Introduction
Attention-deficit/hyperactivity disorder (ADHD) is a chronic neurodevelopmental disorder characterized by clinically significant inattentive and hyperactive/impulsive symptoms (American Psychiatric Association [APA], 2013), and is one of the most prevalent psychiatric disorders in childhood (Polanczyk et al., Reference Polanczyk, Willcutt, Salum, Kieling and Rohde2014). ADHD symptoms emerge in early development and predict a range of adverse clinical, academic, socioemotional, and functional impairments into adulthood (Pelham et al., Reference Pelham, Fabiano and Massetti2005), exacting annual illness-related costs of over $100 billion in the US alone (Zhao et al., Reference Zhao, Page, Altszuler, Pelham, Kipp, Gnagy, Coxe, Schatz, Merrill, Macphee and Pelham2019). Importantly, though evidence supports the validity of ADHD as a diagnostic entity, our knowledge of factors contributing to the well-documented instability of ADHD symptom severity and subtypes across development is limited (for review, see Willcutt et al., Reference Willcutt, Nigg, Pennington, Solanto, Rohde, Tannock, Loo, Carlson, McBurnett and Lahey2012). Moreover, while decades of critical ADHD research have identified risk factors associated with the disorder, empirical work examining factors contributing to positive development among youth with ADHD remains in its nascent stages (Chan et al., Reference Chan, Groves, Marsh, Miller, Richmond and Kofler2022, Reference Chan, Barroso, Groves, Marsh, Black, Jaisle and Kofler2023; Dvorsky & Langberg, Reference Dvorsky and Langberg2016). Developmental psychopathology models that emphasize both risk and protective factors are needed to understand individual differences not only in psychopathology, but also in adaptive outcomes such as higher levels of interpersonal functioning, among youth with ADHD (Hinshaw & Becker, Reference Hinshaw and Becker2020). In line with developmental psychopathology models, one promising approach to understanding risk and protective factors in ADHD is through the lens of a dimensional-trait framework. One such model, which conceives of traits in neurobehavioral terms, is the triarchic model (Patrick et al., Reference Patrick, Fowles and Krueger2009, Reference Patrick, Iacono and Venables2019).
Triarchic model
Early temperament traits, theorized to reflect basic neurobehavioral propensities (e.g., Buss & Plomin, Reference Buss and Plomin1975; Rothbart, Reference Rothbart, Kohnstamm, Bates and Rothbart1989), are increasingly recognized as significant factors for understanding the developmental trajectories of childhood psychopathology (for discussion, see Perkins et al., Reference Perkins, Latzman and Patrick2020). The neurobehavioral trait constructs of the triarchic model (Patrick et al., Reference Patrick, Fowles and Krueger2009, Reference Patrick, Iacono and Venables2019; Patrick, Reference Patrick2022) have shown promise for elucidating both adaptive and maladaptive trajectories involving externalizing forms of psychopathology, including substance use problems, antisocial behavior, and ADHD (Bertoldi et al., Reference Bertoldi, Perkins, Tuvblad, Oskarsson, Kramer, Latzman, Baker, Raine and Patrick2022; Bertoldi et al., Reference Bertoldi, Tuvblad, Joyner, Ganley, Raine, Baker and Patrick2023; Palumbo et al., Reference Palumbo, Patrick and Latzman2021; Patrick, Reference Patrick2022; Perkins et al., Reference Perkins, Joyner, Foell, Drislane, Brislin, Frick, Yancey, Soto, Ganley, Keel, Sica, Flor, Nees, Banaschewski, Bokde, Desrivières, Grigis, Garavan, Gowland and Patrick2022). The triarchic model traits are boldness, reflecting social dominance, emotional resiliency, and venturesomeness; meanness, entailing aggressive resource seeking without regard for others; and disinhibition, involving deficient restraint and general proneness to impulse control problems (Patrick et al., Reference Patrick, Fowles and Krueger2009). Consistent with the view of the triarchic traits as reflecting basic neurobehavioral propensities, a growing body of research indicates that these traits can be indexed using measures from modalities of behavioral performance, neurophysiological response, and report-based measures (Palumbo et al., Reference Palumbo, Perkins, Yancey, Brislin, Patrick and Latzman2020; Patrick, Reference Patrick2022; Patrick, Iacono, et al., Reference Patrick, Iacono and Venables2019; Perkins et al., Reference Perkins, Latzman and Patrick2020; Venables et al., Reference Venables, Foell, Yancey, Kane, Engle and Patrick2018; Yancey et al., Reference Yancey, Venables and Patrick2016).
The triarchic model was originally formulated to advance understanding of maladaptive (e.g., explosive, impulsive, reckless, and irresponsible actions) and adaptive (e.g., charm, self-assurance, stress resilience, and leadership) features of psychopathy in adults (Patrick et al., Reference Patrick, Fowles and Krueger2009). More recently, the model has been applied to children and youth, with several studies supporting the reliability and distinctiveness of the triarchic traits, and their associations with relevant criterion measures, in younger-aged samples (e.g., Kyranides et al., Reference Kyranides, Fanti, Sikki and Patrick2017; Sica et al., Reference Sica, Ciucci, Baroncelli, Frick and Patrick2020; Somma et al., Reference Somma, Borroni, Drislane and Fossati2016). Critically, however, the triarchic model is a neurobehavioral framework with transdiagnostic implications for developmental understanding of psychopathology and adaptive outcomes outside of psychopathy (Patrick et al., Reference Patrick, Iacono and Venables2019; Patrick, Reference Patrick2022). For example, boldness relates strongly to self-report measures of fearlessness, low threat sensitivity, and tolerance for uncertainty (Benning et al., Reference Benning, Patrick, Blonigen, Hicks and Iacono2005; Patrick, Kramer, et al., Reference Patrick, Kramer, Vaidyanathan, Benning, Hicks and Lilienfeld2019) and has been shown to relate inversely to internalizing psychopathology (Latzman et al., Reference Latzman, Palumbo, Sauvigné, Hecht, Lilienfeld and Patrick2019, Reference Latzman, Palumbo, Krueger, Drislane and Patrick2020). Meanness (or callousness; Frick et al., Reference Frick, Ray, Thornton and Kahn2014), on the other hand, is hypothesized to entail deficits in neural systems for empathic concern (Blair, Reference Blair1995, Reference Blair, Farrow and Woodruff2007; Marsh et al., Reference Marsh, Finger, Fowler, Adalio, Jurkowitz, Schechter and Blair2013) and social affiliation (Green et al., Reference Green, Palumbo, Shishido, Kesner and Latzman2020; Patrick et al., Reference Patrick, Fowles and Krueger2009; Viding & McCrory, Reference Viding and McCrory2019). Clinical researchers working with children and adolescents have suggested that impaired conscience development arising from lack of fear, and negative social exchanges that arise from weak restraint, also contribute to the development of meanness (Frick & Morris, Reference Frick and Morris2004; Patrick et al., Reference Patrick, Fowles and Krueger2009). Disinhibition is posited to involve dysfunction in frontal-regulatory circuity of the brain (Davidson et al., Reference Davidson, Putnam and Larson2000; Patrick & Drislane, Reference Patrick and Drislane2015), reflected in lower performance on executive-function tasks and decreased brain activation during cognitive processing tasks (Ribes-Guardiola et al., Reference Ribes-Guardiola, Poy, Patrick and Moltó2020; Venables et al., Reference Venables, Foell, Yancey, Kane, Engle and Patrick2018; Yancey et al., Reference Yancey, Venables, Hicks and Patrick2013).
Triarchic traits in ADHD and related functional outcomes
Disinhibition and meanness are the two dimensions of the triarchic model that have been studied most in relation to ADHD. Disinhibition is associated cross-sectionally with attention problems, a diagnosis of ADHD, and ADHD-related impairment (Palumbo et al., Reference Palumbo, Patrick and Latzman2021; Perkins et al., Reference Perkins, Joyner, Foell, Drislane, Brislin, Frick, Yancey, Soto, Ganley, Keel, Sica, Flor, Nees, Banaschewski, Bokde, Desrivières, Grigis, Garavan, Gowland and Patrick2022). Although disinhibition shares conceptual overlap with ADHD symptoms and ADHD is often seen as the earliest manifestation of disinhibitory tendencies (Beauchaine et al., Reference Beauchaine, Zisner and Sauder2017), empirical evidence indicates that this trait is best viewed as a risk factor (liability) for the development of ADHD symptoms (i.e., vulnerability hypothesis) rather than as a component of the disorder itself (i.e., continuum hypothesis; Gagne & Hill Goldsmith, Reference Gagne and Hill Goldsmith2011; Wichstrøm et al., Reference Wichstrøm, Stenseng, Belsky, von Soest and Hygen2019). In particular, findings from etiologically informed studies provide evidence for disinhibition as a liability factor for externalizing problems, including ADHD (see Perkins et al., Reference Perkins, Latzman and Patrick2020). For example, longitudinal research has shown that disinhibition predicts escalation of ADHD-related impairment across time (Perkins et al., Reference Perkins, Joyner, Foell, Drislane, Brislin, Frick, Yancey, Soto, Ganley, Keel, Sica, Flor, Nees, Banaschewski, Bokde, Desrivières, Grigis, Garavan, Gowland and Patrick2022), and twin research has demonstrated that shared genetic factors influence both disinhibitory traits and ADHD symptoms (as part of the broader externalizing spectrum; Young et al., Reference Young, Stallings, Corley, Krauter and Hewitt2000, Reference Young, Friedman, Miyake, Willcutt, Corley, Haberstick and Hewitt2009). However, the effect of disinhibition in relation to ADHD also appears to change over development, showing reduced heritability at age 17 relative to age 12 (Young et al., Reference Young, Friedman, Miyake, Willcutt, Corley, Haberstick and Hewitt2009).
The triarchic trait of meanness has also been examined in relation to ADHD symptomatology. A study by Palumbo et al. (Reference Palumbo, Patrick and Latzman2021) found meanness to be positively correlated at the zero-order level with attention problems and likelihood of an ADHD diagnosis, but this association was greatly attenuated when accounting for moderate-level covariation between meanness and disinhibition (Palumbo et al., Reference Palumbo, Patrick and Latzman2021). In contrast to disinhibition, meanness appears more specifically predictive of antisocial manifestations of externalizing (e.g., conduct problems) than of impulsive rule-breaking behavior or ADHD-related impairment (Perkins et al., Reference Perkins, Joyner, Foell, Drislane, Brislin, Frick, Yancey, Soto, Ganley, Keel, Sica, Flor, Nees, Banaschewski, Bokde, Desrivières, Grigis, Garavan, Gowland and Patrick2022; Sica et al., Reference Sica, Ciucci, Baroncelli, Frick and Patrick2020).
To date, there has been less research examining the third triarchic trait, boldness, in relation to ADHD. The work that does exist provides some basis for predicting that boldness may operate in a protective manner to mitigate ADHD-related impairment. Two cross-sectional studies, one with children (Palumbo et al., Reference Palumbo, Patrick and Latzman2021) and the other with adolescents (Sica et al., Reference Sica, Ciucci, Baroncelli, Frick and Patrick2020), found small negative associations for boldness with ADHD-related problems (ßs = −.11 and −.26, respectively, when controlling for meanness and disinhibition). Socially adaptive behaviors associated with boldness may explain these findings: As noted above, this trait includes elements of social assuredness, dominance and leadership, and efficacious interpersonal relations (Green et al., Reference Green, Palumbo, Shishido, Kesner and Latzman2020; Lilienfeld et al., Reference Lilienfeld, Smith, Sauvigné, Patrick, Drislane, Latzman and Krueger2016; Neo et al., Reference Neo, Sellbom, Smith and Lilienfeld2018; Sica et al., Reference Sica, Ciucci, Baroncelli, Frick and Patrick2020). In contrast, ADHD frequently involves social impairments (for review, see Ros & Graziano, Reference Ros and Graziano2018) that appear to vary based on the symptom dimension in question. For example, inattention symptoms are associated with deficits in assertiveness and proneness to social withdrawal (Marshall et al., Reference Marshall, Evans, Eiraldi, Becker and Power2014; Solanto et al., Reference Solanto, Pope-Boyd, Tryon and Stepak2009) – characteristics that are incompatible with boldness. In contrast, hyperactive/impulsive symptoms are associated with higher rates of socially disruptive behaviors (Garner et al., Reference Garner, O’Connor, Narad, Tamm, Simon and Epstein2013; Solanto et al., Reference Solanto, Pope-Boyd, Tryon and Stepak2009), which are observed more generally among disinhibited individuals (Green et al., Reference Green, Palumbo, Shishido, Kesner and Latzman2020; Patrick & Drislane, Reference Patrick and Drislane2015). Given these findings, it can be hypothesized that over the course of development, the triarchic traits may influence ADHD symptomatology in either a protective manner (boldness) or as a risk factor (disinhibition) – indirectly, through their effects on social functioning.
Effects of sex differences on ADHD and/or the triarchic traits
Another important consideration is whether these relations differ based on sex assigned at birth. Research to date indicates that males tend to score higher than females on boldness and meanness (though not disinhibition; Drislane & Patrick, Reference Drislane and Patrick2017; Murphy et al., Reference Murphy, Lilienfeld, Skeem and Edens2016; Sica et al., Reference Sica, Perkins, Joyner, Caudek, Bottesi, Caruso and Patrick2021, Reference Sica, Ciucci, Baroncelli, Frick and Patrick2020; c.f. Somma et al., Reference Somma, Borroni, Drislane and Fossati2016), but no study has yet tested for sex differences in associations of the triarchic traits with ADHD. In regard to sex differences and ADHD symptoms, meta-analytic findings indicate that males with ADHD exhibit higher levels of hyperactive/impulsive but not inattentive symptoms (Loyer Carbonneau et al., Reference Loyer Carbonneau, Demers, Bigras and Guay2021) as compared to females diagnosed with ADHD (Gaub and Carlson, Reference Gaub and Carlson1997; Gershon & Gershon, Reference Gershon and Gershon2002; Loyer Cargonneau et al., Reference Loyer Carbonneau, Demers, Bigras and Guay2021). Findings pertaining to sex differences in ADHD-related social impairments, on the other hand, have been highly mixed. Some studies have found higher levels of interpersonal difficulties for females with ADHD compared to males (e.g., Diamantopoulou et al., Reference Diamantopoulou, Henricsson and Rydell2005; Fedele et al., Reference Fedele, Lefler, Hartung and Canu2012), whereas others have reported either the reverse (e.g., Thorell & Rydell, Reference Thorell and Rydell2008) or no sex differences (e.g., Gershon & Gershon, Reference Gershon and Gershon2002; Greene et al., Reference Greene, Biederman, Faraone, Monuteaux, Mick, DuPre, Fine and Goring2001; Mikami & Lorenzi, Reference Mikami and Lorenzi2011). Further research is needed to resolve these inconsistencies in the literature and evaluate whether they might be attributable to sex differences in ADHD-relevant neurobehavioral traits, such as those of the triarchic model.
Current study
The present study is the first to examine how neurobehavioral traits described by the triarchic model (Patrick et al., Reference Patrick, Fowles and Krueger2009; Patrick, Reference Patrick2022) relate to ADHD symptomatology concurrently and prospectively. The study had four major aims. The first was to evaluate how the triarchic traits (i.e., boldness, meanness, and disinhibition) relate to symptoms of ADHD assessed concurrently at age 14, and to the trajectory of ADHD symptoms across time, from age 14 to age 19. We hypothesized that disinhibition and boldness would each show associations with concurrent and prospective changes in ADHD symptomatology, but in opposing directions, such that disinhibition would relate to greater symptoms and boldness to fewer symptoms. The second study aim was to examine interpersonal difficulties at age 17 as a mediator of the expected relations between earlier (age 14) triarchic traits and later (age 19) ADHD symptoms. We hypothesized that the positive prospective relationship between disinhibition and ADHD would be explained in part by increased social impairment. In contrast, the negative prospective association between boldness and ADHD would be explained by enhanced social functioning.
The third study aim was to test differences in associations of the triarchic traits with inattentive versus hyperactive/impulsive symptom subdimensions of ADHD, and the potential role of social impairment as a mediator in these relations. We hypothesized that observed relations of boldness and disinhibition with overall ADHD symptoms would be driven more by the hyperactive/impulsive symptoms than by the inattentive symptoms, and that these associations would be mediated by social impairment. Finally, we evaluated whether triarchic trait/ADHD symptom associations might differ by sex. Given the limited prior research on sex differences in ADHD, we had no specific hypotheses regarding these associations.
Method
Participants
Participants were twins and triplets from the University of Southern California Risk Factors for Antisocial Behavior project. Data collection for the project occurred across five waves, with the first (Wave 1 [W1]) occurring during 2000-2004 when participants were 9 to 10 years of age, and subsequent waves occurring every 2 to 3 years thereafter, with W3, W4, and W5 occurring at ages 14 to 15, 16 to 18, and 19 to 20, respectively. Additional participants were recruited at W3 to be representative of the greater Los Angeles area in terms of race/ethnicity and socioeconomic status (for further details regarding sample characteristics; see Baker et al. (Reference Baker, Barton and Raine2002) and Baker et al. (Reference Baker, Barton, Lozano, Raine and Fowler2006) for details regarding recruitment and study inclusion criteria). The total W3 sample consisted of 1,185 youth with a mean age of 14.87 years (SD = .87), of whom 51.2% were female. Regarding race/ethnicity, 31.9% identified as Caucasian, 33.2% as Hispanic, 12.1% as Black, 4.1% as Asian, and 18.0% as Mixed; 0.8% of the sample did not report their race/ethnicity.
Procedure
At each time point, youth and their adult caregivers (>90% biological mothers) completed clinical interviews and questionnaires; youth additionally participated in neurocognitive and psychophysiological testing. The majority of families completed an in-lab study visit, with some participating via mail, phone, or internet surveys. Adult caregivers provided informed consent at each time point, as did youth aged 18 or older. All study procedures were approved by the USC Institutional Review Board.
Measures
Wave 3 triarchic traits
Self-report-based triarchic trait scales developed for this prospective longitudinal study and validated in prior published work (Bertoldi et al., Reference Bertoldi, Perkins, Tuvblad, Oskarsson, Kramer, Latzman, Baker, Raine and Patrick2022) were used to quantify boldness, meanness, and disinhibition at W3. Briefly, candidate items were initially selected using a construct-referenced rating approach (Hall et al., Reference Hall, Drislane, Murano, Patrick, Lilienfeld and Poythress2014), and scales were refined iteratively to optimize psychometric properties while maintaining sufficient content coverage of the nuances of each trait (Bertoldi et al., Reference Bertoldi, Perkins, Tuvblad, Oskarsson, Kramer, Latzman, Baker, Raine and Patrick2022). The resulting scales consist of 32 items (10 for boldness, 10 for meanness, and 12 for disinhibition) from two inventories administered to study participants: (1) the self-report Child Psychopathy Scale (Lynam, Reference Lynam1997; e.g., Are you kind?; originally rated 0 = not true, 1=somewhat true, 2 = very true) and (2) the Youth Self-Report inventory (Achenbach & Edelbrock, Reference Achenbach and Edelbrock1991; e.g., Impulsive; 0 = no, 1 = yes). Items were reverse-coded as needed to reflect higher levels of the relevant triarchic trait, z-scored to account for different rating scales and item difficulties, and averaged to create participant scores for each trait (Bertoldi et al., Reference Bertoldi, Perkins, Tuvblad, Oskarsson, Kramer, Latzman, Baker, Raine and Patrick2022). Internal consistency reliabilities (αs) for these scales at W3 of the current study were .66, .69, and .72, respectively.
Wave 3 ADHD symptoms
The Diagnostic Interview Schedule for Children – Version IV (Shaffer et al., Reference Shaffer, Fisher, Lucas, Dulcan and Schwab-Stone2000), a structured diagnostic interview for children and adolescents, was used to operationalize parent-reported ADHD symptoms at W3. The Diagnostic Interview Schedule for Children was administered to parents at each of the first four waves to assess their children’s internalizing and externalizing symptoms; youth responded to questions about conduct disorder only as this was the focus of the original study. All symptom-level criteria (e.g., Often avoids tasks that require attention) were coded as No (0) or Yes (1) based on whether they had occurred over the preceding year. The ADHD module of the Diagnostic Interview Schedule for Children yielded parent-reported symptom counts for hyperactive/impulsive (9 items; α = .88), inattentive (9 items; α = .81), and total symptoms (18 items; α = .87).
Wave 5 ADHD symptoms
At study W5, youth completed the Barkley Adult ADHD Rating Scale – Version IV (Barkley, Reference Barkley2011) as an index of self-reported ADHD symptoms. The Barkley Adult Rating Scale – Version IV consists of 18 self-report items (e.g., Fidgets) assessing hyperactive/impulsive (9 items; α = .81) and inattentive behaviors (e.g., Easily distracted; 9 items; α = .89), as well as a total score (α = .91). Items were rated on a four-point Likert scale including Never or Rarely (0), Sometimes (1), Often (2), and Very Often (3) over the last week.
Waves 3 and 4 interpersonal problems
At W3 and W4, participants completed the Youth Self-Report inventory, which comprises 112 items assessing different types of behavioral, social, and emotional competencies in youth. Each item was rated as Not True (0), Somewhat or Sometimes True (1), or Very True or Often True (2) over the last six months. In the current study, the Social Problems composite (11 items, e.g., Does not get along with peers; αs = .70 at W3 and .68 at W4) was utilized as an index of child-reported problems in peer-to-peer interactions.
Analytic plan
The main analytic approach used to test study hypotheses was path analysis, performed using Mplus 8.6 (Muthén & Muthén, 1998-Reference Muthén and Muthén2017). Standard errors were adjusted for family clustering using a sandwich estimator as implemented within maximum likelihood with robust standard errors. Maximum likelihood with robust standard errors was also used to handle missing data. The variances of all predictor variables were added to all models to treat these variables as endogenous, permitting their inclusion in maximum likelihood with robust standard errors to handle missing data. Thus, all participants were included in every analysis, except for a small number of individuals who were missing all variables for a given analysis (mean participants missing across models = 4.19%; range = 2.28 to 7.09%); inclusion ns are reported for each analysis. Exclusion of these participants was considered unlikely to introduce excess bias given that Little’s missing completely at random test was nonsignificant, increasing confidence that the data were at least missing at random (χ2(326) = 136.40, p > .999).
Given the positively skewed and leptokurtic distribution of ADHD symptoms in this community sample (see Table 1) and the count nature of these outcome variables, negative binomial regression was used for all analyses. This analytic approach yields incidence rate ratios (IRRs) for each predictor, reflecting the percent change in the outcome variable for a one-unit increase in the predictor from the predictor’s mean. For example, an IRR of 1.20 indicates a 20% increase in the outcome variable, whereas an IRR of .70 signifies a 30% decrease. Unstandardized regression coefficients were exponentiated to convert them to IRRs. Continuous scores for the triarchic trait scales were winsorized to a criterion of median ± 2 interquartile ranges to allow for representation of a range of values and include all participants, while limiting excessive influence of outliers. This procedure resulted in the winsorization of 9 low values for boldness, 73 high values for meanness, and 2 high values for disinhibition.Footnote 1 Given the importance of measurement scale for IRR interpretability, winsorized triarchic scores were z-scored prior to analysis.
Table 1. Zero-order correlations and descriptive statistics for all study variables
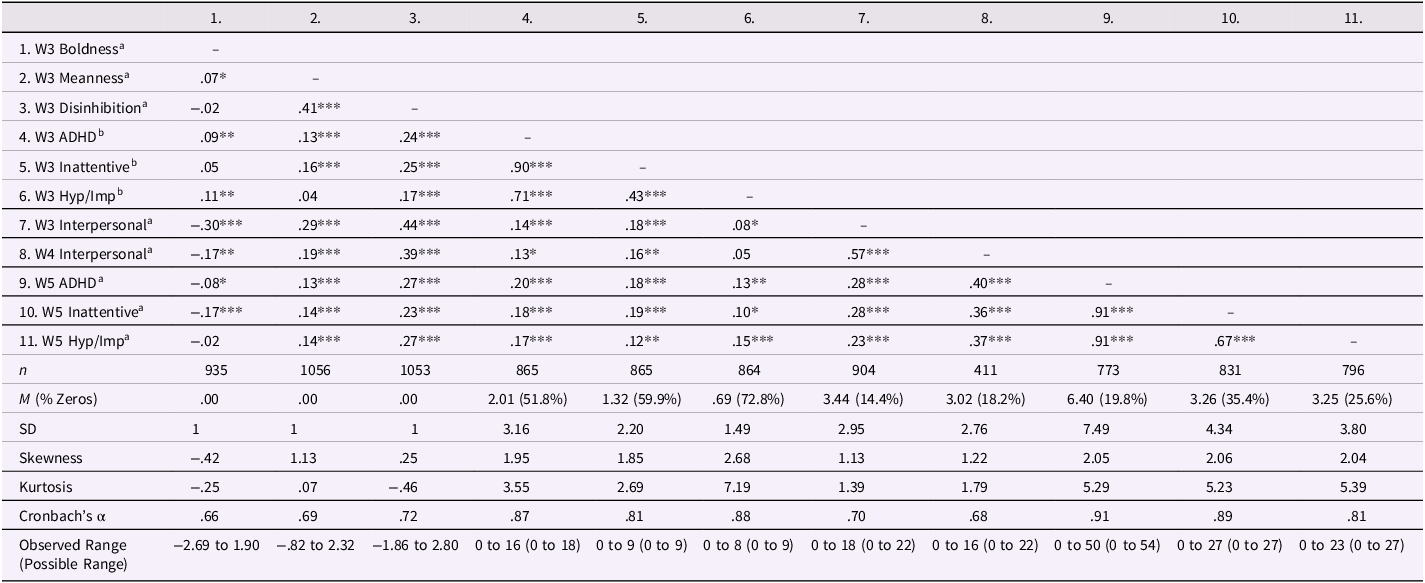
Note. W3 = Wave 3 assessment (age 14); W4 = Wave 4 assessment (age 17); W5 = Wave 5 assessment (age 19); ADHD = total attention-deficit/hyperactivity disorder symptoms; Inattentive = inattentive symptom dimension of ADHD; Hyp/Imp = hyperactive/impulsive symptom dimension of ADHD; Interpersonal = interpersonal problems. aYouth-reported. bParent-reported. All correlations are Spearman’s ρs. *p < .05, **p < .01, ***p < .001.
To test Aim 1 hypotheses, pertaining to concurrent and prospective associations of traits with ADHD symptoms, we performed separate analyses regressing (a) age 14 ADHD symptoms onto age 14 boldness, meanness, and disinhibition, and (b) age 19 ADHD symptoms onto age 14 ADHD symptoms, boldness, meanness, and disinhibition. For Aim 2, we added age 17 interpersonal problems to the model and calculated direct and indirect effects to determine whether such problems mediated the observed relations between age 14 triarchic traits and age 19 ADHD symptoms. This model also included age 14 interpersonal problems as a covariate to control for existing interpersonal problems. To test Aim 3 hypotheses, we repeated all analyses with inattentive and hyperactive/impulsive symptom subdimensions included as separate outcome variables within a single model. Finally, we tested hypotheses for Aim 4 using a multigroup path analysis, with groups consisting of males and females. A chi-square difference test was used to evaluate whether imposing the constraint of equality of all paths across groups resulted in significantly worse model fit. Significant overall decrements in model fit were probed by constraining paths one by one.
Results
Aim 1: Concurrent and prospective associations between triarchic traits and total ADHD symptoms
In the concurrent path model for this Aim (model n = 1,101), boldness showed an unexpected positive association with concurrent ADHD symptoms, IRR = 1.14, p = 0.020, 95% CI = [1.02, 1.28], and disinhibition showed a strong positive association, IRR = 1.44, p < .001, 95% CI = [1.28, 1.62]. In the prospective path model (n = 1,147), when accounting for the predictive effect of age 14 ADHD symptoms, age 14 boldness was negatively related to age 19 ADHD symptoms, IRR = .91, p = .034, 95% CI = [.83, .99], whereas disinhibition showed an opposing positive association, IRR = 1.25, p < .001, 95% CI = [1.14, 1.38]. Meanness was unrelated to ADHD symptoms in either model. Results for these path models (concurrent, prospective) are depicted in Figure 1.
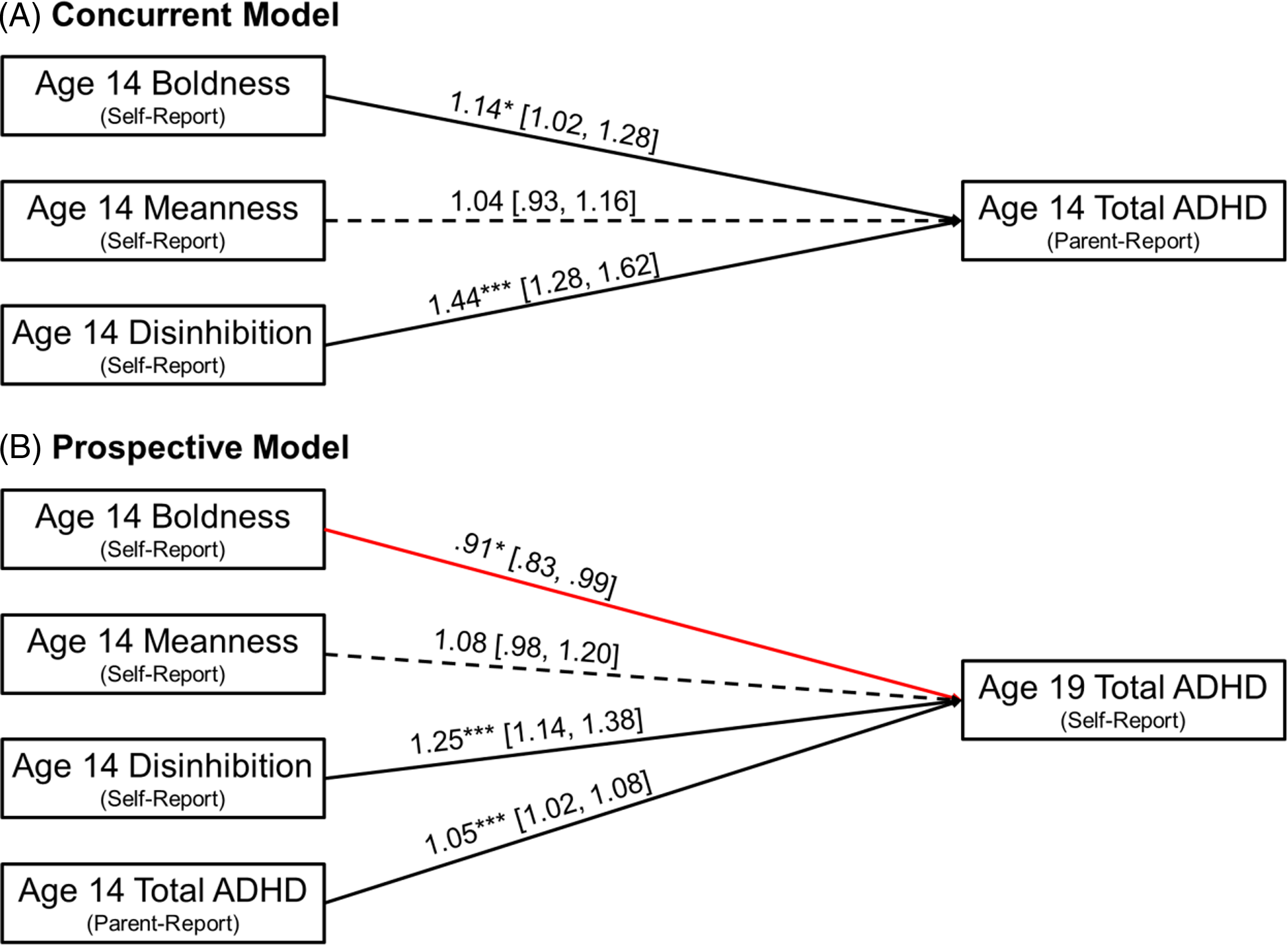
Figure 1. Concurrent (panel A) and prospective (panel B) path models for total ADHD symptoms; the latter controls for age 14 symptoms. Path coefficients are incidence rate ratios (IRRs) from negative binomial regression models shown with [95% confidence intervals]. Standard errors are adjusted for within-family clustering. Negative paths are red and nonsignificant paths (p > .05) are dashed. Model ns = 1,101 and 1,147. *p < .05, ***p < .001.
Aim 2: Social problems as a mediator of paths between triarchic traits and total ADHD symptoms
Figure 2 depicts the model testing for a mediating effect of age 17 interpersonal problems on the associations between age 14 triarchic traits and age 19 ADHD symptoms, controlling for ADHD symptoms and interpersonal problems at age 14 (model n = 1,152). Age 14 disinhibition showed a significant total effect on age 19 ADHD symptoms, total IRR = 1.17, p = .002, 95% CI = [1.06, 1.29]. This included both direct and indirect positive associations with age 19 ADHD symptoms, direct path IRR = 1.15, p = .005, 95% CI = [1.04, 1.28]; indirect path IRR = 1.01, p = .028, 95% CI = [1.00, 1.02]. That is, a small portion (6.5%) of the positive association between disinhibition and ADHD was attributable to the escalation of interpersonal problems by age 17. Importantly, this effect was observed over and above the other triarchic traits, and over and above ADHD symptoms and interpersonal problems already evident at age 14, pointing to specificity of the finding. Neither boldness nor meanness showed direct or indirect associations with ADHD symptoms at age 19; of note, the negative direct association for boldness observed in Aim 1 was reduced to nonsignificant with the inclusion of age 14 interpersonal problems in the analytic model.
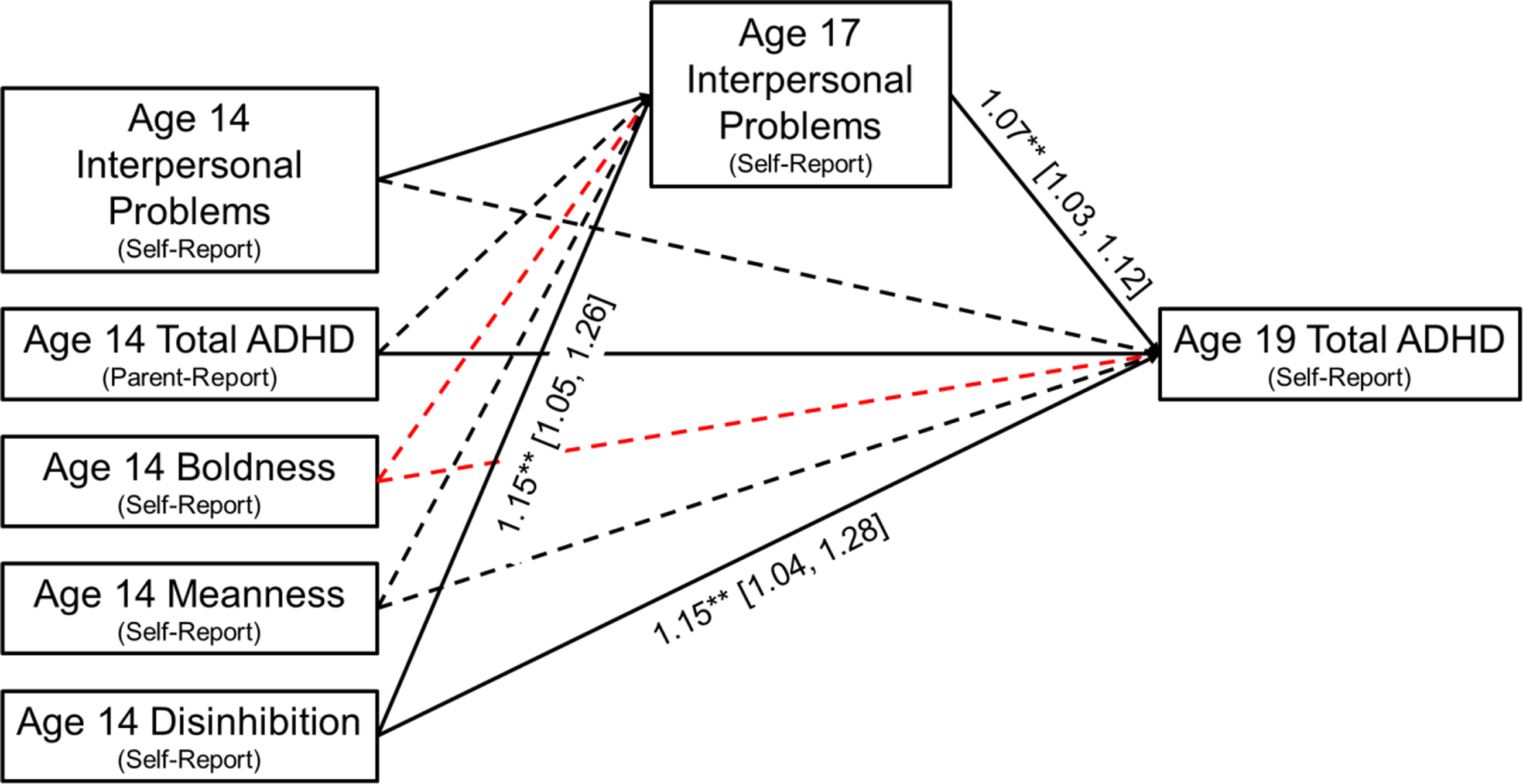
Figure 2. Prospective mediation model for total ADHD symptoms, controlling for age 14 symptoms and interpersonal problems. Path coefficients are incidence rate ratios (IRRs) from negative binomial regression models shown with [95% confidence intervals]. Standard errors are adjusted for within-family clustering. Negative paths are red and nonsignificant paths (p > .05) are dashed. Model n = 1,152. **p < .01.
Aim 3: Differential effects for ADHD subdimensions
In the concurrent model for ADHD symptom subdimensions at age 14 (n = 1,101; see Figure 3), only disinhibition emerged as a significant predictor of inattentive symptoms, IRR = 1.43, p < .001, 95% CI = [1.26, 1.63], whereas both boldness and disinhibition showed positive predictive relations with hyperactive/impulsive symptoms, IRRs = 1.32 and 1.50, ps < .001, 95% CIs = [1.14, 1.54] and [1.28, 1.77], respectively.
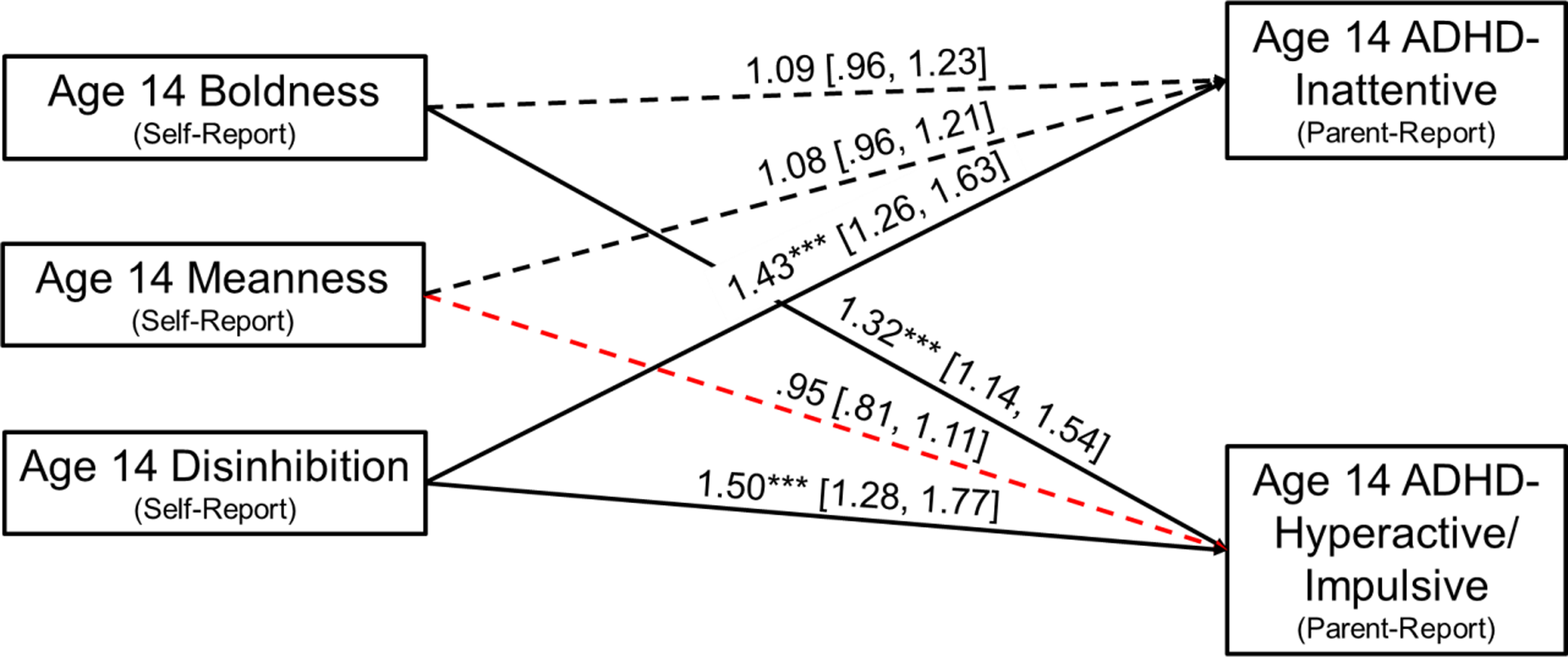
Figure 3. Concurrent path model for ADHD subdimensions. Path coefficients are incidence rate ratios (IRRs) from negative binomial regression models shown with [95% confidence intervals]. Standard errors are adjusted for within-family clustering. Negative paths are red and nonsignificant paths (p > .05) are dashed. Model n = 1,101. ***p < .001.
By contrast, in the prospective model that controlled for age 14 ADHD subdimensions (n = 1,153; Figure 4), boldness was negatively associated with later inattentive symptoms, IRR = .81, p < .001, 95% CI = [.72, .90], whereas disinhibition showed an opposing positive association, IRR = 1.27, p < .001, 95% CI = [1.13, 1.41]. Disinhibition and meanness prospectively predicted greater hyperactive/impulsive symptoms at age 19, IRRs = 1.26 and 1.12, ps = <.001 and .030, 95% CIs = [1.15, 1.39] and [1.01, 1.24], respectively.
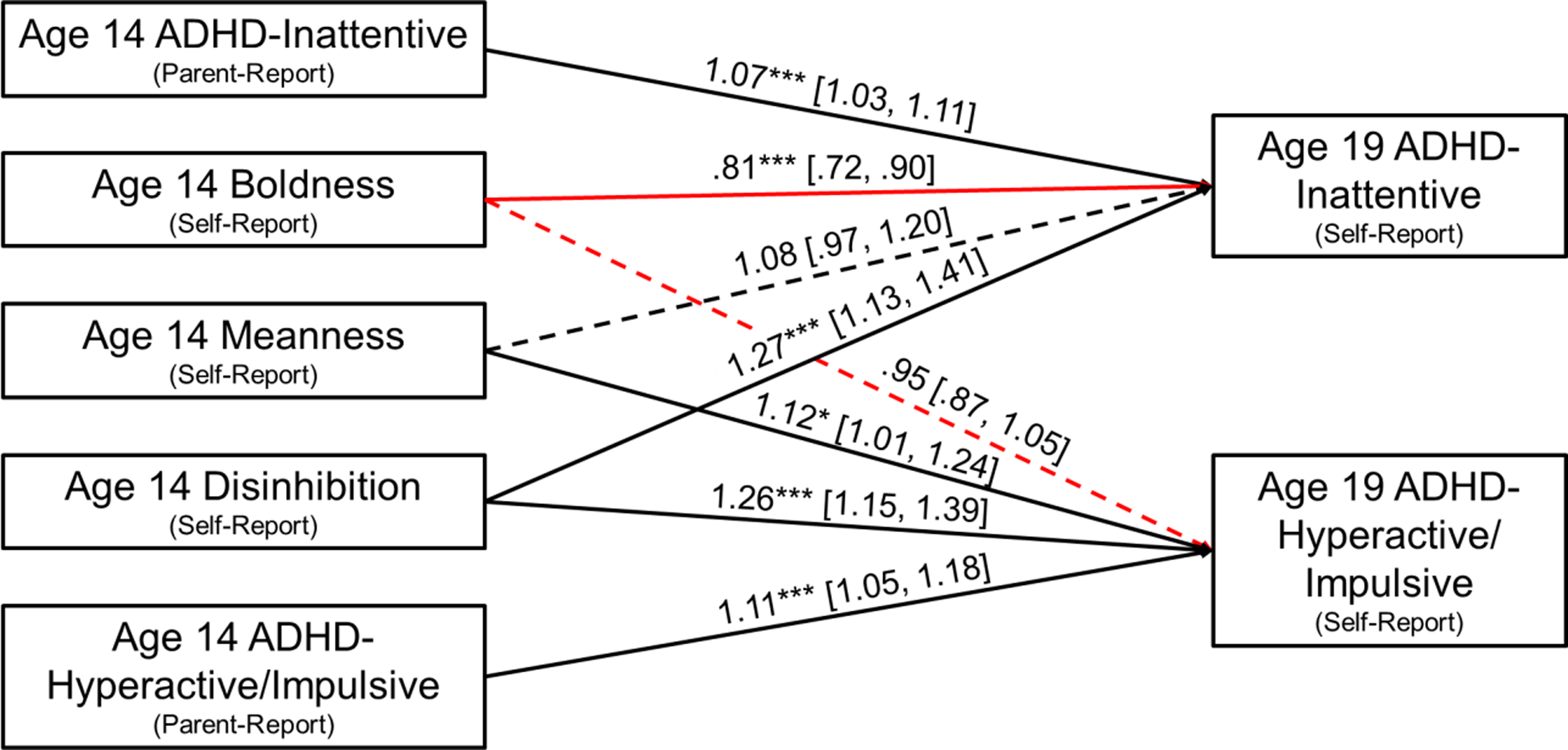
Figure 4. Prospective path model for ADHD subdimensions, controlling for age 14 symptoms. Path coefficients are incidence rate ratios (IRRs) from negative binomial regression models shown with [95% confidence intervals]. Standard errors are adjusted for within-family clustering. Negative paths are red and nonsignificant paths (p > .05) are dashed. Model n = 1,153. *p < .05, ***p < .001.
The mediation model for age 17 interpersonal problems (model n = 1,158) is depicted in Figure 5. Controlling for concurrent symptoms and interpersonal problems, disinhibition evidenced significant total effects on each ADHD symptom subdimension at age 19: for inattentive symptoms, total IRR = 1.18, p = .009, 95% CI = [1.04, 1.35]; for hyperactive/impulsive symptoms, total IRR = 1.20, p = .001, 95% CI = [1.08, 1.33]. Both direct and indirect paths were evident in predicting inattentive symptoms, with the indirect path explaining 11.5% of the total effect (direct path IRR = 1.16, p = .025, 95% CI = [1.02, 1.32]; indirect path IRR = 1.02, p = .017, 95% CI = [1.00, 1.04]). A similar pattern was observed for hyperactive/impulsive symptoms, with the indirect effect accounting for 9.3% of the total effect (direct path IRR = 1.18, p = .003, 95% CI = [1.06, 1.31]; indirect path IRR = 1.02, p = .018, 95% CI = [1.00, 1.03]).
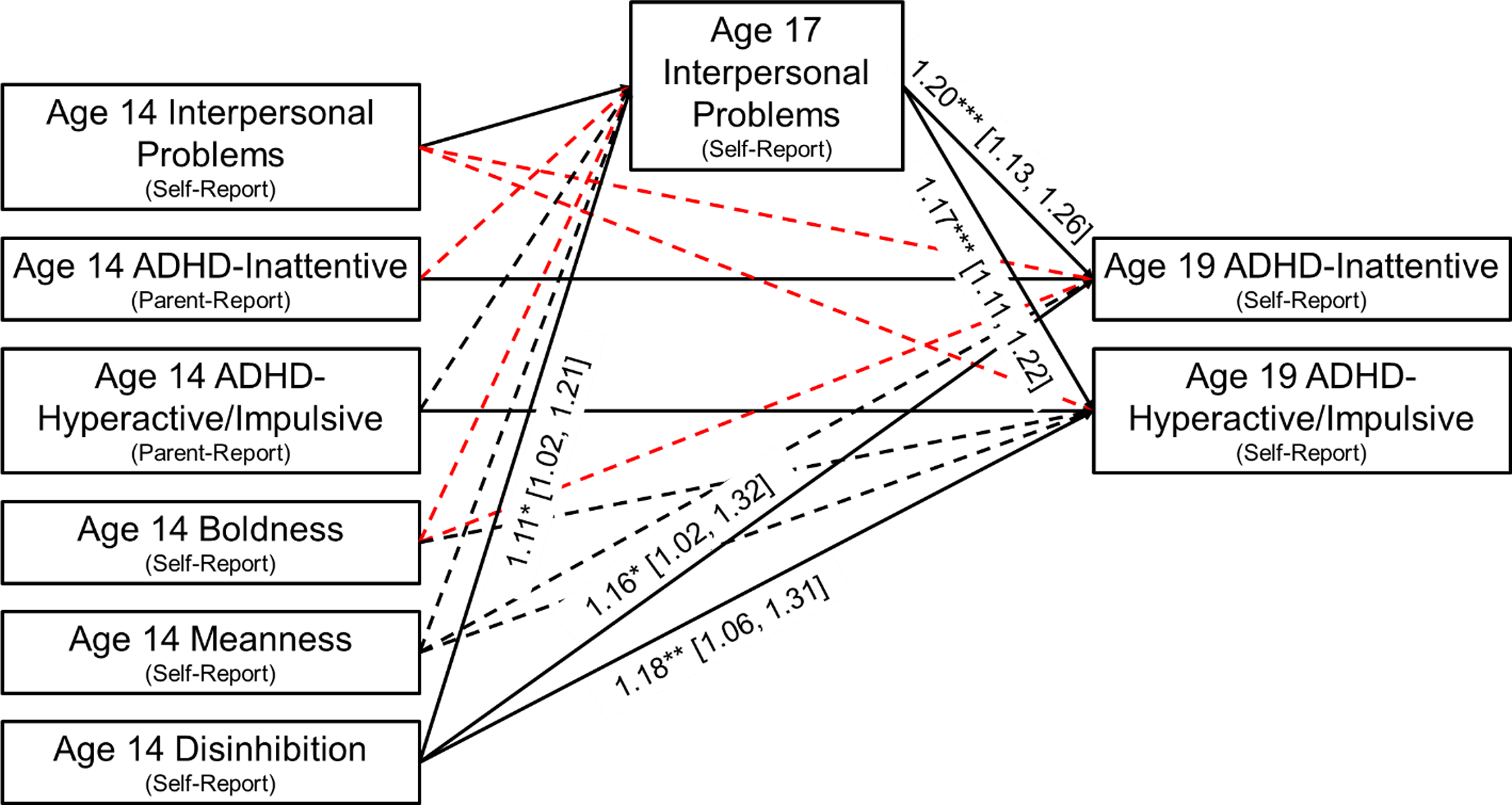
Figure 5. Prospective mediation model for ADHD subdimensions, controlling for age 14 symptoms and interpersonal problems. Path coefficients are incidence rate ratios (IRRs) from negative binomial regression models shown with [95% confidence intervals]. Standard errors are adjusted for within-family clustering. Negative paths are red and nonsignificant paths (p > .05) are dashed. Model n = 1,158. *p < .05, **p < .01, ***p < .001.
Aim 4: Sex moderation
To examine whether sex moderated any of the observed associations, Wald chi-square difference tests were conducted to compare models in which all regression coefficients were freed versus constrained to be equal across sex. For the concurrent model predicting total ADHD symptoms, constraining the parameters to be equal across sex did not significantly worsen model fit, χ2(3) = 4.33, p = .228, indicating that sex moderation was not present. In the prospective model, constraining the path coefficients across sex significantly worsened model fit, χ2(4) = 9.57, p = .048. When individual coefficients were constrained one by one, only the meanness path contributed to poor model fit, χ2(1) = 4.38, p = .036 (other paths’ χ2s(1) ≤ .01, ps ≥ .920). When all paths were allowed to vary freely, meanness showed a positive prospective association with total ADHD symptoms among girls (IRR = 1.20, p = .013, 95% CI = [1.04, 1.38]), but not boys (IRR = .97, p = .700, 95% CI = [.85, 1.11]). There was no evidence of sex moderation in the mediation model that included age 17 interpersonal problems (χ2(11) =16.19, p = .134).
In the concurrent model examining both ADHD subdimensions, constraining the path coefficients across sex significantly worsened model fit, χ2(6) = 17.52, p = .008. When individual coefficients were constrained one by one, the paths found to contribute to poor model fit were those from disinhibition to inattentive symptoms (χ2(1) = 6.42, p = .011) and from meanness to hyperactive/impulsive symptoms (χ2(1) = 5.03, p = .025; no other paths contributed significantly to reduced model fit, χ2s(1) ≤ .66, ps ≥ .416). When all paths were allowed to vary freely, disinhibition showed a stronger positive concurrent association with inattentive symptoms in females (IRR = 1.74, p < .001, 95% CI = [1.40, 2.17]) than in males (IRR = 1.23, p = .012, 95% CI = [1.05, 1.44]), and meanness showed a negative association with hyperactive/impulsive symptoms in females (IRR = .75, p = .040, 95% CI = [.57, .99]) but not males (IRR = 1.11, p = .301, 95% CI = [.91, 1.36]). By contrast, in the prospective model for ADHD subdimensions, no moderating effect of sex was observed, χ2(8) = 13.34, p = .101. Finally, there was evidence of sex moderation in the mediation models that included age 17 interpersonal problems and age 19 ADHD subdimensions, χ2(18) = 31.19, p = .027). When constraining the paths one by one, the only path contributing significantly to overall model degradation was that of age 14 inattentive symptoms to age 19 inattentive symptoms, χ2(1) = 4.48, p = .034 (all other paths’ χ2s(1) ≤ 2.86, ps ≥ .091), suggesting invariance for all paths of interest (i.e., those involving triarchic traits).
Discussion
The present study is the first to evaluate contributions of all three triarchic neurobehavioral traits (boldness, meanness, and disinhibition) to the persistence and severity of ADHD symptoms. Prior studies examining the triarchic traits in relation to ADHD have focused on disinhibition and meanness (or callous-unemotionality), finding disinhibition to be associated with general proneness to externalizing problems (Dotterer et al., Reference Dotterer, Waller, Cope, Hicks, Nigg, Zucker and Hyde2017; Yancey et al., Reference Yancey, Venables, Hicks and Patrick2013) including ADHD (Palumbo et al., Reference Palumbo, Patrick and Latzman2021; Pauli et al., Reference Pauli, Liljeberg, Gustavsson, Kristiansson and Howner2019; Perkins et al., Reference Perkins, Joyner, Foell, Drislane, Brislin, Frick, Yancey, Soto, Ganley, Keel, Sica, Flor, Nees, Banaschewski, Bokde, Desrivières, Grigis, Garavan, Gowland and Patrick2022; Young et al., Reference Young, Stallings, Corley, Krauter and Hewitt2000, Reference Young, Friedman, Miyake, Willcutt, Corley, Haberstick and Hewitt2009), and meanness to be related robustly to antisocial expressions of externalizing but less or negligibly to ADHD (Palumbo et al., Reference Palumbo, Patrick and Latzman2021; Perkins et al., Reference Perkins, Joyner, Foell, Drislane, Brislin, Frick, Yancey, Soto, Ganley, Keel, Sica, Flor, Nees, Banaschewski, Bokde, Desrivières, Grigis, Garavan, Gowland and Patrick2022; Sica et al., Reference Sica, Ciucci, Baroncelli, Frick and Patrick2020). Preliminary evidence for a significant but weak association of boldness with fewer ADHD-related problems was reported in two prior cross-sectional studies of children and adolescents (Palumbo et al., Reference Palumbo, Patrick and Latzman2021; Sica et al., Reference Sica, Ciucci, Baroncelli, Frick and Patrick2020). The current work adds to this existing literature by (a) utilizing data from a longitudinal study sample to elucidate risk as well as protective effects of the triarchic traits on ADHD symptomatology across periods of development from adolescence to emerging adulthood, and (b) testing for potential mediating and moderating effects of interpersonal difficulties and sex, respectively, on observed trait effects.
In line with hypotheses, a prospective analysis revealed a protective effect for boldness on ADHD symptoms, such that higher boldness at age 14 was associated with fewer overall ADHD symptoms at age 19. In contrast, a concurrent analysis revealed boldness at age 14 to be associated with greater ADHD severity at that age. These contrasting findings, while surprising, align with prior ADHD research indicating that detriments versus benefits conferred by an attribute may differ based on developmental stage (Mikami & Hinshaw, Reference Mikami and Hinshaw2006). For example, risk profiles among children with ADHD tend to change over time (Dvorsky & Langberg, Reference Dvorsky and Langberg2016; Hinshaw & Becker, Reference Hinshaw and Becker2020), and the very nature of ADHD-related difficulties evolves with development, with hyperactive/impulsive symptoms diminishing across time while inattention symptoms remain impairing into adulthood (Willcutt et al., Reference Willcutt, Nigg, Pennington, Solanto, Rohde, Tannock, Loo, Carlson, McBurnett and Lahey2012).
A potential explanation for the detrimental versus protective effects of boldness in the current study could lie in the distinct symptom clusters of ADHD and how they interface with demands arising at successive developmental stages. Specifically, during mid-adolescence, the fearless aspects of boldness may be expressed in impulsive behavior (Casey, Reference Casey2015), which would in turn elevate perceptions of ADHD-related hyperactive/impulsive symptoms in that age group (Biederman et al., Reference Biederman, Faraone, Hirshfeld-Becker, Friedman, Robin and Rosenbaum2001). By contrast, the interpersonally adaptive features of boldness (e.g., social poise and efficacy, emotional resilience; Green et al., Reference Green, Palumbo, Shishido, Kesner and Latzman2020; Lilienfeld et al., Reference Lilienfeld, Smith, Sauvigné, Patrick, Drislane, Latzman and Krueger2016; Neo et al., Reference Neo, Sellbom, Smith and Lilienfeld2018; Sica et al., Reference Sica, Ciucci, Baroncelli, Frick and Patrick2020) could be expected to mitigate the types of social impairments uniquely associated with the inattentive symptoms of ADHD that predominate as individuals enter adulthood, such as deficits in assertiveness (Solanto et al., Reference Solanto, Pope-Boyd, Tryon and Stepak2009), proneness to social withdrawal, and lack of leadership engagement (Marshall et al., Reference Marshall, Evans, Eiraldi, Becker and Power2014).
Consistent with this proposed explanation, we found that the positive cross-sectional association between boldness and ADHD symptoms was attributable to the hyperactive/impulsive dimension. Further, the protective effect of adolescent boldness on ADHD symptoms in early adulthood (age 19) was specific to the inattention dimension, though this relation became nonsignificant when controlling for early- (age 14) and mid-adolescent (age 17) interpersonal problems. A parsimonious explanation for this finding may be that individuals who are more interpersonally skilled at an early age acquire more boldness traits over time. Alternatively, adept social functioning and boldness may be intertwined in a complex manner across development, such that by the time of early adulthood, the former subsumes the latter and any prospective association of boldness with ADHD is entirely explained by higher levels of interpersonal functioning. This explanation accords with evidence indicating that boldness operates to attenuate problems in interpersonal functioning across different contexts, including with family and peers at earlier ages (Green et al., Reference Green, Palumbo, Shishido, Kesner and Latzman2020) and with work colleagues in adulthood (Kranefeld & Blickle, Reference Kranefeld and Blickle2022; Neo et al., Reference Neo, Sellbom, Smith and Lilienfeld2018). Relatedly, among youth with elevated ADHD inattention symptoms, higher levels of boldness may facilitate success in peer groups, as well as protect against adverse outcomes associated with peer rejection or loneliness (Green et al., Reference Green, Palumbo, Shishido, Kesner and Latzman2020). However, this idea is necessarily speculative, and future research with younger samples is needed to refine our understanding of whether adept interpersonal functioning predates boldness, or vice versa, among youth with ADHD inattention symptoms.
Our analyses further revealed that disinhibition predicted overall symptoms of ADHD as well as constituent hyperactive/impulsive and inattentive symptoms – both concurrently (at age 14) and prospectively (from 14 to 19). These findings align with prior reported associations of disinhibition with ADHD specifically and externalizing problems more broadly (Dotterer et al., Reference Dotterer, Waller, Cope, Hicks, Nigg, Zucker and Hyde2017; Palumbo et al., Reference Palumbo, Patrick and Latzman2021; Yancey et al., Reference Yancey, Venables, Hicks and Patrick2013; Perkins et al., Reference Perkins, Joyner, Foell, Drislane, Brislin, Frick, Yancey, Soto, Ganley, Keel, Sica, Flor, Nees, Banaschewski, Bokde, Desrivières, Grigis, Garavan, Gowland and Patrick2022; Sica et al., Reference Sica, Ciucci, Baroncelli, Frick and Patrick2020). Notably, the concurrent effect of disinhibition on inattention was found to be stronger for girls than boys. This finding is consistent with prior studies in which disinhibition was shown to predict ADHD symptoms regardless of sex (Hartung et al., Reference Hartung, Milich, Lynam and Martin2002; Milich et al., Reference Milich, Hartung, Martin and Haigler1994), though one study found stronger effects for boys versus girls aged 13–21 (Milich et al., Reference Milich, Hartung, Martin and Haigler1994). Nonetheless, studies focusing on disinhibition, sex, and inattention specifically, as opposed to ADHD symptoms more broadly, are limited, and thus further research is needed in this area. We additionally found that the positive prospective association between disinhibition and ADHD symptoms from age 14 to 19 was partially mediated by intervening interpersonal problems at age 17. This finding, observed for the ADHD total score and both symptom subdimensions, corroborates prior research indicating that impairments in inhibitory control – including difficulties in inhibiting inappropriate behavioral responses (Kipp, Reference Kipp2005) and regulating emotions (Wheeler & Carlson, Reference Wheeler Maedgen and Carlson2000) – are associated with difficulties in peer socialization among youth with ADHD (Bunford et al., Reference Bunford, Brandt, Golden, Dykstra, Suhr and Owens2015).
The triarchic trait of meanness was found to prospectively predict greater hyperactive/impulsive symptoms at age 19, with no evidence of sex differences in this association. However, in two other models, the multigroup analysis revealed that the nonsignificant overall effect of meanness masked significant effects for females only. Specifically, for females, meanness at age 14 was associated with fewer concurrent hyperactive/impulsive symptoms (p = .040), but prospectively with greater total symptoms of ADHD at age 19 (p = .013). These effects were nonsignificant for males (ps = .301 and .700). A previous study of adolescents found no evidence for sex differences in the meanness/ADHD association (Sica et al., Reference Sica, Ciucci, Baroncelli, Frick and Patrick2020), although separate symptom subdimensions were not examined. Interestingly, within a predominantly (∼2/3) male school-aged sample, Palumbo et al. (Reference Palumbo, Patrick and Latzman2021) found a small positive association between meanness and a dichotomous (present/absent) ADHD diagnosis that became negative when controlling for boldness and disinhibition. Although sex differences and symptom subdimensions were not tested in the study by Palumbo et al., their findings appear consistent with the current work in showing a weak negative association between the variance unique to meanness and ADHD, when measured concurrently. However, given that (1) female-specific effects regarding the meanness/ADHD association in the present sample were small and inconsistent across models, and (2) the effect for ADHD diagnosis found by Palumbo did not emerge for a continuous measure of total ADHD symptoms in the same sample, these findings should be considered tentative. More research is needed to clarify the nuanced developmental associations between meanness and ADHD symptoms in females.
Strengths, limitations, directions, and conclusions
Along with notable strengths, certain limitations of the current study warrant consideration. One strength of our study was the use of psychometrically validated measures for all constructs of interest. Despite the somewhat low reliability of the current study’s triarchic scales, the brevity of the scales and use of items from scales that are widely implemented in the developmental literature are notable. Further, prior research has demonstrated validity for these triarchic scale versions in relation to a variety of criterion measures (see Bertoldi et al., Reference Bertoldi, Perkins, Tuvblad, Oskarsson, Kramer, Latzman, Baker, Raine and Patrick2022). Nevertheless, it will be important for future work to undertake additional formal psychometric evaluation of these scales and refine them to address these potential limitations. Another strength was our use of continuous-score measures. Given that our primary aim was to examine whether the triarchic traits served as risk or protective factors for ADHD symptomatology over time, it was important to model symptom persistence at a more granular level than presence versus absence of a threshold diagnosis. Continuous symptom scores are more reliable and valid than dichotomous diagnoses (e.g., Markon et al., Reference Markon, Chmielewski and Miller2011) and thus are preferred in developmental psychopathology research. However, a potential limitation of our symptom counts is that they did not include indices of distress or impairment, as are required for a diagnosis of ADHD. Accordingly, it will be valuable in future research to examine longitudinal associations between triarchic traits and changes in ADHD-related functional impairment (see Perkins et al., Reference Perkins, Joyner, Foell, Drislane, Brislin, Frick, Yancey, Soto, Ganley, Keel, Sica, Flor, Nees, Banaschewski, Bokde, Desrivières, Grigis, Garavan, Gowland and Patrick2022). Relatedly, in the present study ADHD symptoms were parent-reported at age 14 and self-reported at age 17, and thus the significant but differential associations between boldness and ADHD across time points could be a product of differing reporter perspectives. The same could be true for the inconsistent evidence regarding sex moderation of associations between meanness and ADHD. Replication of study findings with consistent reporters across time is thus needed. Future research may also benefit from including measures from other response modalities (e.g., direct behavioral observation, electrophysiology) to operationalize the triarchic traits (cf. Patrick et al., Reference Patrick, Iacono and Venables2019) as well as ADHD-related impairments and interpersonal functioning. Moreover, future research may benefit from examining the triarchic traits and ADHD in singleton (i.e., non-twin/triplet) participants, who may experience different rearing conditions than twins/triplets. Furthermore, research on the facets of boldness at differing developmental stages may point to novel intervention targets for addressing the well-documented social impairments and affiliated adverse outcomes associated with ADHD. Similarly, although interpersonal problems were the focus of mediation analyses in the current work given their theoretical relevance to both triarchic traits and ADHD symptomatology, future studies should also investigate other functional difficulties commonly observed in ADHD, such as academic and occupational impairment.
Taken together, current study findings provide further evidence for a role of the triarchic traits not only in psychopathy, but also in relation to the externalizing spectrum more broadly, including ADHD in adolescence (Beauchaine et al., Reference Beauchaine, Zisner and Sauder2017; Martel et al., Reference Martel, Levinson, Lee and Smith2017; Perkins et al., Reference Perkins, Joyner, Foell, Drislane, Brislin, Frick, Yancey, Soto, Ganley, Keel, Sica, Flor, Nees, Banaschewski, Bokde, Desrivières, Grigis, Garavan, Gowland and Patrick2022). Importantly, our finding that later ADHD symptoms were predicted from earlier assessed triarchic traits when controlling for concurrent ADHD symptoms indicates that conceptual overlap between the triarchic traits and ADHD symptoms does not account for their observed associations. The implication is that the neurobehavioral traits of the triarchic model may offer some index of risk for the escalation of ADHD-related impairment, over and above what can be known by measuring early-emerging symptoms. Our pattern of results emphasizes the continued need for developmental psychopathology models and longitudinal studies that elucidate pathways to both psychopathology and adaptive outcomes in the study of neurobehavioral traits and ADHD, with implications for early identification and strengths-based interventions for youth with ADHD.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0954579423001608.
Acknowledgements
Elizabeth S.M. Chan, Ph.D. and Emily R. Perkins, Ph.D. are co first-authors.
Funding statement
The work reported in this article was supported by the Swedish Research Council (CT, 2018-01041), National Institute of Mental Health grant (ERP, F31MH122096), U.S. Army grant (CJP, W911NF-14-1-0018), and a MindCORE postdoctoral fellowship from the University of Pennsylvania (ERP). The University of Southern California Risk Factors for Antisocial Behavior twin study was supported by NIMH grant R01-MH58354. The content of this paper is solely the responsibility of the authors and does not necessarily reflect the official views of the Swedish government, the U.S. Government, National Institutes of Health, Department of Defense, Department of the Army, Department of Veterans Affairs, or U.S. Recruiting Command.
Competing interests
The authors declare none.









