The epidemiological trends in communicable diseases in Lebanon have been generally moving in the direction of greater control since the late 1990s. However, this trend was severely affected by the influx of Syrian refugees since 2011. The Syrian crisis limited the capacity of the Lebanese government to provide acceptable and continued health-care services. Reference Hajj Hussein, Mortada and Geagea1 This contributed to an increased disease burden and placed thousands of people at risk of acquiring various communicable diseases, including those diseases that did not exist earlier in Lebanon. Reference Ammar, Kdouh and Hammoud2 So, this study aims to review the main communicable diseases that experienced a sharp increase in the past 10 y in Lebanon and to highlight the reasons behind the upsurge.
Data of reported communicable diseases between January 2010 and December 2019 were obtained from the Lebanese Ministry of Public Health (LMOPH) epidemiological surveillance program public database. 3
Results and Discussion
Tuberculosis
The reported cases of tuberculosis (TB) in Lebanon had been decreasing until 2011. In 2012, the cases increased by 27% to reach 630, and kept on increasing until 2014 (Figure 1). However, 48% of the reported TB cases in 2012 were non-Lebanese. TB trends in Lebanon are low, and according to the World Health Organization (WHO), the originally higher TB prevalence among the Syrians, along with poor living conditions in Lebanon, have resulted in an elevation in TB incidence. 4 Correspondingly, the Lebanese national TB program has been strengthened (human resources, medical treatment, and monitoring prevalence and incidence). These efforts could have assisted in achieving a treatment rate of 76% for the new and relapsed cases in 2012, with 50% of those who received the treatment becoming completely cured. 4 Despite the increase in the number of reported TB cases, early detection, proper isolation, and treatment of TB patients including refugees might have helped in the prevention of a TB outbreak in Lebanon.

Figure 1. Reported cases of tuberculosis, measles, and mumps in Lebanon between 2010 and 2019.
Measles
On average, 10 cases of measles were reported annually in Lebanon between 2010 and 2012 (Figure 1). In 2013, a measles outbreak occurred where 1760 cases were reported, 13.2% of which were Syrian refugees. In 2018, another outbreak was reported with 952 and 1070 cases in 2018 and 2019, respectively, 12.7% of which were Syrian refugees. Beqaa (44.5%) and North (34.4%) governorates had the highest percentage of cases. The high-risk age groups were children below 5 y followed by children between 5 and 9 y old. For the children between 1 and 9 y, 30% received at least 1 measles containing vaccine.
The 2013 outbreak coincided with the massive influx of Syrian refugees. Studies have shown that the increased rate of measles among Lebanese shows how disturbances in the settings have exploited defects in the Lebanese measles immunization coverage to contribute to a local crisis. Reference Sharara and Kanj5 Following, the LMOPH implemented a national immunization campaign. As a result, the reported measles cases decreased after. While continuous vaccination campaigns might have attempted to manage this epidemic, challenges remain to prevent sufficient coverage. Reference Sharara and Kanj5 As for the 2018 outbreak, it occurred after the flux of refugees had stabilized in Lebanon. So, gaps appearing in the Lebanese vaccination system that might have been indirectly linked to the Syrian influx in the previous outbreak, cannot be linked to the influx in the second outbreak.
Mumps
Between 2010 and 2013, the average number of mumps reported cases in Lebanon was 17 annually (Figure 1). At the end of 2014, a localized mumps outbreak occurred. A total of 2232 cases were reported in 2014 and 2015, 21.1% of which were Syrian refugees. The highest percentage of cases was in Beqaa (60%) and North governorates (18.1%), which have the highest number of Syrian refugees living next to the border with Syria. The overcrowded Syrian population in these areas might have assisted the transmission of mumps. Following, a vaccination program was initiated by the LMOPH, 6 which contributed to decreasing the number of cases. Remarkable efforts are required to monitor and enhance vaccination coverage, especially in low coverage governorates, such as Beqaa and North. In addition to enlarging administration of vaccine at the level of primary health-care services mainly in resource limited regions. 4
Leishmaniasis
Reported cases of leishmaniasis have been only ranging between 2 and 6 annually before 2013 (Figure 2), despite the presence of its vector, that is, the sand fly in the north of Lebanon. In 2013, a Leishmaniasis outbreak occurred that was predominately involving Syrian refugees. A total of 1033 cases were reported, of which 96.6% were Syrians. Beqaa governorate had 70% of all cases and the highest incidence rate among the Syrian refugees (38/100,000). As per the Syrian Ministry of Health, tens of thousands of leishmaniasis cases are annually reported. Reference Kawa, Hanna and Bizri7 Available studies have shown that the Syrian crisis has increased the incidence of leishmaniasis in Syria, as well as in the neighboring countries. As per Sharara and Kanj, Reference Sharara and Kanj5 the high concentration of Syrian refugees, poor sanitation, and bad living conditions together with limited health-care access in rural areas contributed to the higher burden of leishmaniasis in Lebanon. Following the outbreak, the LMOPH organized a campaign by spraying pesticides to kill the vector, providing treatment free of charge, diagnosis for new cases, and disease surveillance. Reference Sharara and Kanj5 The LMOPH, with the collaboration with the WHO, was able to contain the outbreak. This fast response played a key role in the containment and has been recommended as an effective way for managing future outbreaks. Reference Kawa, Hanna and Bizri7
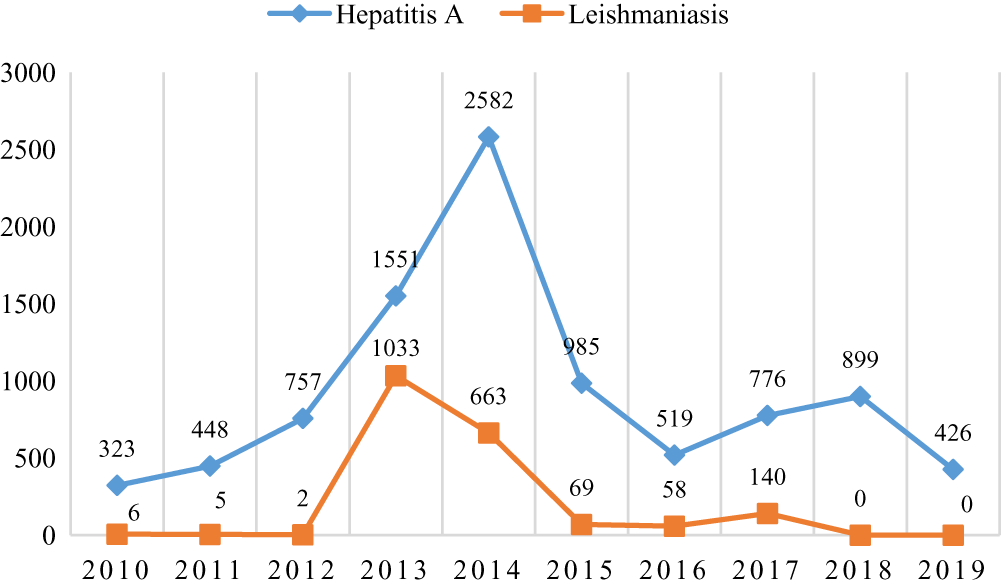
Figure 2. Reported cases of leishmaniasis and hepatitis A in Lebanon between 2010 and 2019.
Hepatitis A
Between 2010 and 2012, the annual average of reported hepatitis A cases in Lebanon was 509 (Figure 2). In 2014, a total of 2582 cases were reported, 33.3% of which were Syrian refugees. The sharp increase in hepatitis A cases in 2013 concurred with a massive wave of Syrian refugees. The cases were mainly reported from Beqaa (58.8%) and North (22.4%) governorates. Studies done in Lebanon have revealed that surface and groundwater are able to carry hepatitis A virus (HAV) because of untreated sewage. Reference Bizri, Fares and Musharrafieh8,Reference Assaf and Saadeh9 Around 17% of Syrian refugees in Lebanon are living in informal camps Reference Hajj Hussein, Mortada and Geagea1,Reference Ammar, Kdouh and Hammoud2 where most of them suffer from a shortage of clean drinking water. Moreover, the poor sanitary infrastructure, the accretion of solid waste, and the absence of sewage networks resulted in an open defecation in many camps. To solve this, the Lebanese authorities shared this problem with the 67th World Health Assembly where an improvement plan was developed to prevent viral hepatitis and to encourage and reinforce immunization strategies. Reference Bizri, Fares and Musharrafieh8 Consequently, Lebanon succeeded in managing the HAV outbreak.
Approximately 8840 HAV cases were reported between 2010 and 2018. A total of 34.4% belonged to the age group of 10-19 y, while only 0.43% were above 60 y old, which can be explained because older age groups have already an immunity to HAV. At present (2021), the HAV vaccination in Lebanon is not obligatory. It is provided by the public health sector, at a cost, through primary health-care centers. Thus, to prevent HAV in Lebanon, the Lebanese authorities should offer suitable and safe water supply, improve the living situations of the Lebanese and Syrian refugees especially in rural areas, and finally, nationalize and provide HAV vaccine to children. Reference Bizri, Fares and Musharrafieh8
Our study has some limitations. First, the discussed communicable diseases are mandatory notifiable to the LMOPH either immediately or weekly. So, relying on the reported cases of diseases may underestimate the real situation. Second, the sociological and social determinants were not studied in this report so, further studies are recommended to include these determinants.
Conclusions
In conclusion, the massive influx of Syrian refugees to Lebanon, the waste management crisis, the lack of developmental projects mainly in Beqaa and North governorates, in addition to the poor water management system, lack of clean drinking water, poor sanitation, and deprived living conditions with limited health-care access in rural areas, might have contributed to the increase in the transmission of communicable diseases in Lebanon. Despite the limited resources and the challenges that resulted from the Syrian crisis, the LMOPH succeeded in containing several outbreaks and preventing the spread of communicable diseases in the past 10 y. Nevertheless, further efforts are needed from the Lebanese authorities to improve the identified gaps to avoid future outbreaks and similar events.
Acknowledgment
We thank Mr. Bashar Farran who contributed to editing the writing language of this study.
Authors contributions
Sahar Hammoud, David Onchonga, and Béla Kocsis were responsible for the conception and the design of the study. Sahar Hammoud was responsible for the acquisition of data. Sahar Hammoud and Faten Amer were responsible for the analysis and interpretation of data. Sahar Hammoud was responsible for drafting the study. All authors revised the study critically and approved the final manuscript.




