Smoking is one of the leading public health problems in the world, killing about seven million people worldwide each year (WHO, 2018). In the Netherlands alone, about 20,000 people die due to tobacco-related diseases every year (RIVM, 2016). Despite a decrease in the number of Dutch smokers under 16 years of age, the number of young smokers between the ages of 16 and 25 has shown a small increase (CBS, 2016, 2017; internationally, there are similar smoking prevalence increases in this age group: US Department of Health and Human Services, 2014). It is therefore critical to invest in interventions to help youth quit smoking. In the remainder of this paper, when we refer to youth we specifically mean the group of adolescents and young adults between 16 and 25 years of age.
Young smokers have been largely overlooked in intervention research and policy building (Bader, Travis, & Skinner, Reference Bader, Travis and Skinner2007; McClure, Arheart, Lee, Sly, & Dietz, Reference McClure, Arheart, Lee, Sly and Dietz2013; Villanti, McKay, Abrams, Holtgrave, & Bowie, Reference Villanti, McKay, Abrams, Holtgrave and Bowie2010), as the major burden of smoking-related diseases falls on the adult population (Fanshawe et al., Reference Fanshawe, Halliwell, Lindson, Aveyard, Livingstone-Banks and Hartmann-Boyce2017). Yet, almost all smokers (98%) start smoking before the age of 26 years (US Department of Health and Human Services, 2012), and the percentage of effective self-initiated quit attempts among young people is extremely low. Without intervention very few young people quit smoking (Centers for Disease Control and Prevention, 2006; Fritz, Wider, Hardin, & Horrocks, Reference Fritz, Wider, Hardin and Horrocks2008; Lane, Leatherdale, & Ahmed, Reference Lane, Leatherdale and Ahmed2011; Mermelstein, Reference Mermelstein2003). Crucially, quitting smoking before the age of 30 reduces more than 97% of the lifelong health consequences related to smoking (Pirie et al., Reference Pirie, Peto, Reeves, Green and Beral2013; Thun et al., Reference Thun, Carter, Feskanich, Freedman, Prentice, Lopez and Gapstur2013).
A recent review on smoking cessation interventions specifically for young people demonstrated that there is not enough evidence to recommend one specific intervention model for youth (Fanshawe et al., Reference Fanshawe, Halliwell, Lindson, Aveyard, Livingstone-Banks and Hartmann-Boyce2017). Both in the Netherlands and worldwide, there are not many studies focusing on this at-risk group (Fanshawe et al., Reference Fanshawe, Halliwell, Lindson, Aveyard, Livingstone-Banks and Hartmann-Boyce2017; McClure et al., Reference McClure, Arheart, Lee, Sly and Dietz2013; Nationaal Expertisecentrum Tabaksontmoediging, 2013), and the available studies suffer from limitations such as no proven evidence-base, poor methodological design, or the lack of long-term effects (Fanshawe et al., Reference Fanshawe, Halliwell, Lindson, Aveyard, Livingstone-Banks and Hartmann-Boyce2017; Stockings et al., Reference Stockings, Hall, Lynskey, Morley, Reavley, Strang and Degenhardt2016; Towns, DiFranza, Jayasuriya, Marshall, & Shah, Reference Towns, DiFranza, Jayasuriya, Marshall and Shah2017; Villanti et al., Reference Villanti, McKay, Abrams, Holtgrave and Bowie2010). The limited evidence available seems to suggest that complex interventions that address a variety of mechanisms related to smoking among youth are most promising (Fanshawe et al., Reference Fanshawe, Halliwell, Lindson, Aveyard, Livingstone-Banks and Hartmann-Boyce2017; Gabble, Babayan, DiSante, & Schwartz, Reference Gabble, Babayan, DiSante and Schwartz2015). Most of these complex interventions include some sort of combination of a cognitive behavioral component, a motivational interviewing or enhancement component, a transtheoretical model of change component, and/or a social cognitive component, but some studies also include other elements such as meditation or acupressure. However, it remains unclear exactly which mechanism(s) drive observed effects and how these mechanisms could be effectively targeted (Fanshawe et al., Reference Fanshawe, Halliwell, Lindson, Aveyard, Livingstone-Banks and Hartmann-Boyce2017; Gabble et al., Reference Gabble, Babayan, DiSante and Schwartz2015; Waldron & Turner, Reference Waldron and Turner2008).
Barriers to Successful Smoking Cessation for Youth
Our lack of successful change in smoking behavior among young people is likely because of ineffective targeting of one of the most important predictors of youth's smoking initiation and continuation in interventions: peer influence (Dishion & Owen, Reference Dishion and Owen2002; Gabble et al., Reference Gabble, Babayan, DiSante and Schwartz2015; Goodnight, Bates, Newman, Dodge, & Pettit, Reference Goodnight, Bates, Newman, Dodge and Pettit2006; Kim, Fleming, & Catalano, Reference Kim, Fleming and Catalano2009; Liu, Zhao, Chen, Falk, & Albarracín, Reference Liu, Zhao, Chen, Falk and Albarracín2017). Substantial research has documented the profound effects of peer influence on youths’ development and well-being (Choukas-Bradley & Prinstein, Reference Choukas-Bradley, Prinstein, Lewis and Rudolph2014; Rubin, Bukowski, & Bowker, Reference Rubin, Bukowski, Bowker and Lerner2015), specifically for smoking behavior: youth are about twice as likely to initiate or continue smoking if their peers or friends smoke (Liu et al., Reference Liu, Zhao, Chen, Falk and Albarracín2017). Several intervention programs integrate peer influence processes in one way or another, such as by including social skill training that is directed at helping youth say no to smoking peers, by nonsmoking youth's giving support and advice to smoking youths, or by suggesting to spend less time with their smoking peers (Golechha, Reference Golechha2016; Sussman & Sun, Reference Sussman and Sun2009). These programs remain highly problematic, however, for several reasons: (a) the content is still solely targeted at the individual instead of a broader peer group (Gabble et al., Reference Gabble, Babayan, DiSante and Schwartz2015), (b) imbalanced relationships between the support giver and support taker are not helpful (Lenkens et al., Reference Lenkens, Rodenburg, Schenk, Nagelhout, Van Lenthe, Engbersen and Van De Mheen2019), and (c) these programs instigate high resistance among young smokers (Harakeh & Van Nijnatten, Reference Harakeh and van Nijnatten2016; Schenk et al., Reference Schenk, Sentse, Lenkens, Engbersen, van de Mheen, Nagelhout and Severiens2018; Wolburg, Reference Wolburg2006).
A second important barrier to successful smoking cessation among young people is the difficulties that are encountered with recruiting and retaining youth that might benefit from intervention programs (Villanti et al., Reference Villanti, McKay, Abrams, Holtgrave and Bowie2010). A key underlying reason for these recruitment and retention issues are youths’ difficulties in finding resources and services that they find initially engaging and relevant to their needs and that will support them in a way that suits their preferences and modes of learning (Bader et al., Reference Bader, Travis and Skinner2007; Scholten & Granic, Reference Scholten and Granic2019). Young smokers are a highly heterogeneous group; not only do they differ greatly in their reasons to smoke and to quit but also in their backgrounds (McClure et al., Reference McClure, Arheart, Lee, Sly and Dietz2013; Moran, Wechsler, & Rigotti, Reference Moran, Wechsler and Rigotti2004). For example, youth often define themselves as “occasional” or “social” smokers instead of daily smokers (McClure et al., Reference McClure, Arheart, Lee, Sly and Dietz2013; Moran et al., Reference Moran, Wechsler and Rigotti2004). Yet, these occasional or social smokers are usually not invited for smoking cessation interventions, which is problematic because intermittent smoking can lead to escalation to established smoking (Berg & Schauer, Reference Berg and Schauer2012; McDermott, Dobson, & Owen, Reference McDermott, Dobson and Owen2007; White, Bray, Fleming, & Catalano, Reference White, Bray, Fleming and Catalano2009).
Furthermore, youth from lower educational backgrounds are equally likely to attempt to quit smoking as their higher educated counterparts, but they are less successful and drop out of intervention programs much more often (Hill, Amos, Clifford, & Platt, Reference Hill, Amos, Clifford and Platt2014; Hiscock, Bauld, Amos, Fidler, & Munafò, Reference Hiscock, Bauld, Amos, Fidler and Munafò2012; Kotz & West, Reference Kotz and West2009; McCarthy, Siahpush, Shaikh, Sikora Kessler, & Tibbits, Reference McCarthy, Siahpush, Shaikh, Sikora Kessler and Tibbits2016; Springvloet, Kuipers, & Van Laar, Reference Springvloet, Kuipers and Van Laar2017). Therefore, smoking cessation researchers should try to include a heterogeneous group of young smokers in cessation trials. Moreover, a one-size-fits-all approach, which ignores the different needs and motivations among young smokers, is probably not going to have a major reach among this heterogenous group of youth (Carlson, Widome, Fabian, Luo, & Forster, Reference Carlson, Widome, Fabian, Luo and Forster2018). Taken together, the lack of targeting peer influences and the mismatch between the design of intervention programs and the needs of young people strongly suggest that novel approaches are critical to engaging young smokers in cessation interventions (McClure et al., Reference McClure, Arheart, Lee, Sly and Dietz2013; Thrul & Ramo, Reference Thrul and Ramo2017).
Intervention Development
The initiation, continuation, and cessation of smoking behavior is influenced by several mechanisms including individual (e.g., psychological, cognitive) and contextual (e.g., social) mechanisms. These mechanisms interact with each other in a complex and multidimensional way (Unger et al., Reference Unger, Cruz, Baezconde-Garbanati, Shakib, Palmer, Johnson and Glynn2003). The foundation of the current study was inspired by Tom Dishion's seminal work on peer influence processes. A transactional model by Wills and Dishion (Reference Wills and Dishion2004) accounts for the potential interaction between self-control, as individual mechanism, and peer influence, as contextual mechanism, on youths’ substance use. In a previous study, we developed a game to train inhibitory control through a modified version of a Go/No-Go training (Lawrence et al., Reference Lawrence, O'Sullivan, Parslow, Javaid, Adams, Chambers and Verbruggen2015; Veling, Van Koningsbruggen, Aarts, & Stroebe, Reference Veling, van Koningsbruggen, Aarts and Stroebe2014) to help youth quit smoking. The goal of that study was to test the effects of the training on smoking-specific inhibitory control and perceived attractiveness of smoking stimuli and its possible contributions to smoking cessation. Although we found promising effects on the devaluation of smoking-related stimuli through Go/No-Go training, we found no positive effect on smoking cessation (Scholten, Luijten, Poppelaars, Johnson-Glenberg, & Granic, Reference Scholten, Luijten, Poppelaars, Johnson-Glenberg and Granicunder review). We believe that the lack of effects on smoking behavior could be tackled by dealing with the two barriers in intervention design described before: the inclusion of peer processes and improvements in game design to increase engagement, making the game feel relevant and fun to youth.
Peer processes
Social interactions take on increased importance in adolescence (Crone & Dahl, Reference Crone and Dahl2012) and often provide the context in which youth start to engage in risky behaviors, such as substance use (Dishion & Owen, Reference Dishion and Owen2002). These risky behaviors are often the consequence of a process called peer contagion, conceptualized as a mutual influence process between peers that includes behaviors and emotions that potentially undermine one's own development or cause harm to others (Dishion & Tipsord, Reference Dishion and Tipsord2011). Peer contagion works through positive reinforcement between peers: actions or dialogues that elicit a positive response from peers increase in frequency (Dishion & Snyder, Reference Dishion and Snyder2016). Indeed, a wealth of research shows that affiliation with deviant peer groups is related to increases in aggression and an amplification of problem behaviors, including substance use (Dishion & Tipsord, Reference Dishion and Tipsord2011). Yet, these precise peer contagion processes can also be harnessed to support, amplify, and maintain positive behavioral change. Consistent with principles of developmental psychopathology more generally, youths’ peer relationships offer unique contributions for the introduction of support and close bonds, and these relationships serve as resources that boost youths’ competence as well as a buffer against stress (Dishion & Patterson, Reference Dishion, Patterson, Cicchetti and Cohen2006). In particular, we propose that peer contagion processes can be positively exploited to support young people who are attempting to quit smoking.
If we are able to infiltrate peer systems and instantiate positive peer contagion processes, this supportive context could trigger long lasting change for youth (Dishion & Patterson, Reference Dishion, Patterson, Cicchetti and Cohen2006; Dishion & Snyder, Reference Dishion and Snyder2016). A particularly promising way to infiltrate the peer system is through social digital technologies (i.e., social media, YouTube, mobile games etc.), given that these are the ubiquitous contexts currently being used for peer interaction, identity exploration, and social norm creation (Boyd, Reference Boyd2014; Ehrenreich & Underwood, Reference Ehrenreich, Underwood, Dishion and Snyder2016; McFarland & Ployhart, Reference McFarland and Ployhart2015; Peter & Valkenburg, Reference Peter, Valkenburg and Valdivia2013; Prinstein & Giletta Reference Prinstein, Giletta and Cicchetti2016; Subrahmanyam & Smahel, Reference Subrahmanyam and Smahel2010). Youth are connected with their peers instantaneously and continuously through interactive media, and this near-constant access provides an enormous amount of time for both positive and negative reinforcement processes to take hold (for reviews, see Lenhart, Reference Lenhart2015a; Lenhart, Reference Lenhart2015b; Nesi, Choukas-Bradley, & Prinstein, Reference Nesi, Choukas-Bradley and Prinstein2018). Indeed, the features of digital media provide unique opportunities to rapidly disseminate content, to promote positive norms among peers, and to reach youth who feel stigmatized or do not connect with traditional forms of prevention or intervention (Nesi et al., Reference Nesi, Choukas-Bradley and Prinstein2018).
To our knowledge, an intervention that attempts to infiltrate the broader peer system through interactive media for the purposes of supporting smoking cessation has not been done before. The current study was directed at designing and testing a social mobile game intervention that brought together like-minded youth who wanted to quit smoking, incorporating both cooperative and competitive team-based gameplay. Within their teams, participants publicly committed to quitting smoking, communicated with each other about their team performance, encouraged each other to participate, and supported each other's quit attempts.
Engagement processes
To address the mismatch between intervention programs and the needs of young people, we developed our intervention following design thinking principles and through a participatory process (Scholten & Granic, Reference Scholten and Granic2019). By recruiting smoking youth from the outset of the design process and by finding out how these youth interact and seek information, we have a better chance of understanding their situation and designing an intervention that facilitates engagement, retains attention, and matches their needs (Boyd, Reference Boyd2014). Specifically, we ran focus groups with a diverse group of smoking youth, iterated on several versions of the game, and employed play testing, leading us to two key lessons.
First, we learned that there is a common misconception that youth do not want to quit smoking because they just started smoking and they are uninformed about the health consequences of smoking. However, research indicates that young people are just as motivated to quit as adults are (Ramo et al., Reference Ramo, Thrul, Delucchi, Hall, Ling, Belohlavek and Prochaska2018), yet they are less likely to use the available adult evidence-based smoking cessation interventions (e.g., nicotine replacement therapy, medication, counseling, quit lines), instead trying to quit on their own (Curry, Sporer, Pugach, Campbell, & Emery, Reference Curry, Sporer, Pugach, Campbell and Emery2007; Fiore et al., Reference Fiore, Jaén, Baker, Bailey, Benowitz and Curry2008; Solberg, Asche, Boyle, McCarty, & Thoele, Reference Solberg, Asche, Boyle, McCarty and Thoele2007; Thrul & Ramo, Reference Thrul and Ramo2017). Indeed, young people value self-reliance and self-sufficiency (Lenkens et al., Reference Lenkens, Rodenburg, Schenk, Nagelhout, Van Lenthe, Engbersen and Van De Mheen2019; Schenk et al., Reference Schenk, Sentse, Lenkens, Engbersen, van de Mheen, Nagelhout and Severiens2018), which require both the capability of insight into your own situation and needs and the availability of social capital (Lauriks et al., Reference Lauriks, de Wit, Buster, Fassaert, van Wifferen and Klazinga2014). Therefore, most youth expressed the desire to quit smoking using their own strength (Bader et al., Reference Bader, Travis and Skinner2007; Lenkens et al., Reference Lenkens, Rodenburg, Schenk, Nagelhout, Van Lenthe, Engbersen and Van De Mheen2019; Schenk et al., Reference Schenk, Sentse, Lenkens, Engbersen, van de Mheen, Nagelhout and Severiens2018) and they wanted help with their quit attempt, but not when this advice was didactic, outdated, or boring (Bader et al., Reference Bader, Travis and Skinner2007).
Second, we discovered that there was a great deal of variability in terms of where and when young people chose to smoke, suggesting the importance of tailoring an intervention to youth's individual preferences. We learned that smoking served several functions: to cope with stress, to overcome boredom during the day (e.g., waiting for the bus) and, crucially, to socialize with friends during breaks. Many youth felt captivated by their smoking addiction, and although they knew that most smoking moments were driven by habitual behavior, they could not distract themselves from their feelings of craving.
From these conversations with youth, we designed a game intervention to serve as a functional replacement for the smoking habit that could be played on a mobile phone during individualized moments of high craving. Both distraction from feelings of craving (Kong, Ells, Camenga, & Krishnan-Sarin, Reference Kong, Ells, Camenga and Krishnan-Sarin2014; Ploderer, Smith, Pearce, & Borland, Reference Ploderer, Smith, Pearce and Borland2014; Whittaker, McRobbie, Bullen, Rodgers, & Gu, Reference Whittaker, McRobbie, Bullen, Rodgers and Gu2016) and tailoring an intervention to individual preferences (An et al., Reference An, Klatt, Perry, Lein, Hennrikus, Pallonen and Ehlinger2008; Kong et al., Reference Kong, Ells, Camenga and Krishnan-Sarin2014; Villanti et al., Reference Villanti, McKay, Abrams, Holtgrave and Bowie2010; Whittaker et al., Reference Whittaker, McRobbie, Bullen, Rodgers and Gu2016; Zanis et al., Reference Zanis, Hollm, Derr, Ibrahim, Collins, Coviello and Melochick2011) are practices that are helpful and recommended for effectively quitting smoking.
Design and Hypotheses
In the present preregistered, two-armed randomized controlled trial (RCT) we examined the effects of HitnRun, a social mobile game, among young smokers who were motivated to quit smoking. We targeted young smokers ranging from 16 to 26 years of age, with a specific focus on youth between 16 and 18. In the Netherlands, youth from this subgroup are often excluded from research because it is legally forbidden for people under the age of 18 years to purchase tobacco. In addition, many youth between 16 and 18 do not tell their parents that they smoke, yet previous Dutch legislation necessitated parental consent for participation of youth under 18. This legislation changed just after we started recruitment; therefore, we updated our IRB approval to include participants between 16 and 18 years of age, without the necessity of parental consent. Furthermore, we tried to include a diverse group of young people, ranging from light, intermittent smokers to heavy, dependent smokers (McClure et al., Reference McClure, Arheart, Lee, Sly and Dietz2013; Villanti et al., Reference Villanti, McKay, Abrams, Holtgrave and Bowie2010) and ranging from lower educational to higher educational backgrounds (Hiscock et al., Reference Hiscock, Bauld, Amos, Fidler and Munafò2012; Springvloet et al., Reference Springvloet, Kuipers and Van Laar2017). A psychoeducational brochure, which is a common intervention for smoking cessation that does not include any components actively targeted in HitnRun (Boot, Simons, Stothart, & Stutts, Reference Boot, Simons, Stothart and Stutts2013), was selected as the active control intervention. We examined the effects of HitnRun compared with those of the psychoeducational brochure on participants’ weekly smoking behavior and abstinence rates at pretest, post-test, and three-month follow-up.
We expected that the game group would show larger decreases in weekly smoking behavior and higher abstinence rates at post-test and three-month follow-up than the brochure group. In addition, we expected that we would find a dose-response effect in the game group: the more time spent playing the game the larger the decrease in weekly smoking behavior. Furthermore, based on Tom Dishion's social reinforcement and contagion research, we tried to harness the power of the peer system and its potential to support change processes by including a text-based, peer support component to HitnRun. Our preliminary, and modest, goal at this early stage was to track how youth naturally used and navigated through our digital intervention, with a specific focus on the peer-based support opportunities and engagement properties of HitnRun. We did not have the resources to build a fully integrated communication system in HitnRun; therefore, we resorted to the Google Hangouts function on participant's mobile phones that they were encouraged to use to communicate with their team members. These team-based conversations were expected to be a rich source of information for exploring the effects of our peer-based design on intervention dose and smoking behavior. Our intention was to use simple, text-based analytic methods to investigate whether the frequency of communication with each other, as well as the use and frequency of certain types of words (e.g., emotion words), would be related to outcomes.
Because HitnRun has never been evaluated or implemented, we also collected intervention evaluation measures to understand whether our engagement goals were met and to inform further iterations of the game. In order to consider the design of HitnRun successful, HitnRun should have been able to engage youth; otherwise, our rationale for using design thinking and participatory design principles is lost. We hypothesized that participants in the game group would rate the game more favorably after intervention than the brochure group. In addition, we predicted that, within the game group, higher game evaluation scores would be related to a higher dose of gameplay and a larger decrease in smoking behavior over time.
Materials and Methods
Participants
Youth were recruited through flyers on campus and through online advertisements on Facebook and Instagram. We also recruited through high schools and vocational education institutions and administered screening questionnaires with active consent from participating youth. Our electronic screening questionnaire included questions about smoking frequency and quantity, environmental smoking, motivation to quit, demographics, questions related to the exclusion criteria, and if participants wanted to, their contact details. Screening data were collected between April 2017 and May 2018, before and during the intervention. Study inclusion criteria included the following: (a) aged 16 to 26 years, (b) at least a weekly smoker, (c) motivated to quit smoking for at least four weeks during study participation (Prochaska et al., Reference Prochaska, Velicer, Rossi, Goldstein, Marcus, Rakowski and Rossi1994), and (d) willing to give informed consent. Exclusion criteria included (a) taking psychotropic drugs and (b) receiving psychosocial care.
When participants were between 16 and 18 years of age, we asked if their parents were aware of their smoking. If yes, we asked for their permission to talk to their parents and inform them about the study. If no, we encouraged youth to talk to their parents about their smoking behavior and participation in the current study. Yet, we did not force youth to tell their parents about their smoking behavior, neither did we exclude them from the study as formally we did not need parental consent for youth 16 years and older. We got explicit permission from the ethical committee for this procedure, as we found it important to include this vulnerable group of youth. In the Netherlands, it is legally forbidden for people under 18 years of age to purchase tobacco, so many youth between 16 and 18 do not tell their parents that they smoke, which results in youth from this subgroup often being excluded from research.
In total, 144 young people (54.9% females) took part in the study, with a mean age of 19 (M age = 19.39; SD age = 2.52; range = 16–27). The sample included more participants with a lower education level (56%) than with a higher education level (44%). Participants smoked at least one day per week (M = 6.18, SD = 1.55, range = 1–7), and smoked on average 71 cigarettes per week (M = 70.63, SD = 47.82, range = 1–252). Fagerström scores (FTND) were suggestive of moderate levels of nicotine dependence, M = 2.72, SD = 2.16, range = 0–10 (Heatherton, Kozlowski, Frecker, & Fagerstrom, Reference Heatherton, Kozlowski, Frecker and Fagerstrom1991; Vink, Willemsen, Beem, & Boomsma, Reference Vink, Willemsen, Beem and Boomsma2005). Finally, 63% of the participants had attempted to quit smoking before, with an average of 2.91 quit attempts (M = 2.91, SD = 2.44, range = 0–16). All participant characteristics are displayed in Table 1.
Table 1. Participant characteristics and outcome variables per group at pretest

Sample size
Based on an a priori power analysis using G*Power 3, the target sample size was set at 128 participants (Faul, Erdfelder, Lang, & Buchner, Reference Faul, Erdfelder, Lang and Buchner2007; repeated measures analysis of variance (ANOVA), between subjects design; η2 = 0.06, α = 0.05, power = 0.80). In total, 144 young people were enrolled in the study, allowing for 10% attrition.
Randomization
A blocked randomization scheme was used, as we randomized 12 participants to one intervention cohort that started the intervention at the same day and time. Randomization of the cohorts was performed by an independent researcher using random number generation. The intervention scheme was (0 = brochure intervention; 1 = game intervention): 0, 1, 0, 1, 1, 0, 0, 1, 0, 1, 0, 1.
Procedure
Data were collected at the Behavioural Science Institute Laboratory of Radboud University. Participants were asked to refrain from smoking at least one hour before the start of the first lab visit (i.e., pretest). At the first lab visit, participants provided informed consent and were randomized into either the game group (n = 72) or the brochure group (n = 72). Test procedures lasted approximately 120-–180 minutes, with a number of neurocognitive and EEG measures that were administered as part of a larger research project. The current study focused on the outcomes to assess intervention effectiveness, dose-response effects, and peer influence and engagement factors.
After all testing procedures, participants received an explanation of the intervention they were randomly assigned to. Participants in the brochure group were instructed to read the brochure at least once at home during the intervention period, and they were reminded halfway through the intervention period to engage with the intervention via a personalized email. Participants in the game group were instructed to play the game at least once per day for 2 to 5 minutes, and they received tailored prompts to keep them engaged with the intervention and remind them of the purpose of the game. The official start of the intervention period of four weeks was determined by the inclusion of twelve participants in one cohort; after twelve participants visited the lab the complete group was informed about their official quit day with at least a four day notice. All twelve participants in one cohort quit smoking together at their official quit date. Participants were allowed to use other smoking cessation aids to help them stay abstinent during their quit attempt; we asked them to report on these aids at post-test. Nine participants reported to have used other aids during their quit attempt, ranging from food-related replacements (lollipops or other candy, oranges, chewing gum; n = 4), shisha pens (without nicotine; n = 2), or nicotine replacement aids (e-cigarette or nicotine patches; n = 3)Footnote 1.
After the four week intervention period, participants came to the lab for the second time (i.e., post-test) and completed the same procedure as at the pretest (with the exception that we added some reading/playing frequency and evaluation questions to the questionnaire, to get insights about engagement with intervention materials). Three months after the second lab visit, participants received a digital questionnaire at home for follow-up assessment. After filling out the three-month follow-up questionnaire, participants received course credits or a €60 gift certificate for their participation. Pretest and post-test data were collected between September 2017 and August 2018. Follow-up data were collected between January and October 2018. The current study was approved by the ethics committee of the faculty of social sciences at Radboud University (ECSW2017-1303-487; Amendment: ECSW-2017-001) and registered at the Dutch Trial Register (No. NTR6706).
Loss to follow-up
At pretest, 144 youth took part in the study (see Figure 1). The response rate for the post-test in the lab was 91% (n = 131). Of the thirteen youth who did not show up for post-test, two had been randomized to the game group and eleven to the brochure group. Although these thirteen people did not visit the lab at post-test, four of them still filled out the questionnaire part of this study at home (n = 135, response rate = 94%). Two of those participants had been randomized to the game group and two to the brochure group. The response rate for the three-month follow-up was 97% (n = 135). Of the five participants who did not complete the three-month follow-up questionnaires at home, zero had been randomized to the game group and five to the brochure group. Of the nine youth who did not fill out the post-test questionnaire, four did fill out the three-month follow-up questionnaire.

Figure 1. Flow of participants through trial.
Attrition analyses were conducted to examine whether youth who stayed in the study and completed the follow-up assessment differed with respect to sex, age, education, study condition, and baseline weekly smoking levels from youth who were lost to follow-up. Logistic regression analyses with loss to follow-up as the dependent variable showed no differences for sex (p = .403), age (p = .256), education (p = .988), study condition (p = .997), and baseline weekly smoking levels (p = .472).
Interventions
Game
The current version of the social mobile game HitnRun is the second iteration of this game, and it is based on a genre that is usually referred to as a “runner” game. In runner games, players control an avatar that is running forward continuously while collecting points along the way by moving the character up-and-down or left-to-right. The first iteration of HitnRun was fully focused around principles of Go/No-Go training (Lawrence et al., Reference Lawrence, O'Sullivan, Parslow, Javaid, Adams, Chambers and Verbruggen2015; Veling et al., Reference Veling, van Koningsbruggen, Aarts and Stroebe2014), and it was tested for its effects on inhibitory control and evaluation of smoking stimuli (Scholten et al., Reference Scholten, Luijten, Poppelaars, Johnson-Glenberg and Granicunder review) and food stimuli (Poppelaars et al., Reference Poppelaars, Scholten, Granic, Veling, Johnson-Glenberg and Luijten2018). In the second iteration of HitnRun, we stuck to the integration of Go/No-Go training because we found promising decreases in evaluations of smoking stimuli over time in the game group compared with the brochure group (Scholten et al., Reference Scholten, Luijten, Poppelaars, Johnson-Glenberg and Granicunder review). In addition, we added features to the game to ‘infiltrate’ the peers system and to maximize engagement processes. The most important features of the current version of HitnRun are described below (see Figure 2).
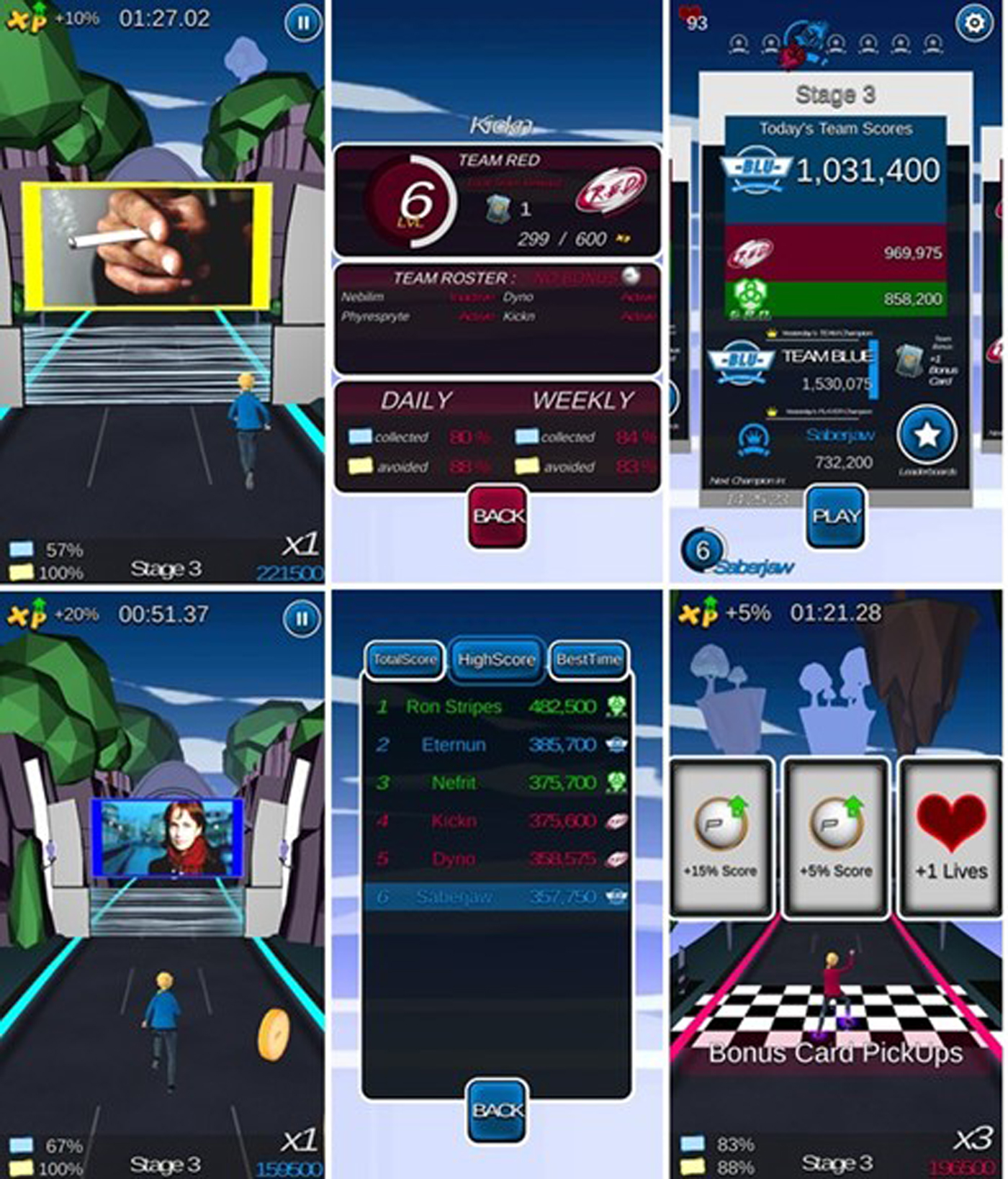
Figure 2. Screenshots HitnRun game play.
We altered the delivery mode of HitnRun to accommodate a mobile platform. Mobile phones offer resources for coping in high-risk situations when quitters may be tempted to relapse, as support is available at any time and place (Whittaker et al., Reference Whittaker, McRobbie, Bullen, Rodgers and Gu2016). We wanted HitnRun to serve as a functional replacement for participants’ smoking habit psychologically and physically (i.e., keeping their hands busy; Struik, Bottorff, Baskerville, & Oliffe, Reference Struik, Bottorff, Baskerville and Oliffe2018). Therefore we needed a method of delivery that was flexible, portable, and relevant. Smoking is triggered for a variety of reasons such as boredom, stress, or being in the company of smoking friends (McClure et al., Reference McClure, Arheart, Lee, Sly and Dietz2013); thus, we designed the game to be played during individualized moments of high craving, stress, or boredom. The runner genre lends itself perfectly for short bursts of intensive gameplay (i.e., 3–5 minutes per session), which is also the approximate time it takes to overcome a craving moment or to smoke a cigarette (O'Connell et al., Reference O'Connell, Gerkovich, Cook, Shiffman, Hickcox and Kakolewski1998). During the pretest, we put emphasis on this information: participants were specifically told that these moments only take a short while and that distracting yourself during those moments helps overcome craving. Furthermore, we designed tailored prompts that reminded users to play when they were suffering from high levels of craving.
These tailored prompts were constructed for each individual separately and relied on three sources of information. Participants filled out a craving diary in which they indicated at what exact moments during each week and weekend day they experienced high levels of craving and why. In addition, we asked participants for their top three motivations to quit smoking and wrote them down for them. Finally, we primed the participants to think about their future self as a nonsmoker and the benefits related to that (Scholten, Scheres, De Water, Graf, Granic, & Luijten, Reference Scholten, Scheres, De Water, Graf, Granic and Luijten2019). These motivations and future benefits were used in combination with the craving diary information at the pretest in composing the tailored prompts that were sent to participants once or twice a day during the first two weeks. As we expected craving levels to go down over intervention time (Struik et al., Reference Struik, Bottorff, Baskerville and Oliffe2018), the participants received fewer emails during the last two intervention weeks.
In addition, we tried to take advantage of the effects of peer influence on smoking behavior in a supporting and reinforcing way by using game-based experiences that were fundamentally interactive. We brought youth together with like-minded peers who were motivated to quit. Participants were rewarded for prosocial instead of antisocial behaviors by using cooperative team-based gameplay; all participants were member of a team of four people. We applied “friendly” peer pressure in playful nudges to encourage players to engage with the game, thereby implicitly reminding participants they were all quitting together. Specifically, each day a bonus could be obtained that was contingent on the participation of all team members, when one or more team members did not play, no bonus was given. Competitive team play elements were added to keep up motivation, commitment, and engagement, without our having to resort to didactic or stigmatizing scare tactics. There were three teams of four members competing against each other who all had the same quit date (they belonged to the same cohort of 12 participants).
Within teams, players could communicate with each other through the Google hangouts function on their mobile phone. Participants were instructed at the pretest to use this function to motivate their fellow team members to play the game and to seek and give support regarding their quit attempt. On average participants played the game 18.86 times (SD = 11.48; range = 0–60); in total, they played 114.26 minutes (SD = 106.07; range = 0–450) over all play sessions.
Brochure
The freely available self-help brochure Wat je zou moeten weten over stoppen met roken (What you should know about quitting smoking) by the Trimbos Instituut (2014) was provided to participants in the brochure group. This brochure, designed for the general public, seeks to optimally prepare individuals for a quit attempt by addressing the benefits of quitting smoking, describing the withdrawal symptoms individuals will probably encounter and how to cope with these, providing references to specialist support, and supporting methods such as nicotine replacement therapy. Participants received a digital version of this 16-page brochure on the day before their official quit day, to read at least once in the intervention period and more often if they wanted to. On average participants read the brochure 2.52 times (SD = 1.19; range = 1–6).
Measures
Weekly smoking behavior
Weekly smoking behavior was assessed at pretest, post-test, and three-month follow-up by multiplying the values for responses to two questions: a question measuring the number of smoking days (“How many days per week do you smoke on average?”) and a question measuring smoking quantity per day (“On a day that you smoke, how many cigarettes do you smoke on average? I smoke approximately __ cigarettes a day.”)
Abstinence
Abstinence was assessed at post-test and three-month follow-up by the question: “Have you smoked in the last 24 hours, even if it was just one puff?” Participants could answer this question with yes (1) or no (0).
Intervention dose
At post-test, participants estimated the number of minutes that they spent reading the brochure or playing the game (dose). Specifically, they answered the following question: “How many minutes in total did you spend reading the brochure/playing the game?” Participants could respond by typing in a number representing the dose of reading the brochure/playing the game. Based on a median split, we created a dichotomous variable indicating either a low or. high dose of reading/play sessions (i.e., hereafter referred to as dose). In the brochure group the median for dose was 30 (n low = 42; n high = 19), and for the game group the median for dose was 80 (n low = 37; n high = 35).
Text-based analyses—game group only
Participants in the game group could communicate with each other by using the Google hangouts function. The textual hangouts data for all participants in the 18 groups was saved and used for analysis with a computerized text analysis program, Linguistic Inquiry and Word Count (LIWC2015; Pennebaker, Boyd, Jordan, & Blackburn, Reference Pennebaker, Boyd, Jordan and Blackburn2015). Linguistic Inquiry and Word Count has been shown to be a reliable and valid method for measuring psychological constructs, particularly emotion (Tausczik & Pennebaker, Reference Tausczik and Pennebaker2010). A complete list of the standard LIWC2015 scales can be found in the supplementary materials or in the article by Pennebaker and colleagues (Reference Pennebaker, Boyd, Jordan and Blackburn2015).
For our purposes, we extracted the data from LIWC2015 on a group level and fed that into SPSS to relate the textual data to our outcome variables, weekly smoking behavior and the dose of game play. Although LIWC2015 can analyze text along more than 90 linguistic dimensions, several categories were excluded from the present analyses. First, variables were excluded from all subsequent analyses if they were not expected to be relevant in the current study (Newman, Pennebaker, Berry, & Richards, Reference Newman, Pennebaker, Berry and Richards2003). Second, any linguistic variables that were used at extremely low rates (less than 0.2% of the time) were excluded (Newman et al., Reference Newman, Pennebaker, Berry and Richards2003). For example, we were interested in the results related to the categories future focus, money, death, and friend, but these categories had base rates that were too low to be interpreted. Therefore, the final list of variables that were used in the analysis was reduced to eleven variables.
We were specifically interested in (a) the overall word count (M = 234; SD = 440.13), as previous work on small groups or communities suggests that group cohesion increases if more words are used (Leshed, Hancock, Cosley, McLeod, & Gay, Reference Leshed, Hancock, Cosley, McLeod and Gay2007). In turn, higher group cohesion is related to better outcomes (Tamersoy, Chau, & De Choudhury, Reference Tamersoy, Chau and De Choudhury2017; Tausczik & Pennebaker, Reference Tausczik and Pennebaker2010); (b) emotional tone, as positive affect words are associated with low risk of smoking relapse (Murnane & Counts, Reference Murnane and Counts2014; Tamersoy et al., Reference Tamersoy, Chau and De Choudhury2017); (c) first person singular pronouns, as first person singular pronouns are associated with high risk of smoking relapse (Tamersoy et al., Reference Tamersoy, Chau and De Choudhury2017); (d) first person plural pronouns, as group cohesion increases if more first person plural pronouns are used (the “we can do this” feeling; Sexton & Helmreich, Reference Sexton and Helmreich2000); (e) second person pronouns, as lower use of second person pronouns is indicative of lowered social interaction with the greater community and linked to increased risk of relapse (Tamersoy et al., Reference Tamersoy, Chau and De Choudhury2017); (f) impersonal pronouns, as impersonal pronouns might indicate distancing oneself from their internal state (Collins et al., Reference Collins, Chawla, Hsu, Grow, Otto and Marlatt2009); (g) social, as the use of social words is related to better team cohesion (Neubauer, Woolley, Khooshabeh, & Scherer, Reference Neubauer, Woolley, Khooshabeh and Scherer2016); (h) affiliation, as affiliation is seen as an indicator of identification with the community one belongs too (Best, Bliuc, Iqbal, Upton, & Hodgkins, Reference Best, Bliuc, Iqbal, Upton and Hodgkins2018); (i) focus past, as past tense words are associated with low risk of smoking relapse (Tamersoy et al., Reference Tamersoy, Chau and De Choudhury2017); (j) focus present, as the use of present tense words is associated with high risk of smoking relapse (Tamersoy et al., Reference Tamersoy, Chau and De Choudhury2017); (k) assent, as group cohesion increases if more assent words are used (i.e., “agree,” “OK”; Tausczik & Pennebaker, Reference Tausczik and Pennebaker2010).
Intervention evaluation
Evaluations of each intervention were assessed at post-test, with five questions related to the intervention to which participants had been assigned. Participants responded on a 5-point scale ranging from 1 (totally disagree) to 5 (totally agree) to the following questions: (a) “I liked to read/play the brochure/game,” (b) “I think that the brochure/game is attractive to others,” (c) “What I learn in the brochure/game I can use in my daily life,” (d) “While I studied/played the brochure/game, I forgot everything around me,” and (e) “I like the fact that the brochure/game is a brochure/game.” Sum scores were calculated for the participants’ evaluations of the intervention to which they had been assigned; the minimum score that participants could obtain was 5 and the maximum score 25.
In addition, the intrinsic motivation inventory (IMI; McAuley, Duncan, & Tammen, Reference McAuley, Duncan and Tammen1987; Ryan, Reference Ryan1982) was used to assess participants’ subjective experience related to HitnRun gameplay at post-test. We included the subscales interest/enjoyment (n = 71; α = .90); perceived competence (n = 71; α = .86); effort (n = 71; α = .79); value/usefulness (n = 71; α = .95); and perceived choice while performing a given activity (n = 71; α = .86), yielding five subscale scores with excellent reliability. Example items for the subscales are, respectively, “I enjoyed doing this activity very much,” “I think I am pretty good at this activity,” “I tried very hard on this activity,” “I believe doing this activity could be beneficial to me,” and “I believe I had some choice about doing this activity.” Participants answered these items on a 7-point scale ranging from “1 = not at all true” to “7 = completely true.” We performed additional intervention evaluation analyses and report on them in the supplementary materials.
Strategy of Analysis
Prior to running the analyses, we checked for outliers in our data (±3 interquartile range; Walfish, Reference Walfish2006). In accordance with the intention-to-treat principle, all of the participants who had been randomized to a group were included in the weekly smoking and abstinence analyses. Thus, participants who did not show up for the post-test lab session or did not fill out the three-month follow-up questionnaire were included as nonabstinent, using the same values as at pretest. Therefore, only one participant was excluded from the analyses regarding weekly smoking behavior (outlier), and no participants were excluded from abstinence analyses. One participant was excluded (outlier) from the analyses regarding game dose–response effects; eleven participants were excluded (two due to outliers; nine due to missing data) from analyses regarding brochure dose–response effects.
We performed chi-square tests and independent sample t tests to examine whether randomization resulted in an equal baseline distribution of relevant participant characteristics across the two intervention groups (see Table 1). Significant differences at baseline were controlled for in our subsequent analyses. In addition, we performed correlations for the difference scores of weekly smoking behavior from pretest to post-test and from pretest to follow-up and a variety of measures (i.e., age, education level, prior gaming experience, nicotine dependence, craving levels, motivation to quit, expectations, number of smoking friends, and peer environmental smoking) for the whole sample. Full explanations of how these participant characteristics were measured can be found in the supplementary materials. Furthermore, we performed independent sample t tests for sex and difference scores of weekly smoking behavior from pretest to post-test and from pretest to follow-up for the whole sample.
Confirmatory analyses
Weekly smoking behavior was analyzed with a Group (brochure vs. game) × Time (pretest vs. post-test vs. three-month follow-up) repeated measures ANOVA, comparing group differences for smoking quantity per week. In addition, we performed chi-square tests to examine whether abstinence rates differed between groups (brochure vs. game) at post-test and at three-month follow-up. Furthermore, we performed analyses for both intervention groups separately to check for dose–response effects on weekly smoking behavior using two Dose (low vs. vs. high dose of reading the brochure/number of game play sessions) × Time (pretest vs. post-test vs. follow-up) repeated measures ANOVAs of weekly smoking behavior. Greenhouse-Geisser corrections were used when the assumption of sphericity was violated. Follow-up t tests with a Bonferroni correction for multiple comparisons were employed when the interaction effects were significant. In the supplementary materials, we report on additional Bayesian repeated measures ANOVAs and chi-square tests for all of our confirmatory analyses to inform the interpretation of null findings.
Exploratory analyses
Based on our confirmatory analyses, we found out that the majority of change in weekly smoking rates took place between pretest and post-test (overall decrease of 62% in weekly smoking rates from pretest to post-test; a small overall increase of 9% in weekly smoking rates was observed from post-test to follow-up). Because our exploratory analyses are meant to understand the types of peer processes and engagement processes that might be beneficial to successful smoking cessation among young people, we chose to focus the exploratory analyses on the time window between pretest and post-test where the most change took place.
Text-based analyses—game group only
We exported the textual Hangouts data to SPSS to perform Pearson correlations between a difference score of weekly smoking behavior from pretest to post-test and a continuous measure of game play dose and all LIWC variables except word count and emotional tone. Word count was not normally distributed, so it was transformed into a dichotomous variable based on a median split (median split = 65; n low = 36, and n high = 36; Iacobucci, Posavac, Kardes, Schneider, & Popovich, Reference Iacobucci, Posavac, Kardes, Schneider and Popovich2015). Emotional tone is a summary variable that includes both positive and negative emotional dimensions. Numbers below 50 reflect a more negative tone, and numbers above 50 reflect a more positive tone. Therefore, emotional tone was transformed into a dichotomous variable excluding missing cases, based on a cut-off score of 50 (n negative = 32, and n positive = 24). The sample sizes differ because not all of the participants expressed themselves in the Hangouts conversations, which yielded less data to analyze. Repeated measures ANOVAs were used to examine the relation between weekly smoking from pretest to post-test and word count and emotional tone. Again, Greenhouse-Geisser corrections were used when the assumption of sphericity was violated. Follow-up t tests with a Bonferroni correction for multiple comparisons were employed when interaction effects were significant. Independent sample t tests were used to examine the relation between game dose, and word count and emotional tone.
Intervention evaluation
An independent samples t test was performed to test for differences between groups on intervention evaluation. In addition, we performed correlational analyses, separately for each intervention group, for intervention evaluation measures and a difference score of weekly smoking measures from pretest to post-test and continuous intervention dose measures. Finally, we performed correlational analyses for participants’ subjective experience related to HitnRun gameplay and a difference score of weekly smoking levels from pretest to post-test and game dose.
Results
Table 1 presents the descriptive statistics for the participant characteristics and outcome variables per group at the pretest. No group differences were observed at the pretest point, indicating that the random assignment was successful. In Table 2, we present the correlations between a range of different participant characteristics and smoking behavior from pretest to post-test and from pretest to follow-up for the whole sample. The correlational analyses showed that larger decreases in weekly smoking behavior from pretest to post-test and from pretest to follow-up were associated with lower education level, higher prior gaming experience, higher baseline nicotine dependence levels, higher motivation to quit at baseline, and higher exposure to peer smoking. Additionally, greater decreases in weekly smoking behavior from pretest to post-test were also associated with higher baseline expectations. An independent samples t test for sex and smoking outcomes showed that males showed larger decreases in smoking behavior from pretest to post-test, t (142) = −2.76; p = .007, and the same trend was observed for decreases in smoking behavior from pretest to follow-up, t (141) = −1.96; p = .052. Notably, even given the large age range, there were no significant correlations between age and other variables, including smoking behavior.
Table 2. Correlations between intervention evaluation variables and smoking outcome variables

Note: We performed bivariate Pearson correlations for continuous variables; Kendal's tau correlations were applied for ordinal variables.
p-values are represented between parentheses for each correlation. Significant correlations are bolded.
Confirmatory Analyses
Weekly smoking behavior
A Group × Time repeated measures ANOVA on number of cigarettes smoked per week revealed a main effect for Time, F (1.81, 254.95) = 120.43, p < .001, ηp2 = .46, indicating a general decrease in cigarettes per week from pretest to follow-up (see Figure 3). There was no main effect for Group, F (1, 142) = .00, p = .979, ηp2 < .01, nor was there an interaction effect for Group × Time, F (1.81, 254.95) = .87, p = .412, ηp2 = .01. Thus, contrary to our hypotheses, both intervention groups showed a steep decrease in the number of cigarettes that they smoked from pretest to post-test (p < .001) and a small increase in number of cigarettes from post-test to follow-up (p < .001), but there were no differences between the groups.

Figure 3. Cigarettes per week for game group and brochure group.
Abstinence
A chi-square test revealed no significant effect for group on abstinence levels at post-test, χ2 (1, n = 144) = .00, p = 1.000, and follow-up, χ2 (1, n = 144) = .03, p = .856. This indicates, contrary to our hypotheses, that there were as many participants in the brochure group as in the game group that were abstinent at post-test and follow-up (see Table 3).
Table 3. Abstinence rates at post-test and follow-up

Dose-response effects
Brochure
A Dose × Time repeated measures ANOVA revealed a main effect for Time, F (1.50, 88.41) = 63.13, p < .001, ηp2 = .52, indicating a general decrease in cigarettes per week from pretest to follow-up. Furthermore, a significant effect for Dose was found F (1, 59) = 20.73, p < .001, ηp2 = .26, indicating higher weekly smoking rates for participants reporting to have invested more time in reading the brochure than participants that invested less time in reading the brochure (see Figure 4). There was no significant interaction effect for Dose × Time, F (1.50, 88.41) = 2.52, p = .101, η p2 = .04.

Figure 4. Cigarettes per week for brochure group with brochure dose as moderator.
Game
A Dose × Time repeated measures ANOVA revealed a main effect for Time, F (2, 138) = 79.50, p < .001, ηp2 = .54, indicating a general decrease in cigarettes per week from pretest to follow-up. No significant effect was found for Dose F (1, 69) = 1.47, p = .230, ηp2 = .02. As expected, a significant Dose × Time interaction effect was found, F (2, 138) = 3.23, p = .043, ηp2 = .05. Follow-up tests indicated that only at post-test (not at pretest or follow-up) there was a significant difference (p = .027) between low and high dose of gaming sessions, with lower weekly smoking levels for participants that reported a higher dose of gaming sessions than those with a lower reported dose of gaming sessions (see Figure 5). Additional follow-up tests showed that there were significant differences between all measurement moments for the low and high dose group. All follow-up tests are reported in the supplementary materials (see Table S.2).

Figure 5. Cigarettes per week for game group with game dose as moderator.
Exploratory Analyses
Text-based analyses—game group only
All of the correlations between the decrease in weekly smoking behavior, intervention dose, and LIWC categories are displayed in Table 4. These correlations show that more use of first person singular pronouns was associated with larger decreases in weekly smoking rates from pretest to post-test and higher dose of gameplay. More use of second person pronouns was associated with larger decreases in weekly smoking from pretest to post-test and with a higher dose of gameplay. Finally, high usage of assent words was related to larger decreases in weekly smoking rates from pretest to post-test. Interestingly, high use of first person singular pronouns and second person pronouns and assent words seemed to co-occur, and all three were related to better outcomes. Thus, more frequent use of first person singular, second person pronouns, and assent words was related to larger decreases in weekly smoking rates from pretest to post-test. No significant correlations were found for first person plural, impersonal pronouns, past focus, present focus, social and affiliation categories and our outcomes.
Table 4. Correlations between LIWC categories, weekly smoking levels, and game dose

Note: p-values are represented between parentheses for each correlation. Significant correlations are bolded.
A Word Count × Time repeated measures ANOVA revealed a main effect for Time, F (1, 70) = 131.50, p < .001, ηp2 = .65, indicating a general decrease in cigarettes per week from pretest to post-test. No significant effect was found for Word Count F (1, 70) = .05, p = .833, ηp2 < .01. Finally, a Word Count × Time trend emerged, F (1, 70) = 3.19, p = .078, ηp2 = .04. Follow-up tests indicated that the decrease in weekly smoking from pretest to post-test was significant for participants with both a low and a high word count. No significant differences were found between participants with low and high word count on either the pretest or post-test.
An Emotional Tone × Time repeated measures ANOVA revealed a main effect for Time, F (1, 54) = 111.96, p < .001, ηp2 = .68, indicating a general decrease in cigarettes per week from pretest to post-test. No significant effect was found for Emotional Tone, F (1, 54) = .16, p = .696, ηp2 < .01. Finally, there was no significant Emotional Tone × Time interaction effect, F (1, 54) = 2.19, p = .145, ηp2 = .04. All follow-up tests are reported in the supplementary materials (see Table S.2).
An independent samples t test showed a trend between low and high word count and game dose, t (59.14) = −1.79; p = .079, such that participants who used greater numbers of words in the Hangouts conversations also played HitnRun for longer durations (M = 136.60, SD = 124.50) than the participants who used fewer words did (M = 92.75, SD = 78.74). An independent samples t test showed a significant difference between negative and positive emotional tone based on game dose, t (31.42) = −2.36; p = .024. This indicates that participants who expressed themselves in the Hangouts conversation more positively also played HitnRun for longer durations (M = 83.98, SD = 70.15) than the participants who expressed themselves more negatively did (M = 158.46, SD = 141.93).
Intervention evaluation
An independent samples t test showed a significant difference between the game group and the brochure group on intervention evaluation, t (124) = −2.50; p = .014. This indicates that participants in the game group rated the game intervention more favorably (M = 15.21, SD = 4.10) than the participants in the brochure group rated the brochure intervention (M = 13.49, SD = 3.53). Separate correlational analyses were performed for each intervention group for intervention evaluation, and the difference score of weekly smoking behavior from pretest to post-test and a continuous measure of intervention dose (see Table 5). In line with our previous ANOVA findings, we found that a higher dose of gameplay was associated with larger decreases in the number of weekly cigarettes from pretest to post-test. No significant correlations were found between decreases in weekly smoking from pretest to post-test and the dose of reading the brochure.
Table 5. Correlations between intervention evaluation, weekly smoking levels, and intervention dose

Note: Numbers above the diagonal represent correlations for the game group only, whereas numbers below the diagonal represent correlations for the brochure group only. IMI = Intrinsic Motivation Inventory; IMI scores were not obtained for the brochure group. p-values are represented between parentheses for each correlation. Significant correlations are bolded.
Significant correlations are bolded.
In addition, a higher intervention evaluation within the game group was associated with a higher dose of HitnRun gameplay. In contrast, the correlations within the brochure group showed no relation between the dose of reading the brochure and intervention evaluation. No direct correlations were found between decreases in weekly smoking from pretest to post-test and intervention evaluation in either group. Finally, the intrinsic motivation inventory variables did not correlate with weekly smoking measures but with dose of gameplay. Specifically, higher dose of gameplay was associated with higher perceived competence, effort, perceived choice, and value (see Table 5). In addition, higher intervention evaluation was related to higher levels of interest, perceived competence, effort, perceived control, and value.
Discussion
The current two-armed RCT tested the effectiveness of the social mobile game intervention HitnRun among young smokers who were motivated to quit smoking. The game intervention was compared with an active brochure intervention to test its effects on weekly smoking and abstinence rates as well as dose–response effects. Contrary to our expectations, no differences were found between participants in the game and brochure intervention on weekly smoking behavior and abstinence rates. Yet, we did find a dose–response effect for the game group only: participants that played HitnRun for a longer period of time over all gaming sessions also showed lower weekly smoking levels than participants that played HitnRun for a shorter period of time at post-test. This effect faded away, however, at the three-month follow-up. In the brochure group, we only found that participants that read the brochure for longer periods of time, also reported higher levels of weekly smoking behavior at all measurement moments.
Although we hoped to find stronger beneficial effects of HitnRun on weekly smoking levels and abstinence levels over time, we know that smoking cessation in this group of young smokers is very hard to reach, especially since the majority of this group had a lower education level (Hill et al., Reference Hill, Amos, Clifford and Platt2014; Springvloet et al., Reference Springvloet, Kuipers and Van Laar2017). Nevertheless, we were able to help 35% (post-test) and 30% (three-month follow-up) of all participants quit smoking in this study, which is high compared with other studies that estimate 9% abstinence rates following interventions (Fanshawe et al., Reference Fanshawe, Halliwell, Lindson, Aveyard, Livingstone-Banks and Hartmann-Boyce2017; Nationaal Expertisecentrum Tabaksontmoediging, 2013; Sussman, Sun, & Dent, Reference Sussman, Sun and Dent2006). Also, we were able to reach youth that are difficult to recruit and retain in smoking cessation trials: largest effects on smoking behavior were established within a group of participants that had a lower education level, were more severely addicted, and were more exposed to peer smoking (these effects are mostly driven by the game group; see Table S.1 in the supplementary materials). Altogether, it seems that we have been quite successful in both intervention groups to help youth quit smoking.
The equal improvements in weekly smoking behavior and abstinence rates in both groups can be understood in two ways. First, as parts of this study took place in a controlled research environment with multiple “live” contact moments between participants and researchers, nonspecific factors, such as motivation to quit smoking, expectations, therapeutic alliance, and mindset, may have played a large role in boosting smoking cessation in both intervention groups (Boot et al., Reference Boot, Simons, Stothart and Stutts2013; Crum, Leibowitz, & Verghese, Reference Crum, Leibowitz and Verghese2017; Crum & Phillips, Reference Crum, Phillips, Scott, Kosslyn and Pinkerton2015; Dweck, Reference Dweck2006; McCuller, Sussman, Wapner, Dent, & Weiss, Reference McCuller, Sussman, Wapner, Dent and Weiss2006; Newman, Szkodny, Llera, & Przeworski, Reference Newman, Szkodny, Llera and Przeworski2011). For example, it may be that our casual talks with participants during pretest and post-test measurements, whereby we tried to be independent and nonjudgmental listeners to their stories and to understand their personal reasons and needs to quit smoking, might have been effective by actively supporting this highly motivated group of participants to help them quit smoking (Lenkens et al., Reference Lenkens, Rodenburg, Schenk, Nagelhout, Van Lenthe, Engbersen and Van De Mheen2019; Schenk et al., Reference Schenk, Sentse, Lenkens, Engbersen, van de Mheen, Nagelhout and Severiens2018). These nonspecific effects can be very valuable (Crum et al., Reference Crum, Phillips, Scott, Kosslyn and Pinkerton2015; Reference Crum, Leibowitz and Verghese2017), but they may have limited the effect of the game mechanics specifically, which may have been found with an otherwise wait-list control. Future studies will benefit from measuring these nonspecific factors to disentangle such alternative explanations.
The second explanation for equal improvements in both groups is related to the design of our study: in RCT's, participants are randomized to different treatment groups to ensure that they do not differ in any systematic way (Suresh, Reference Suresh2011). Although there are multiple very good reasons to use RCT designs, this design also contradicts the design-thinking principles that likewise guide our work. In an RCT, participants are randomized to take part in one of two interventions with which they do not necessarily connect. In contrast, according to participatory-driven design principles, participants should be matched to interventions that best fit their preferences, demographics, personalities, and needs (Scholten & Granic, Reference Scholten and Granic2019). In our study, participants that liked playing games benefitted most from this game intervention, as substantiated by the positive association between prior game experience and decreases in weekly smoking over time (see Table S.1 in the supplementary materials). Based on this reasoning, we planned the dose–response analyses because they gave us more insight into the potential connection that participants had with the intervention.
As expected, higher game play dose was related to larger decreases in weekly smoking levels from pretest to post-test, but this effect faded over the three-month follow-up. It is promising that we were able to motivate a hard-to-reach group of young smokers to be involved in the game intervention, thereby helping this subgroup to reduce smoking, especially since there are almost no evidence-based interventions that are currently available (Fanshawe et al., Reference Fanshawe, Halliwell, Lindson, Aveyard, Livingstone-Banks and Hartmann-Boyce2017; Nationaal Expertisecentrum Tabaksontmoediging, 2013). Although promising, we were not able to maintain this positive effect on smoking behavior over the three-month follow-up period. Therefore, we need to strengthen the intervention itself and additionally maybe add booster sessions over longer follow-up periods in order to show long-term intervention effectiveness (Hale, Fitzgerald-Yau, & Viner, Reference Hale, Fitzgerald-Yau and Viner2014).
While we did not have strong expectations regarding a dose–response effect for the brochure group, we found that participants who read the brochure for longer periods of time surprisingly reported higher levels of weekly smoking behavior at all measurement moments. It might be that highly motivated participants in the brochure group, who were also suffering from high craving, high nicotine dependence levels, and multiple friends smoking in their environment etc., tried to cope with those feeling by reading the brochure very often, but the brochure was not a strong enough intervention to help them. This explanation is supported in that of the thirteen participants who dropped out at post-test, eleven had been randomized to the brochure group and only two to the game group. To further investigate the types of peer processes and communication that might be underlying the beneficial effects of playing HitnRun, we explored potential peer-based game factors that could have affected smoking outcomes.
Peer Processes
HitnRun was designed to bring together like-minded youth who wanted to quit smoking to instantiate a supportive peer context that could trigger long-lasting smoking cessation. Our text-based exploratory analyses of communication between teams were used to investigate the affordances of these peer-influence based game factors on smoking behavior and game dose. We found that participants who used more first person singular pronouns and second person pronouns also played HitnRun more often and showed larger decreases in weekly smoking rates from pretest to post-test. These results might reflect participants’ increased levels of self-disclosure, which in turn promoted closeness to others (Laurenceau, Barrett, & Pietromonaco, Reference Laurenceau, Barrett and Pietromonaco1998; Rankin-Esquer, Burnett, Baucom, & Epstein, Reference Rankin-Esquer, Burnett, Baucom and Epstein1997).
Empirical studies show that the use of first person singular pronouns is related to conversational engagement, informal and socially oriented communication, emotional disclosure, and psychological closeness (Pennebaker & King, Reference Pennebaker and King1999; Pennebaker, Mehl, & Niederhoffer, Reference Pennebaker, Mehl and Niederhoffer2003; Seih, Lin, Huang, Peng, & Huang, Reference Seih, Lin, Huang, Peng and Huang2008). Second person pronouns are found to stimulate the dialogue one can have with oneself in the form of self-support (Seih et al., Reference Seih, Lin, Huang, Peng and Huang2008). This social cohesion and support hypothesis is also corroborated by our findings that the use of more positive and more assent words is related to higher doses of HitnRun gameplay and better smoking outcomes respectively. Previous literature has shown that more positive and endorsing language towards each other is related to higher levels of agreement, responsiveness, and cohesion (Tausczik & Pennebaker, Reference Tausczik and Pennebaker2010) and that, in turn, group cohesion is related to better outcomes (Tamersoy et al., Reference Tamersoy, Chau and De Choudhury2017; Tausczik & Pennebaker, Reference Tausczik and Pennebaker2010). In sum, these exploratory analyses suggest that creating a cohesive, supportive, and positive peer context can indeed help youth successfully quit smoking.
Engagement Processes
Through the design of HitnRun we attempted to address the mismatch between current intervention programs and the needs of young people. Overall, HitnRun was evaluated more positively than the brochure. It is very important that we found that HitnRun was able to engage youth; otherwise, our rationale for using design thinking and participatory design principles would have been lost. Within the brochure group, no relations were found between intervention evaluations and dose and weekly smoking levels. Within the game group, intervention evaluation measures were not consistently and convincingly related to decreases in weekly smoking levels from pretest to post-test, yet higher doses of HitnRun (i.e., more time playing the game) gameplay were associated with higher intervention evaluations and higher perceived competence, effort, perceived choice, and value. Probably, the more that the participants connected with HitnRun, as indicated by higher intervention evaluations, the more time they invested in playing it, which in turn could have led to better smoking outcomes. In sum, HitnRun seems to have provoked feelings of autonomy, competence, and relatedness, thereby not only motivating individuals to play more (i.e., dose) but also enhancing psychological wellbeing or changing behavior (Baranowski, Baranowski, Thompson, & Buday, Reference Baranowski, Baranowski, Thompson and Buday2011; Orji, Mandryk, & Vassileva, Reference Orji, Mandryk and Vassileva2017; Przybylski, Rigby, & Ryan, Reference Przybylski, Rigby and Ryan2010; Ryan, Rigby, & Przybylski, Reference Ryan, Rigby and Przybylski2006).
Although promising, these results only inform us about engagement of participants in the game group compared with those in the control group, but that does not directly translate into engagement success or retention of engagement over time. Based on qualitative interviews with participants at the post-test, we learned that participants got annoyed by technical difficulties that sometimes came up during HitnRun gameplay. Furthermore, participants reported that four weeks of HitnRun gameplay was a bit long, which was also substantiated by a decrease in number of game play sessions over time, as was demonstrated by our back-end data analyses. This was probably due to the repetitiveness of the elements of the game, as we did not add new content to HitnRun over the intervention weeks. Thus, to retain engagement of participants over time, the next iteration of HitnRun should deal with the technical issues that were reported by the participants and new content should be added to improve the replay ability of HitnRun. All of these peer-process and engagement-process findings encourage us to explore further participant and intervention characteristics that lead to beneficial effects for specific subgroups of young people.
Limitations
A primary limitation of the current study is the length of follow-up measurements. While setting up this study, a lot more time and resources than were expected went into the actual game design, which required a great deal of multidisciplinary collaboration and application of (new-to-us) design thinking principles to maximize youth engagement. Thus, due to unexpected time constraints, we were only able to include a three-month follow-up for this trial. Preferably, we would have included a six-month and even a one-year follow-up to find out whether the effects lasted over longer periods of time, and we strongly suggest that future studies include longer follow-up periods (as also recommended by Fanshawe et al., Reference Fanshawe, Halliwell, Lindson, Aveyard, Livingstone-Banks and Hartmann-Boyce2017; Garrison, Christakis, Ebel, Wiehe, & Rivara, Reference Garrison, Christakis, Ebel, Wiehe and Rivara2003; Simon, Kong, Cavallo, & Krishnan-Sarin, Reference Simon, Kong, Cavallo and Krishnan-Sarin2015; Stockings et al., Reference Stockings, Hall, Lynskey, Morley, Reavley, Strang and Degenhardt2016; Villanti et al., Reference Villanti, McKay, Abrams, Holtgrave and Bowie2010).
Another limitation is the strong reliance on self-report data, which may have led to an overestimation of our results because of shared method variance (Kim & Cicchetti, Reference Kim and Cicchetti2010). In the current study it was difficult to include other informants (De Los Reyes, Reference De Los Reyes2011; Hunsley & Mash, Reference Hunsley and Mash2007; Mash & Hunsley, Reference Mash and Hunsley2005), such as parents, because many parents were not aware of the smoking status of their child. Including parental ratings would have excluded a large group of youth from our trial because they would not have participated if parental contact was mandatory. However, we strongly endorse the use of additional informants in future studies (Cicchetti, Ackerman, & Izard, Reference Cicchetti, Ackerman and Izard1995; Kobus, Reference Kobus2003; Zeman, Klimes-Dougan, Cassano, & Adrian, Reference Zeman, Klimes-Dougan, Cassano and Adrian2007), especially if future studies include existing peer groups as part of the intervention (Foster, Linehan, Kirman, Lawson, & James, Reference Foster, Linehan, Kirman, Lawson and James2010; Maher et al., Reference Maher, Lewis, Ferrar, Marshall, De Bourdeaudhuij and Vandelanotte2014). If youth who already know each other within established peer groups could be recruited to participate, we could mimic conditions similar to young people's real-world digital social experiences, allowing for the potential of almost limitless peer-to-peer social support as well as the potential to incorporate assessments from multiple informants (Vandelanotte & Maher, Reference Vandelanotte and Maher2015).
Furthermore, if possible we recommend biochemical verification of smoking behavior, such carbon-monoxide (CO) levels in breath or cotinine levels in saliva, blood, urine, or hair (Deveci, Deveci, Açik, & Ozan, Reference Deveci, Deveci, Açik and Ozan2004; Florescu et al., Reference Florescu, Ferrence, Einarson, Selby, Soldin and Koren2009). However, biochemical verification often contrasts with other intervention objectives we have, such as anonymity and accessibility, especially in future studies testing the effects of HitnRun “in the wild.” Therefore, we also suggest efforts to work towards the use of ecological momentary assessment (Shiffman, Reference Shiffman2009) and, in the near future, passive assessment of smoking behavior through mobile phones (Lind, Byrne, Wicks, Smidt, & Allen, Reference Lind, Byrne, Wicks, Smidt and Allen2018).
Finally, although we did not find any significant associations between our smoking outcome measures and age, we did include a broad range of ages in our sample. A more narrow age range would not only make more sense developmentally but also might have implications for the intervention game design. In the design process of the current version of HitnRun, we could work around the broad age range by inviting youth of different ages to our focus groups and iterative testing sessions and by choosing the casual runner genre as the basis for HitnRun because we know this game genre is age-independent and runner games are played equally by children, adolescents, and adults (Parkin, Reference Parkin2013). Yet beyond these efforts, the needs, motivations, and preferences of a 16-year-old adolescent to smoke or quit smoking probably differ from those of a 25-year-old young adult, and these needs, motivations, and preferences were the basis of the design of HitnRun as well (Scholten & Granic, Reference Scholten and Granic2019). By narrowing down the age range, we may be able to address more specifically the needs, motivations, and preferences of youth, thereby trying to understand peer and engagement processes even better for this specific subgroup to hopefully increase our chance for successful smoking cessation.
Future Intervention and Game Design Implications
We found evidence for a dose–response effect and our exploratory analyses have given us an important perspective on who benefited most from HitnRun. We are encouraged by these results because they provide concrete directions to further iterate on the game. One of the most difficult assignments is to effectively provide opportunities for social connection in the context of young adult smoking cessation (Struik et al., Reference Struik, Bottorff, Baskerville and Oliffe2018), and we succeeded in part. We showed that for those who connected with and were engaged by the intervention the effects on smoking behavior were the largest. However, this also means that there was a group of young people who we did not reach and who did not connect with our intervention. Some participants did not use the peer support opportunities of HitnRun, did not like playing games, or specifically disliked our game.
Our next challenge is to find out how we can further promote players’ connections to and engagement with the intervention. For example, we could encourage conversations with other team members by designing in-game incentives or by priming players to think about their future selves more concretely through playful photo-sharing mechanics that help them visualize themselves as older. Yet, there is also a group of youth that will probably never connect with HitnRun, and for these youth there should be other intervention possibilities available to help them quit smoking. We will need a set of experimental studies to find out for whom HitnRun is a suitable intervention option. Screening tools can then be deployed to target at-risk individuals with recommendation algorithms that can offer HitnRun as their best option for successful quitting. For those with different screening characteristics, different resources including face-to-face coaching or other options could be offered. Furthermore, we need to find out which factors amplify connection to and engagement with HitnRun and whether youth would pick up HitnRun themselves before we move on to an ultimate implementation trial. Within these experimental studies, we need to move beyond RCTs towards more creative or appropriate designs, such as machine learning approaches that can be used to develop just-in-time adaptive interventions (Fisher & Soyster, Reference Fisher and Soyster2019) or single-case experimental designs (Wolery, Dunlap, & Ledford, Reference Wolery, Dunlap and Ledford2011) that evaluate the effectiveness of different versions of interventions on participants and make decisions about which of those versions is most effective. Our ultimate goal is to develop a suite of interventions from which youth have the opportunity to choose the product, digital or otherwise, that best fits their needs and can empower them to change their behavior.
The next iteration of HitnRun should incorporate ecological momentary assessments, instead of the retrospective reporting that was used in the current study, to track mood, smoking moments, and craving over time in the month before the quit date (Fisher & Soyster, Reference Fisher and Soyster2019; Lind et al., Reference Lind, Byrne, Wicks, Smidt and Allen2018). This information can be fed back into the game system, which then automatically prepares the personalized triggers that will be sent to the participants during the intervention period (Fisher & Soyster, Reference Fisher and Soyster2019). Furthermore, the game system itself will incorporate a messaging system that allows participants to communicate with their team members, and this messaging system will also deliver feedback to the teams about their and other teams’ performance.
The basis of the current study was inspired by Tom Dishion's seminal work on peer influence processes. The next step would be to use more sequential, time-series types of data that are collected within the game system for HitnRun to identify the same types of social learning mechanisms that predicted peer support which, in turn, predicted outcomes like substance use many years later (Dishion, Capaldi, Spracklen, & Li, Reference Dishion, Capaldi, Spracklen and Li1995; Dishion & Tipsord, Reference Dishion and Tipsord2011). This more fine-grained analysis can give us specific suggestions about how to iterate on the peer chat function in the game, providing youth with more opportunities to seamlessly support and socially reinforce positive behavioral change and, conversely, minimize reinforcement of antisocial talk (e.g., about smoking potential or cravings).
Another important and related design iteration is the upgrade in personalization of HitnRun. Personalization is consistently mentioned as one of the biggest advantages of digital solutions, but it has not been realized in many game-based interventions (Orji et al., Reference Orji, Mandryk and Vassileva2017; Scholten & Granic, Reference Scholten and Granic2019). Also within the current version of HitnRun, only the tailored messages were personalized, and we believe that we need to optimize this to reach more young people and strengthen the potential of HitnRun. The next version of HitnRun could start with an empty picture library: during the month before the start of the intervention participants will be prompted by the game system to take selfies of themselves smoking, these selfies will be included in the picture library as “no-go” pictures. Then, when the intervention period starts, they will be prompted to take selfies of themselves not smoking, these pictures will be included as “go” pictures. When playing this new version HitnRun, participants will repeatedly respond to their own personal pictures, which will be updated over the intervention period, whereas they will not respond to “their previous self” over and over again.
Conclusion
In conclusion, the current study revealed equal improvements in weekly smoking behavior and abstinence rates for the game and brochure group. Yet, the game group showed a dose–response effect directly after the intervention, which faded over the three-month follow-up. Thus, when participants connected with the game intervention and played it for longer periods of time, they also reported lower smoking levels. Exploratory analyses showed that the most powerful effects for HitnRun on weekly smoking levels over time were found for those who connected with and were engaged by the intervention.
It is promising that we were able to help a subgroup of hard-to-reach young people quit smoking, especially since HitnRun was most successful in a group of participants who had lower education levels, were more severely addicted, and were more severely exposed to peer smoking, yet also had a higher motivation to change. Future work should build on the potential of HitnRun by increasing personalization efforts and strengthening peer influence components, advancing the goal of developing a multicomponent intervention that is dynamically adjustable to individual needs to reach as many young people as possible.
Supplementary Material
The supplementary material for this article can be found at https://doi.org/10.1017/S0954579419001378
Acknowledgments
We gratefully acknowledge the contributions of Ken Koontz, James Comstock, and Mathieu Allaert who codeveloped HitnRun. We also want to thank Rozemarijn Erdbrink, Anna Boormans, Rutger van Mierlo, Eva Tuijtelaars, Iris Verdeuzeldonk, and Amber Reuser for their help with data collection. This work was financially supported by ‘t Trekpaert. They had no role in the design of the study, the collection, analysis, and interpretation of data, in writing the manuscript, or in the decision to submit the article for publication.












