication (C3), and ethical perspectives, regarding hospital evacuation in 10 countries. (NSE=Not specifically for Hospital Evacuation)

Table 4. The status of legal perspectives of hospital evacuation in 10 countries (NSE = Not specifically for Hospital Evacuation, RD = Red Cross, CD = Civil Defense)
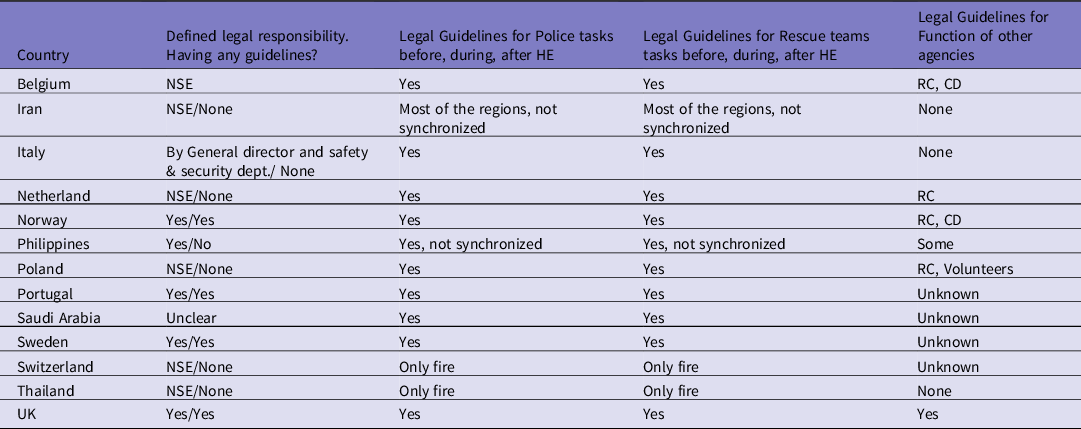
Table 5. The status of internal and external logistic plans regarding hospital evacuation in 10 countries (NSE = Not specifically for Hospital Evacuation, RC = Red Cross)

Note: Central dispatch refers to ambulances being dispatch by a central center. HR management plan refers to extra staff that can be available in the short and long-term. Plan to move devices refer to moving critical equipment such as ventilators. Reference Nagata, Himeno and Himeno25 Sending medication refers to ‘send 7-10 days of ordinary medication to the receiving hospital and concern cancer patients or those having rare diseases.
Table 6. The management of vulnerable groups, including critically sick patients, regarding hospital evacuation in 10 countries
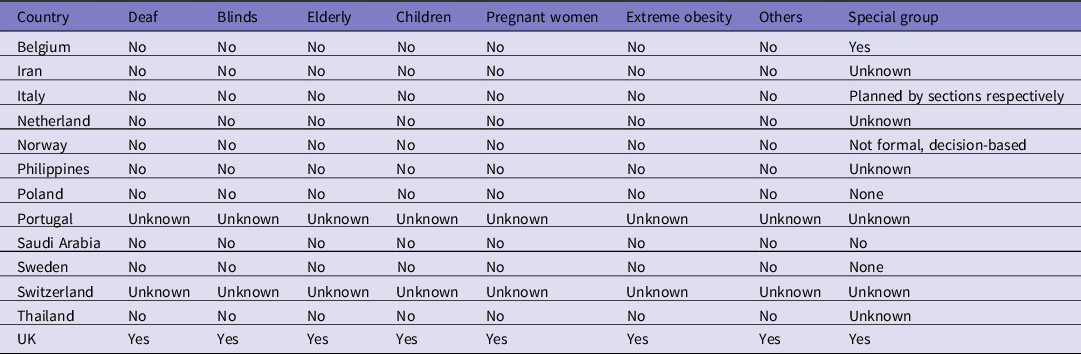
Note: The Participants answered that there is a general lack of planning to evacuate vulnerable groups, especially critically sick patients (Special groups; critically sick patients, e.g., ICU patients, patients under surgery, patients treated for cancer).
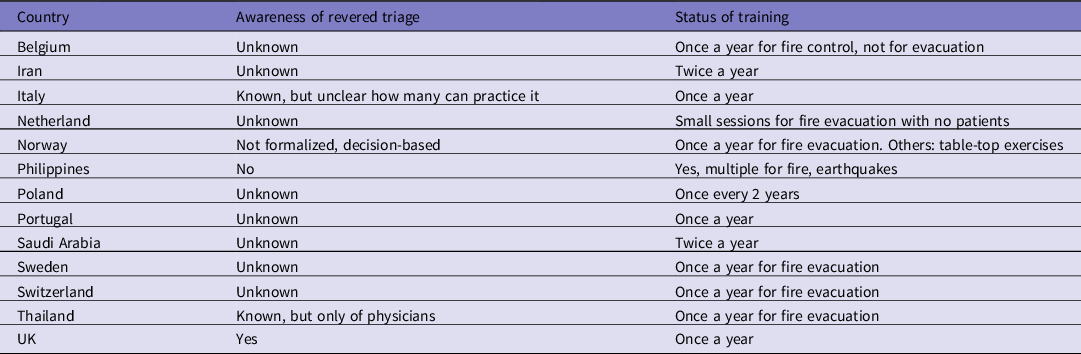
Table 7. The awareness of reversed triage (to identify patients least in need of urgent treatment to free up beds during surge demand), and the status of training and exercises, regarding hospital evacuation in 10 countries
According to the participants, all countries have ICS in which hospitals are independent but in collaboration with a central command. Most of the hospitals have a plan for surge capacity, but not specifically for hospital evacuation. In most countries, private hospitals have their own disaster and evacuation plans (unclear in 4 countries, Table 2). However, the content of the plan was not available. Collaboration, coordination, and communication did exist at all managerial levels, both in hospitals and with other agencies outside the hospital. However, collaboration with private hospitals and their managerial levels was not fully functional (Table 3). There was insufficient information about ethical awareness and difficulties in medical decision-making as public hospitals especially seemed to lack enough knowledge about the imbalance between resources and needs and the necessity for critical decision-making. There were no examples of ethical guidelines for the staff and decision-makers (Table 3). It appeared that the legal perspectives of hospital evacuation followed those needed for disaster management in general (Table 4). There were some Non-Governmental Organizations (NGOs), such as Red Cross/Crescent, available in all countries. However, the relation between these organizations with the disaster management authorities and their designated role within the nation’s disaster management system was not clear (Table 4).
Most of the participant countries seemed to have internal logistic plans for staff and stuff, external logistic plans, and a central dispatch center. They had reserved vehicles, but not any specific pool of personnel. They had no plans to move staff and equipment. Half of them had predetermined receiving hospitals (Table 5). In critical situations, such as in patients with cancers or very rare diseases, whether patients’ medications were sent with them or not, were unclear or unknown. Most countries did not have any procedures for evacuation of vulnerable groups. Only the United Kingdom seemed to have plans for vulnerable groups. Some other countries had plans for elderly, pregnant women and children. Plans for blind and deaf individuals were missing (Table 6). The principles of reverse triage, i.e., to categorize patients in Very Dependent, Dependent, and Independent, were unknown or not implemented. Some countries with strong religious beliefs referred to their spiritual responsibilities. According to their religion, people have the same value and every individual has the responsibility to act morally and ethically, and treat other individual fairly as written in the holy book. However, they had no official documents, and it was not clear how people with other religious backgrounds might act. All participants, except 1, reported 1 exercise/year. Most of the exercises were fire evacuation, and no specific activity for evacuation was conducted (Table 7).
Discussion
A shortcoming revealed by this study is the lack of awareness of the untoward consequences of medical decision-making during an evacuation, which is very different from those taken in peacetime, and during the management of MID. Reference Khorram-Manesh, Angthong and Pangma3,Reference Kaji, Koenig and Bey5,Reference Khorram-Manesh, Berlin and Carlström8-Reference Nero, Örtenwall and Khorram-Manesh10,34,35 The medical decisions made during an evacuation do not only concern the quality of care, but rather, how the limited quantity of everything affects or guarantees the best outcome. Although today’s healthcare is under constant pressure to prioritize patients due to the economic strain, the ethical discussion about who is to be prioritized and why, is avoided. The consequences of various medical decision-making will be more difficult in MID and much more during an evacuation when 1 decision may indicate no treatment for a specific group of patients for the sake of the rest. Understanding this kind of reasoning can be difficult for staff and the public, and there is a major need to learn more about the determinants of the subject before any MID and hospital evacuation. Reference Khorram-Manesh, Angthong and Pangma3,Reference Nero, Örtenwall and Khorram-Manesh10,Reference Zane, Biddinger, Hassol, Rich, Gerber and DeAngelis36
Another important finding in this study is insufficient or defective planning for vulnerable groups, including very sick patients. Reference Khorram-Manesh, Yttermyr, Sörensson and Carlstrom44 The majority of hospitals have no planning for vulnerable groups or specific groups such as ICU patients or patients under surgery. These patients are all cases that might be left in place during an evacuation. Some countries may rely on triage to select the priority of the patients, and there are specific triage methods for evacuation (Healthcare Evacuation Reverse Triage Priorities), 34,35 which may ease up the process of selection. However, they usually are not practiced, nor are they widely known. Irrespective of the method for screening, these cases are far too challenging to move in an evacuation process and the decision of leaving them behind may trigger anger and confusion in people who are not aware of the situation, options, and difficulties emergency managers may have. Reference Khorram-Manesh, Angthong and Pangma3,34,35,Reference Khorram-Manesh45
Internal and external logistics are always a big issue in MID. Although several reports indicate a need for the development of external logistics, the internal logistics in the event of an evacuation is much more affected. Reference Khorram-Manesh, Angthong and Pangma3,Reference Nero, Örtenwall and Khorram-Manesh10,Reference Näsman, Zetterberg Randén and Brändström11 Experience has shown that in many cases, staff who have accompanied patients out of hospital may not get back. Reference Khorram-Manesh, Angthong and Pangma3 Simultaneously, it can be extremely difficult to receive new personnel to a hospital which is already under evacuation. Our study shows a good capacity for internal logistics in MID, yet such ability is unknown or defective in external logistics. Both actions need to be done smoothly. Internal logistics are more demanding in an evacuation, and more consideration should be given to better planning and training. External logistics, on the other hand, demand good collaboration with other entities, which might not be easy to achieve if these entities have not looked into possible ways of cooperation, research, and information sharing.
The Incident Command System has been mentioned as 1 of the significant factors for the successful management of MID. Reference Stander, Wallis and Smith1-Reference Khorram-Manesh, Angthong and Pangma3,Reference Khorram-Manesh, Hedelin and Örtenwall7,Reference Nero, Örtenwall and Khorram-Manesh10 Such a procedure enables the systematic management of an event based on experience and scientific sound guidelines. It also enables collaboration between hospitals and regional entities. In our survey, the majority of included countries had ICS, and the partnership between hospitals and local coordination centers was evident. The contribution and participation of private hospitals/medical facilities in the total preparedness system is a critical issue in many countries and needs to be settled in a way that gives both sides responsibilities but also benefits in their collaboration. The need for such engagement is revealed in the results of our survey in which the roles of private organizations and hospitals are very unclear and not synchronized. A significant way of achieving a good collaboration and rational resource and information sharing is interactive courses and exercises to identify each organization’s weaknesses and capabilities and the areas that can be coordinated and synchronized. Reference Khorram-Manesh, Berlin and Carlström8 The educational initiatives, exercises, and training methods enable all organizations to identify their limitations and capabilities. A significant benefit is to know and understand the legal responsibility of each emergency organization. Although the legal perspectives in MID seem to be well prepared and can also be used in an evacuation, it is essential to discuss all possible issues that may exist in an evacuation, and which may change the course of management and medical outcomes. Reference Goniewicz, Misztal-Okońska and Pawłowski46 Most of the guidelines concerning evacuation deal with short and less complicated cases of fire. Although many countries have legal guidelines that are associated with fire incidents, these guidelines need to be expanded to encompass long-term evacuation of a hospital with all issues it may have.
These results can conclude the need for exercise and training within the organization and in collaboration with others. Exercise and training are mentioned in the plans but are rarely conducted. Concerning an evacuation, they deal with short and temporary evacuation due to fires. Although such preparedness is proper, it is far from what is needed for a total evacuation of a large hospital and its consequences. Reference Khorram-Manesh, Angthong and Pangma3,Reference Khorram-Manesh, Berlin and Carlström8 An important factor in an evacuation is to clarify who makes the final decision to evacuate Reference Khorram-Manesh, Angthong and Pangma3,Reference Verheul and Dückers6,Reference Nero, Örtenwall and Khorram-Manesh10 ; is it the hospital administrator, the chief of medical services/nursing, chief of security, or a predetermined combination? Such a plan should consist of a list of people, who can make such a vital decision, if 1 or more of the decision makers are not available or incapacitated by the crisis event.
Limitations
The study is mainly based on English and in some cases, Swedish publications. Consequently, some important information published in other languages may have been missed in the review process. Nevertheless, the search was completed by the questionnaire, which was sent to representatives of 15 countries. Although the number of countries included might be low, the combination of the literature search and survey can give a good picture of the field internationally. However, it must be remembered that each participants has reported according to his/her total knowledge of hospital evacuation plan in their countries, and thus specific routines or plans from some hospitals might be missing. Another limitation might be the absence discussion on the recovery phase of the evacuation. However, since recovery is an important phase of the disaster management, it was not included in the discussion about hospital evacuation, which was our primary aim.
Conclusions
Evacuation of a hospital is more complicated than the management of MID, because the reverse actions necessary for hospital evacuation are associated with more technical and ethical decisions. 2,Reference Khorram-Manesh, Angthong and Pangma3,Reference Bagaria, Heggie, Abrahams and Murray9,Reference Nero, Örtenwall and Khorram-Manesh10,34,35,Reference Khorram-Manesh, Hedelin and Ortenwall47 Reported experiences show that significant problems and complications lie in the process of total evacuation. Although sheltering on-site may in the long-term result in severe shortages in a hospital, the complete evacuation presents the hospitals and their managers with more difficulties. It increases the need for more collaboration, coordination, and communication within the hospital as well as outside the hospital. The change of paradigm in disaster management necessitates proactivity in the hospital evacuation plan by activating society’s resources. 2,Reference Khorram-Manesh, Angthong and Pangma3,Reference Khorram-Manesh, Hedelin and Örtenwall7,33,Reference Khorram-Manesh45,Reference Khorram-Manesh, Plegas, Högstedt, Peyravi and Carlström48
The recent discussion on flexible surge capacity targets all elements of surge capacity to find out alternatives for staff, stuff, structure, and systems. In an evacuation situation, it is necessary to plan for all these alternatives. Reference Khorram-Manesh45,Reference Khorram-Manesh, Plegas, Högstedt, Peyravi and Carlström48
Future research should investigate how civilians can be empowered to act as immediate responders and assist professional first responders. Reference Khorram-Manesh, Plegas, Högstedt, Peyravi and Carlström48 It should also evaluate the need for alternative leadership and alternate care facilities within a community, which could either take responsibility for the care of lightly injured victims or for accepting lighter emergency cases from a nearby hospital to unburden emergency departments. These steps need legal and ethical evaluations but together will facilitate a flexible surge capacity that can be used in hospital evacuation as well as in other emergencies, to achieve the final goal, which is to secure the continuity of medical care for the patients. Reference Khorram-Manesh45,Reference Khorram-Manesh, Plegas, Högstedt, Peyravi and Carlström48










