Mindfulness is defined as the ability to maintain nonjudgmental, present-centered awareness (Kabat-Zinn & Kabat-Zinn, Reference Kabat-Zinn and Kabat-Zinn1997) and can be understood as both an intrapersonal and interpersonal process, affecting not only an individual’s physical and psychological wellbeing, but also their ability to communicate effectively with others and navigate conflict and disagreement (Davis & Hayes, Reference Davis and Hayes2011). The past two decades have seen growing empirical support for the use of mindfulness-based interventions to address a range of clinical problems, and increasing evidence suggests interventions delivered during pregnancy may reduce adverse mental health outcomes (Dhillon et al., Reference Dhillon, Sparkes and Duarte2017; Taylor et al., Reference Taylor, Cavanagh and Strauss2016). Similarly, research suggests that incorporating mindfulness into parenting interventions enhances the quality of parent–child relationships, reduces child psychopathology, and promotes optimal child socioemotional functioning (McKee et al., Reference McKee, Parent, Zachary and Forehand2018; Meppelink et al., Reference Meppelink, de Bruin, Wanders-Mulder, Vennik and Bögels2016; Sawyer Cohen & Semple, Reference Sawyer Cohen and Semple2010; van den Heuvel et al., Reference van den Heuvel, Johannes, Henrichs and Van den Bergh2015). Despite findings demonstrating the importance of parental present-centered awareness, the factors undermining mindfulness during parenting have received less attention. The goals of the present study were (1) to investigate both parental trauma-related distress and general negative affectivity during pregnancy as simultaneous predictors of diminished parental emotional self-awareness and heightened reactivity when parenting toddlers and (2) to examine impaired parent–infant bonding as a mechanism explaining this link.
Antecedents and consequences of mindful parenting
Cultivating present-centered awareness improves attention (Bögels et al., Reference Bögels, Lehtonen and Restifo2010), which plays an important role in regulating parenting behaviors (Crandall et al., Reference Crandall, Deater-Deckard and Riley2015; Deater-Deckard et al., Reference Deater-Deckard, Wang, Chen and Bell2012). Such findings have helped stimulate an increase in efforts to understand the core components of mindful parenting and the role of mindful parenting in child development. In their seminal work, Kabat-Zinn and Kabat-Zinn (Reference Kabat-Zinn and Kabat-Zinn1997) described mindful parenting as a continual process through which parents become more aware of their children’s feelings through learning to observe and accept their own feelings. Further, Duncan and colleagues (Reference Duncan, Coatsworth and Greenberg2009) have since proposed several dimensions of mindful parenting: listening with full attention, nonjudgmental acceptance of self and child, emotional awareness of self and child, self-regulation in the parenting relationship, and compassion for self and child. Within this framework, mindful parenting involves not only being tolerant of and sensitive to children’s emotions, but also acknowledging one’s own reactions during parenting interactions and not acting upon negative emotions in maladaptive ways (Duncan et al., Reference Duncan, Coatsworth and Greenberg2009). Mindful parenting is of particular importance during toddlerhood, a period during which children’s emerging developmental needs (e.g., conflicting needs for autonomy and support) and limited ability to communicate and regulate their own emotions may exacerbate parenting stress (Potharst et al., Reference Potharst, Zeegers and Bögels2018).
A strong body of research indicates that parental mindfulness promotes early child socioemotional functioning (e.g., van den Heuvel et al., Reference van den Heuvel, Johannes, Henrichs and Van den Bergh2015). Parental sensitivity and acceptance, key facets of mindful parenting, contribute to the development of self-regulation among children (Bernier et al., Reference Bernier, Carlson and Whipple2010; Kochanska et al., Reference Kochanska, Murray and Harlan2000). Drawing on such findings, interventions aimed at increasing mindful parenting have been shown to reduce both parent and child internalizing and externalizing behaviors (Behbahani et al., Reference Behbahani, Zargar, Assarian and Akbari2018; Bögels et al., Reference Bögels, Hellemans, van Deursen, Römer and van der Meulen2014; Coatsworth et al., Reference Coatsworth, Duncan, Greenberg and Nix2010), as well as aggression and noncompliance among children with developmental disabilities or autism (Singh et al., Reference Singh, Lancioni, Winton, Singh, Curtis, Wahler and McAleavey2007).
Although the advantages of mindful parenting are well-established, there remains a critical need for research identifying parental factors, present prior to the birth of the child, that ultimately undermine mindful parenting. Understanding parental risk factors during the prenatal period is essential for informing screening practices and ensuring that parents who would benefit most from mindfulness-based interventions receive appropriate and timely referrals. Further, knowledge of prenatal risk factors can also be used to tailor interventions to provide additional training and support to individuals who may experience particular difficulties in mindful parenting.
Does parental traumatic stress undermine mindful parenting?
If ongoing awareness of emotions and responding to children with nonjudgement and compassion promotes positive child outcomes, then psychopathology that interferes with these processes could undermine the benefits of mindful parenting. Although much of the research examining this question has focused on the role of depression (e.g., Bernard et al., Reference Bernard, Nissim, Vaccaro, Harris and Lindhiem2018; Connell & Goodman, Reference Connell and Goodman2002; Lovejoy et al., Reference Lovejoy, Graczyk, O’Hare and Neuman2000; Wilson & Durbin, Reference Wilson and Durbin2010), emerging findings suggest that posttraumatic stress disorder (PTSD) may also impact parenting (Creech & Misca, Reference Creech and Misca2017). In military and veteran populations, both depression and PTSD play an important role in parenting behaviors and child adjustment (Creech & Misca, Reference Creech and Misca2017). Recent studies also indicate a direct association between maternal lifetime trauma exposure and child anxiety, as well as an indirect association through parenting quality and maternal depression (Robinson et al., Reference Robinson, Hendrix, Sloan Krakovsky, Smith and Brennan2019), with increasing evidence that specific PTSD symptom clusters, such as avoidance, may exert unique effects on parenting behaviors (Brockman et al., Reference Brockman, Snyder, Gewirtz, Gird, Quattlebaum, Schmidt, Pauldine, Elish, Schrepferman, Hayes, Zettle and DeGarmo2016). More specifically, intrusion and avoidance symptoms are both associated with extreme insensitivity in observed parenting behaviors (e.g., nonresponsive to child distress, hostile or rejecting comments) during early childhood (van Ee et al., Reference van Ee, Kleber, Jongmans, Mooren and Out2016).
This body of research converges with several theoretical perspectives suggesting that depression and PTSD might interfere with mindful parenting. For instance, the action-control framework suggests that depressive symptoms impair parenting through cognitive, affective, and motivational processes that interfere with child-oriented, goal-directed action (Dix & Meunier, Reference Dix and Meunier2009). Within this framework, regulatory processes associated with depression affect the quality and nature of the parent–child relationship. Specifically, depressive symptoms may undermine parental attention to and encoding of child cues and contribute to greater negative global appraisals of children. In turn, negative appraisals are associated with more negative, coercive, and overreactive parenting, thereby undermining parents’ abilities to respond to their children with nonjudgment and compassion.
Further, the parental meta-emotion philosophy framework holds that parents’ thoughts and feelings about their own emotions impact how they respond to their children’s emotions (Gottman et al., Reference Gottman, Katz and Hooven1996). Parental meta-emotion philosophy may be particularly salient in the context of parental PTSD, as parents who avoid their own emotional experiences may have more difficulties recognizing when their emotions impact their parenting behaviors. Similarly, the perinatal interactional model posits that PTSD after childbirth contributes to suboptimal parenting behaviors through parental emotional dysregulation; further, this model highlights the possibility of preventing the intergenerational transmission of trauma by intervening during the prenatal period (Lang & Gartstein, Reference Lang and Gartstein2018).
Despite several theories pointing to the salience of PTSD as a dimension of parental psychopathology undermining parenting, the vast majority of research has focused on general depression (Lovejoy et al., Reference Lovejoy, Graczyk, O’Hare and Neuman2000; Wilson & Durbin, Reference Wilson and Durbin2010). Although PTSD is highly comorbid with depression (Flory & Yehuda, Reference Flory and Yehuda2015), the few studies examining the impact of PTSD on parenting, after accounting for depression, yield inconsistent results (Bosquet Enlow et al., Reference Bosquet Enlow, Kitts, Blood, Bizarro, Hofmeister and Wright2011; Muzik et al., Reference Muzik, Morelen, Hruschak, Rosenblum, Bocknek and Beeghly2017). One potential explanation for mixed findings is that past research has not accounted for the shared, negative affectivity that underlies both depression and PTSD. Indeed, a growing body of literature suggests that the nature of psychopathology is dimensional and hierarchical (e.g., Conway et al., Reference Conway, Forbes, Forbush, Fried, Hallquist, Kotov, Mullins-Sweatt, Shackman, Skodol, South, Sunderland, Waszczuk, Zald, Afzali, Bornovalova, Carragher, Docherty, Jonas, Krueger, Patalay, Pincus, Tackett, Reininghaus, Waldman, Wright, Zimmermann, Bach, Bagby, Chmielewski, Cicero, Clark, Dalgleish, DeYoung, Hopwood, Ivanova, Latzman, Patrick, Ruggero, Samuel, Watson and Eaton2019; Kotov et al., Reference Kotov, Waszczuk, Krueger, Forbes, Watson, Clark, Achenbach, Althoff, Ivanova, Bagby, Brown, Carpenter, Caspi, Moffitt, Eaton, Forbush, Goldberg, Hasin, Hyman, Lynam, Samuel, South, Markon, Miller, Morey, Mullins-Sweatt, Ormel, Patrick, Regier, Rescorla, Ruggero, Sellbom, Simms, Skodol, Slade, Tackett, Waldman, Widiger, Wright and Zimmerman2017). Within this framework, PTSD involves specific symptom dimensions – distinct from the general negative affectivity underlying internalizing disorders – that may also play a unique role in parenting (Gros et al., Reference Gros, Simms and Acierno2010). As such, there is a critical need for research that disentangles trauma-specific symptomatology from the more general dimension of negative affectivity common to internalizing disorders to examine the unique effects of trauma-related distress on parenting. Understanding if and how both general and specific symptoms undermine parenting is essential for informing early intervention efforts during pregnancy. Specifically, this knowledge will clarify whether there is any added benefit to screening for specific trauma-related symptoms or if efforts should be focused on more global elevations in negative affectivity. If trauma-related distress uniquely contributes to parenting difficulties, this would also suggest tailoring interventions to target persistent avoidance of distressing thoughts, memories, and external reminders of the trauma (e.g., mindfulness techniques, in vivo exposure to feared stimuli), as well as recurrent, involuntary memories of the traumatic event (e.g., imaginal exposure and/or cognitive reappraisal to change the relationship to trauma-related memories). Further, if trauma symptoms uniquely impact parenting, prevention efforts that aim to prepare women with a history of trauma for the childbirth experience may be warranted.
Methodological considerations: Longitudinal design, dimensional measurement of psychopathology, and factoring in fathers
The contributions of parental psychopathology to parenting difficulties is well-established; however, poor parent–child relationship quality also has the potential to exacerbate parental psychopathology (Paschall & Mastergeorge, Reference Paschall and Mastergeorge2016). Thus, longitudinal research designs are necessary to tease apart the temporal order of effects. Further, examining parental trauma symptoms during pregnancy, prior to the birth of the child, allows researchers to examine whether symptoms present before the parent–child relationship has begun to develop ultimately impact parenting. Understanding how specific dimensions of trauma-related distress during pregnancy impact subsequent parenting behaviors is of particular importance given that pregnant women are at elevated risk for PTSD (Seng et al., Reference Seng, Rauch, Resnick, Reed, King, Low, McPherson, Muzik, Abelson and Liberzon2010). Further, among women with lifetime diagnoses of PTSD, symptom trajectories from pregnancy to early postpartum predict impaired bonding at 6-weeks postpartum (Muzik et al., Reference Muzik, McGinnis, Bocknek, Morelen, Rosenblum, Liberzon, Seng and Abelson2016). Researchers posit that physical changes associated with pregnancy (e.g., increased heart rate, shortness of breath) may be misattributed to anxiety and re-activate the cycle of PTSD (Blackburn, Reference Blackburn2017). In addition, vulnerability factors (e.g., past trauma) may moderate the effect of childbirth on maternal mental health or exacerbate pre-existing PTSD, thereby impacting parenting behaviors (Parfitt & Ayers, Reference Parfitt and Ayers2014).
Research aimed at explicating the link between parental PTSD and parenting could also benefit from applying dimensional models of parental psychopathology during the prenatal period that capture symptom severity rather than relying exclusively on diagnosis. Extant research examining the impact of PTSD on parenting has primarily focused on military and veteran populations or individuals meeting diagnostic criteria for PTSD. Despite the clinical significance of subthreshold symptoms (Cukor et al., Reference Cukor, Wyka, Jayasinghe and Difede2010), less research has examined the impact of subthreshold trauma symptoms on parenting and child outcomes. Further, as previously discussed, current studies examining the impact of trauma symptoms on parenting while controlling for the presence of depression or general negative affectivity are limited. Thus, these studies have been unable to isolate the role of trauma-related distress, beyond general negative affectivity, in parenting practices. Lastly, researchers have yet to investigate the role of trauma-related distress in mindful parenting, despite the fact that symptoms central to PTSD (e.g., avoidance and intrusion symptoms) are expected to undermine one’s ability to engage in present-moment awareness during parent–child interactions.
Finally, most research focuses exclusively on the role of mothers despite increasing evidence that understanding the father-child relationship and its impact on child health and development is critical to family systems research (Cabrera et al., Reference Cabrera, Volling and Barr2018; Volling et al., Reference Volling, Cabrera, Feinberg, Jones, McDaniel, Liu, Almeida, Lee, Schoppe‐Sullivan, Feng, Gerhardt, Dush, Stevenson, Safyer, Gonzalez, Lee, Piskernik, Ahnert, Karberg, Malin, Kuhns, Fagan, Kaufman, Dyer, Parke and Cookston2019). Although the intrauterine environment has received increasing attention as a potential contributor to child development (e.g., Beijers et al., Reference Beijers, Buitelaar and de Weerth2014; Glover, Reference Glover2015), mothers and fathers equally contribute to their children’s genetic makeup. A growing body of research suggests the intergenerational transmission of self-regulation is not only attributable to passive genetic transmission, but also interplay between genetic and environmental factors related to the caregiving context (Bridgett et al., Reference Bridgett, Burt, Edwards and Deater-Deckard2015). Thus, it is integral to understand the influence of both maternal and paternal prenatal psychopathology on subsequent parenting behavior and risk for child maladjustment.
In sum, longitudinal research designs linking specific dimensions of trauma-related distress experienced by both mothers and fathers during pregnancy, beyond the role of negative affectivity, to subsequent parenting during early childhood has the potential to enrich our understanding of factors that undermine attentive, nonjudgmental parenting. Further, there is a need to move beyond examinations of direct associations between parental psychopathology and mindful parenting by investigating mechanisms linking parental trauma-related distress and general negative affectivity to overreactivity, decreased sensitivity and acceptance, and diminished self- and child-awareness during parenting interactions. One such mechanism warranting closer attention is the degree to which each parent is able to develop a healthy bond with the infant after childbirth.
Parent–infant bonding as a mechanism linking parental psychopathology during pregnancy to mindful parenting
Although theory and past research recognize the impact of parental psychopathology on parenting, the mechanisms through which psychopathology impacts subsequent parenting have received considerably less attention. One potential mechanism linking parental psychopathology to deficits in mindful parenting is impaired parent–infant bonding. Bonding, a parent-driven process that emerges throughout the first year postpartum, reflects the emotional tie between a parent and their infant (Bicking Kinsey & Hupcey, Reference Bicking Kinsey and Hupcey2013) and is an important predictor of child socioemotional outcomes (de Cock et al., Reference de Cock, Henrichs, Vreeswijk, Maas, Rijk and van Bakel2016; Mason et al., Reference Mason, Briggs and Silver2011). Though limited research has examined the impact of bonding on parenting, studies suggests that bonding difficulties may detrimentally impact parenting abilities and exacerbate parenting stress (de Cock et al., Reference de Cock, Henrichs, Klimstra, Janneke, Maas, Vreeswijk, Meeus and van Bakel2017; Siddiqui & Hägglöf, Reference Siddiqui and Hägglöf2000).
A robust literature links postpartum depressive symptoms to impaired parent–infant bonding (Moehler et al., Reference Moehler, Brunner, Wiebel, Reck and Resch2006; Nonnenmacher et al., Reference Nonnenmacher, Noe, Ehrenthal and Reck2016; O’Higgins et al., Reference O’Higgins, Roberts, Glover and Taylor2013). Among mothers with postpartum anxiety, subclinical depressive symptoms, and avoidance of anxiety-provoking situations significantly predict impaired bonding, suggesting that avoidance behaviors may interfere with the developing parent–child relationship (Tietz et al., Reference Tietz, Zietlow and Reck2014). Research also suggests PTSD symptoms significantly impair postpartum bonding for both mothers and fathers, and that these difficulties are more severe among parents with comorbid PTSD and depression (Parfitt & Ayers, Reference Parfitt and Ayers2009). Further, among women with lifetime PTSD diagnoses, symptom trajectories from pregnancy to early postpartum predict impaired bonding at six-weeks postpartum (Muzik et al., Reference Muzik, McGinnis, Bocknek, Morelen, Rosenblum, Liberzon, Seng and Abelson2016). As such, negativity directed toward the infant after childbirth and a sense of disconnectedness (i.e., impaired bonding) might explain why parents experiencing higher levels of negative affectivity and trauma-related distress ultimately engage with the infant in a less responsive and sensitive manner (i.e., mindful parenting).
The present study
The aim of the present study was to test a unified framework examining the incremental effects of maternal and paternal trauma-related distress (i.e., avoidance and traumatic intrusions) and general negative affectivity (common across internalizing disorders) during pregnancy on mindful parenting during toddler age through impaired parent–infant bonding during the first six months after childbirth (see Figure 1). Building upon past research and theory, we had four primary hypotheses within this unified model.
Hypothesis 1: Maternal trauma-related distress during pregnancy will uniquely predict mindful parenting at two years postpartum both directly and indirectly through impairments in mother-infant bonding when controlling for maternal negative affectivity.
Hypothesis 2: Maternal negative affectivity during pregnancy will uniquely predict mindful parenting at two years postpartum both directly and indirectly through impairments in mother-infant bonding when controlling for maternal trauma-related distress.
Hypothesis 3: Paternal trauma-related distress during pregnancy will uniquely predict mindful parenting at two years postpartum both directly and indirectly through impairments in father-infant bonding when controlling for paternal negative affectivity.
Hypothesis 4: Paternal negative affectivity during pregnancy will uniquely predict mindful parenting at two years postpartum both directly and indirectly through impairments in father-infant bonding when controlling for paternal trauma-related distress.
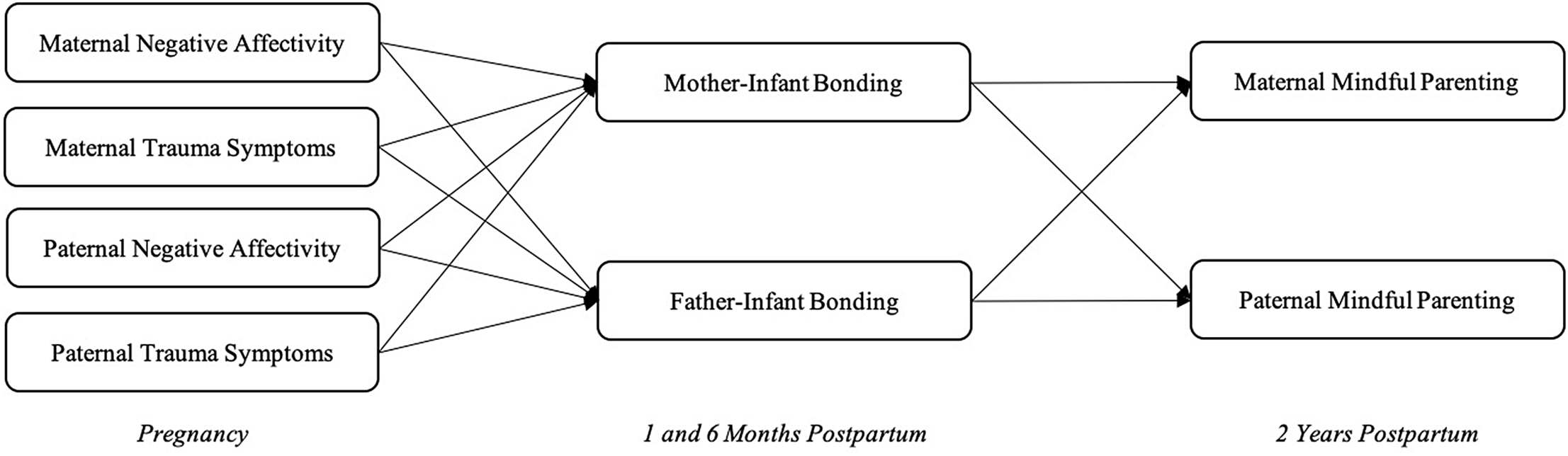
Figure 1. Conceptual model linking prenatal parental psychopathology to mindful parenting at two years postpartum via impaired parent-infant bonding at 1- and 6-months postpartum.
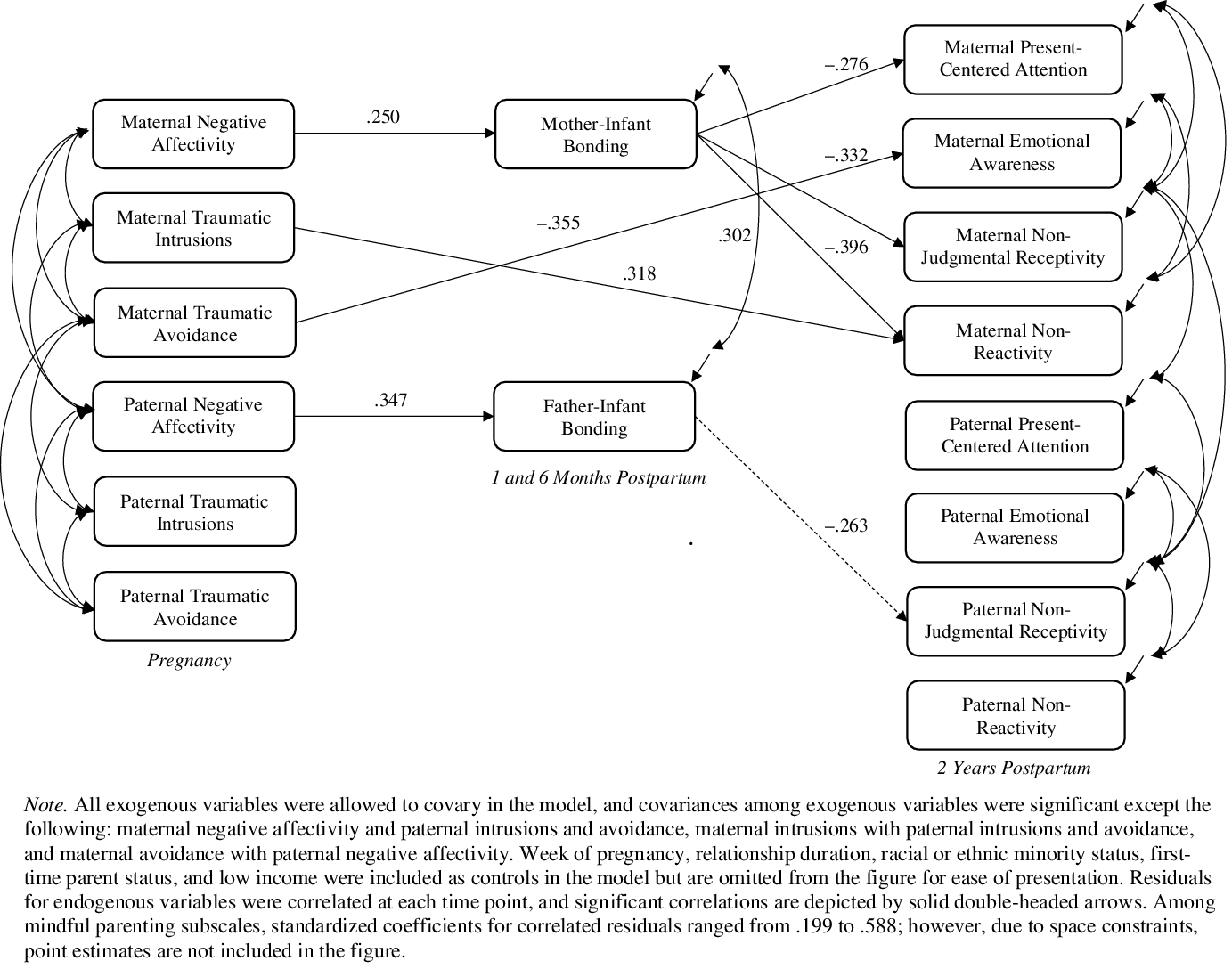
Figure 2. Results of path analysis.
Further, to explore the possibility that parental psychopathology differentially impacts facets of mindful parenting, we modeled four separate subscale scores from our measure of mindful parenting: present-centered attention, emotional awareness, nonjudgmental receptivity, and nonreactivity. However, we did not have specific hypotheses regarding which facets of mindful parenting would be impacted most by parental psychopathology or parent–infant bonding.
Method
Participants
All procedures were approved by the University of Nebraska–Lincoln Institutional Review Board. Flyers and brochures were broadly distributed to businesses and clinics frequented by pregnant women (e.g., obstetric clinics). We established cooperative arrangements with multiple agencies in the community. If an establishment permitted, members of the research team approached potential participants and provided a five-minute overview of the study along with a brochure. Eligibility criteria included that participants were: (a) 19 years of age or older (legal age of adulthood where the research was conducted), (b) English speaking, (c) pregnant at the time of the initial appointment (but not necessarily the first pregnancy to increase generalizability of results), (d) both biological parents of the child, (e) singleton pregnancy, and (f) in a committed intimate relationship and cohabiting. One hundred sixty-two couples enrolled. Three couples were excluded due to either ineligibility or invalid data for a final sample of 159 couples (159 women and 159 men).
Couples had dated an average of 81.90 months (SD = 49.59) and cohabited an average of 61.00 months (SD = 41.80) prior to study enrollment. The majority of couples were married (84.9%). Most women were in the second (38.4%) or third (58.5%) trimester of pregnancy. On average, couples already had one child living at home (SD = 1.18); 57.9% reported that they had no children and, therefore, were experiencing the transition to parenthood for the first time. In the current sample, 67% of mothers and 70% of fathers reported direct exposure to at least one potentially traumatic event on items 1 through 16 on the Life Events Checklist for DSM-5 (LEC-5; Weathers et al., Reference Weathers, Blake, Schnurr, Kaloupek, Marx and Keane2013).
Reflecting the area where the study was conducted, participants were primarily White (89.3% of women; 87.4% of men); 9.4% of women and 6.4% of men identified as Hispanic or Latino/a. On average, women were 28.67 years of age (SD = 4.27) and men were 30.56 years of age (SD = 4.52). Annual joint income ranged from less than $9,999 to more than $90,000 with a median joint income of $60,000 to $69,999, and most participants were employed at least 16 hours per week (74.2% of women; 91.8% of men). Modal education was a bachelor’s degree (46.5% of women; 34.6% of men). During follow-up assessments, it was determined that one child had been diagnosed with trisomy 21 and one mother experienced a miscarriage. As such, those families were excluded to focus on families with typically developing children (50% boys) for a final sample of 157 families.
Procedure
The present study consisted of four waves of data collection. Couples attended a laboratory appointment during pregnancy. Informed consent was obtained from both partners and, subsequently, each parent completed a series of questionnaires assessing parental psychopathology, along with other procedures beyond the scope of the present study. Subsequent waves involved parents completing surveys from home at one- and-six months postpartum, during which parent–child bonding was assessed. Parents were asked to complete surveys separately from one another as to not influence one another’s responses. Last, parents participated in a laboratory visit with their child at two years of age, during which mindful parenting was assessed using a self-report questionnaire.
Measures
Parental psychopathology during pregnancy
Parental psychopathology was assessed using the expanded version of the Inventory of Depression and Anxiety Symptoms (IDAS-II; Watson et al., Reference Watson, O’Hara, Naragon-Gainey, Koffel, Chmielewski, Kotov, Stasik and Ruggero2012). The IDAS-II is a 99-item self-report questionnaire designed to assess general and specific symptom dimensions of depression and related anxiety disorders. Compared to a categorical approach, a dimensional approach to measuring psychopathology allows researchers to gather more clinically relevant information regarding symptom severity and has higher reliability over time (Conway et al., Reference Conway, Forbes, Forbush, Fried, Hallquist, Kotov, Mullins-Sweatt, Shackman, Skodol, South, Sunderland, Waszczuk, Zald, Afzali, Bornovalova, Carragher, Docherty, Jonas, Krueger, Patalay, Pincus, Tackett, Reininghaus, Waldman, Wright, Zimmermann, Bach, Bagby, Chmielewski, Cicero, Clark, Dalgleish, DeYoung, Hopwood, Ivanova, Latzman, Patrick, Ruggero, Samuel, Watson and Eaton2019; Watson, Reference Watson2005). Participants were asked to indicate the extent to which they had experienced each symptom over the past two weeks on a scale ranging from 1 (not at all) to 5 (extremely). The 10-item Dysphoria scale reflects nonspecific, negative affectivity and captures the core affective and cognitive symptoms that span internalizing disorders (Watson et al., Reference Watson, O’Hara, Simms, Kotov, Chmielewski, McDade-Montez, Gamez and Stuart2007). There are two, 4-item scales that assess specific dimensions of trauma-related distress: Traumatic Intrusions (e.g., “I had disturbing thoughts of something bad that happened to me”) and Traumatic Avoidance (e.g., “I tried to ignore upsetting memories”). These scales show significant convergent and divergent validity with the Intrusions and Avoidance subscales on the PTSD symptom checklist, as well as the clinician rating version of the IDAS (Watson et al., Reference Watson, O’Hara, Simms, Kotov, Chmielewski, McDade-Montez, Gamez and Stuart2007). Although the Traumatic Intrusions and Avoidance scales of the IDAS do not tie symptoms to a discrete traumatic event, each item clearly refers to a stressful event (e.g., something bad/scary that happened, upsetting memories). This is consistent with other well-established measures of global trauma sequelae (e.g., the Trauma Symptom Inventory; Briere, Reference Briere1995), which demonstrate good reliability and validity across both clinical and community samples despite items not being tied to a specific trauma. Furthermore, both trauma scales on the IDAS show excellent specificity in criterion validity analyses, and the Traumatic Intrusions scale has been consistently shown to predict PTSD diagnosis (Stasik-O’Brien et al., Reference Stasik-O’Brien, Brock, Chmielewski, Naragon-Gainey, Koffel, McDade-Montez, O’Hara and Watson2019). Scores on the Dysphoria, Traumatic Intrusions, and Traumatic Avoidance scales were internally consistent (Cronbach’s α = 0.83, 0.81, and 0.88, respectively). Importantly, in the present sample, participants without a history of trauma (as objectively defined by items 1 through 16 on the LEC-5) endorsed virtually no trauma-related distress (median = 4, mode = 4; a score of “4” on this scale reflects the absence of symptoms).
Parental bonding during infancy
Postpartum bonding was assessed at one- and six-months postpartum using the Impaired Bonding scale of the Postpartum Bonding Questionnaire (PBQ; Brockington et al., Reference Brockington, Oates, George, Turner, Vostanis, Sullivan, Loh and Murdoch2001). The PBQ is a 25-item, factor-analytically derived, self-report measure assessing parental feelings or attitudes toward their infant. The Impaired Bonding scale consists of 12 items and demonstrates both sensitivity in detecting bonding disorders and high predictive validity (Brockington et al., Reference Brockington, Oates, George, Turner, Vostanis, Sullivan, Loh and Murdoch2001; Perrelli et al., Reference Perrelli, Zambaldi, Cantilino and Sougey2014). Parents were asked to rate their agreement with a series of statements on a 6-point Likert scale. Positive responses (e.g., “I feel close to my baby”) were scored from 0 (always) to 5 (never), while negative responses (e.g., “My baby irritates me”) were scored from 0 (never) to 5 (always). Items for the Impaired Bonding scale were summed to generate a final score, with low scores denoting good bonding and high scores indicating impaired bonding. Scores at one- and six-months postpartum were internally consistent (Cronbach’s α = 0.82 at one-month and Cronbach’s α = 0.78 at six-months) and highly correlated across time points for both mothers (r = 0.68, p < .001) and fathers (r = 0.75, p < .001). Thus, the repeated scores for each parent were aggregated across time points to create robust scores of impaired parent–infant bonding during the first six months postpartum.
Mindful parenting during toddler age
Mindful parenting was assessed using the Interpersonal Mindfulness in Parenting Scale (IEM-P; Duncan, Reference Duncan2007). Parents were asked to rate each item on a 5-point Likert scale. Positive responses (e.g., “I am aware of how my moods affect the way I treat my child”) were scored from 0 (always) to 5 (never), while negative responses (e.g., “I often react too quickly to what my child says or does”) were scored from 0 (never true) to 5 (always true). The IEM-P was originally developed as a 10-item self-report measure designed to capture three aspects of mindful parenting: present-centered awareness and attention, nonjudgmental receptivity, and nonreactivity. However, factor analyses suggested that mindful parenting would be better represented by four first-order factors comprised of 2 items each “to distinguish between the cognitive and affective aspects of present-centered awareness and attention” (p. 36; Duncan, Reference Duncan2007). As such, in the present study, we focused on the 8 items that were retained in the original scale development article (Duncan, Reference Duncan2007). To guide scoring decisions, we conducted a series of confirmatory factor analyses (CFAs) comparing three measurement models with the 8 items: a four-factor model (i.e., 2 items loading to each of the four subscales as identified in Duncan, Reference Duncan2007), a single-factor model (i.e., all 8 items loading to a single factor), and a higher-order factor model (i.e., the four factors loading to a higher-order single factor). Models including the subscale factors required equality constraints for the two indicators loading to each factor given relatively small correlations among some of the factors. Please refer to Table 1 for detailed information about model fit demonstrating that the four-factor solution demonstrated superior fit and was the only solution with adequate global fit. Closer inspection of the four-factor solution revealed that all items were salient indicators of each factor (factor loadings > .40). Two factors – present-centered attention and emotional awareness – had a non-significant correlation (r = .09, p = .48), further supporting the examination of separate factors. Referring to Table 2, it was also evident that there was unique criterion validity for each subscale in relation to other variables of interest in the present study. For example, maternal present-centered attention was significantly associated with maternal negative affectivity (r = −.20) and impaired bonding (r = −.25), whereas maternal emotional awareness was significantly associated with maternal traumatic avoidance (r = −.24).
Table 1. Factor structure of IEM-P

Note. CFI = comparative fit index, RMSEA = root mean square error of approximation, AIC = Akaike information criterion, BIC = Bayesian information criterion, SBIC = sample-size adjusted BIC. Four-factor = model with 2 items from each subscale loading to each of four factors identified by Duncan (Reference Duncan2007). Single-factor = model with all 8 items loading to a single factor. Higher-order = model with four subscale factors (each with 2 indicators) loading to a higher-order factor. Only the four-factor solution demonstrated adequate global fit based on CFI > .90 and RMSEA < .10. The four-factor solution was also deemed to have superior fit as evidenced by the smallest AIC, BIC, and SBIC values (bolded); factor loadings for all items were greater than .40. Values are bolded for the four-factor solution to demonstrate superiority.
Table 2. Correlations and descriptive statistics

Note. P = paternal, M = maternal.
*p < .05. **p < .01. ***p < .001.
In sum, although we did not have specific hypotheses about how parental psychopathology and bonding impact distinct facets of mindful parenting, item-level analysis of the IEM-P supports a four-factor solution. Therefore, subscales are represented as distinct variables in the final model. Four dimensions of mindful parenting were examined in the present study: present-centered attention (e.g., “I rush through activities with my child without really being attentive to him/her”; cognitive aspect), emotional awareness (e.g., “I notice how changes in my child’s mood affect my mood”; affective aspect), nonjudgmental receptivity (e.g., “I listen carefully to my child’s ideas, even when I disagree with them”), and nonreactivity in parenting interactions (e.g., “When I am upset with my child, I calmly tell him/her how I am feeling”). Mean scores were computed for each subscale, with higher scores indicating more mindful parenting. As expected based on the confirmatory factor analyses, scores computed with the two items from each subscale were internally consistent, with inter-item correlations ranging from .33 to .56 (Clark & Watson, Reference Clark and Watson1995), and correlations among the subscale scores ranged from −.03 to .52 for mothers and −.07 to .61 for fathers, further demonstrating discriminant validity.
Data analytic plan
The model depicted in Figure 1 was analyzed using path analysis in Mplus (Muthén & Muthén, Reference Muthén and Muthén2017). Missing data were addressed with maximum likelihood estimation (covariance coverage ranged from .64 to 1.00; Enders, Reference Enders2010). Only marital status during pregnancy had a consistent association with probability of missing a follow-up assessment, such that unwed couples were more likely to miss assessments; however, these associations were relatively small in magnitude (rs ranged from −.27 to −.18). We conducted a sensitivity analysis including marital status as an auxiliary variable, consistent with a saturated correlates model (Enders, Reference Enders2010), and confirmed that the pattern of results replicated.
Data were analyzed using actor-partner interdependence modeling for distinguishable dyads (APIM; Kenny et al., Reference Kenny, Kashy and Cook2006), such that the couple is the unit of analysis. Accordingly, both actor paths (e.g., maternal trauma-related distress predicting maternal mindful parenting) and partner paths (e.g., maternal trauma-related distress predicting paternal mindful parenting) were tested, and maternal and paternal variables were covaried to account for interdependence. Residuals for maternal and paternal endogenous variables were correlated at each time point to account for interdependence across members of a dyad (e.g., maternal and paternal reports) and among subscales from the same measure (i.e., mindful parenting subscales). Although the hypothesized pathways were comprised solely of actor effects (e.g., maternal trauma-related distress → impaired mother-infant bonding → less mindful parenting by mothers), by testing the integrated model with both maternal and paternal variables, we were able to explore partner paths as well (e.g., whether paternal trauma-related distress reported during pregnancy undermines mother-infant bonding).
A series of theoretically meaningful demographic and family characteristics thought to impact parent–infant bonding and mindful parenting were included as control variables, including interparental relationship duration, low income, minority racial or ethnic status, and first-time parenthood status (all measured during pregnancy). Low income status was dichotomized based on the median household income in Nebraska at the time of study enrollment (categorized as low income [<$60,000/year; 47.8% of sample] or high income [>$60,000/year]). We also controlled for the week of pregnancy when the initial appointment occurred to account for differing time intervals between the pregnancy and follow-up assessments across participants.
Given that the mediation model was just identified, global model fit was not assessed. A nonparametric resampling method (bias-corrected bootstrap) with 10,000 resamples drawn was performed to derive the 95% confidence intervals for direct and indirect effects (Preacher et al., Reference Preacher, Rucker and Hayes2007). Bias-corrected bootstrapped confidence intervals were used to determine significant effects (both direct and indirect), as they are robust to violations of univariate and multivariate normality. Code and individual-level data are available upon request from the corresponding author pending IRB approval for data sharing.
Results
Descriptive statistics and correlations are reported in Table 2. As expected for a community sample, levels of parental psychopathology during pregnancy were relatively low, though there was notable variance, as were impairments in bonding during the first six months postpartum. There were large correlations between dimensions of paternal psychopathology (negative affectivity, intrusions, and avoidance; r ranging from .47 to .63) and moderate to large correlations between dimensions of maternal psychopathology (r ranging from .44 to .72). Of note, the correlation between maternal traumatic intrusions and traumatic avoidance exceeded the threshold for collinearity (r > .70; Tabachnick & Fidell, Reference Tabachnick and Fidell2012). However, an examination of tolerance statistics and variance inflation factors (VIF) confirmed there were no violations of multicollinearity, as tolerance values were above 0.20 and VIFs did not exceed 4.0 (maternal traumatic avoidance, tolerance = .46, VIF = 2.17; maternal traumatic intrusions, tolerance = .42, VIF = 2.38; Hair et al., Reference Hair, Black, Babin and Anderson2018).
Results of path analysis
Full model results are reported in Table 3 and depicted in Figure 2. We now turn to a summary of the results for each of the primary study hypotheses, including tests of indirect effects (reported in Table 4). Notably, although we included partner paths in the model, none of those paths were statistically significant, suggesting that (a) one person’s psychopathology is not associated with their partner’s parenting or their ability to bond with their infant, and (b) the bond between one parent and their infant is not associated with the other parent’s ability to parent mindfully.
Table 3. Final results of hypothesized model

Note. Model results after controlling for week of pregnancy, relationship duration, racial or ethnic minority status, first-time parent status, and low income based on the median household income in Nebraska at the time of study enrollment (categorized as low income [<$60,000/year] or high income [>$60,000/year]). Bias-corrected bootstrapped confidence intervals (CIs) were calculated to determine significance of effects. If a CI did not contain zero, the effect was significant; significant effects are bolded.
a 95% CI based on 10,000 bootstrapped samples.
Table 4. Summary of significant direct and indirect effects of parental prenatal psychopathology on mindful parenting during toddler age

Hypothesis 1: Contrary to our hypothesis, there was no evidence of an indirect effect of maternal trauma-related distress on dimensions of mindful parenting through impaired mother-infant bonding when controlling for maternal negative affectivity. However, when controlling for negative affectivity, traumatic intrusions, mother-infant bonding, and paternal psychopathology and bonding, a negative direct effect of maternal prenatal traumatic avoidance on emotional awareness emerged, 95% CI [−.204, −.018]. In addition, there was an unexpected, positive direct effect of maternal prenatal traumatic intrusions on nonreactivity during parenting interactions, 95% CI [.009, .183].
Hypothesis 2: The indirect effects of maternal negative affectivity on present-centered attention, 95% CI [−.020, −.002]; nonjudgmental receptivity, 95% CI [−.024, −.002]; and nonreactivity in parenting interactions, 95% CI [−.028, −.003], at two years postpartum through impaired mother-infant bonding were significant.
Hypothesis 3: Contrary to our hypothesis, there were no significant indirect effects of paternal prenatal trauma-related distress on mindful parenting through impaired father-infant bonding, nor did paternal trauma-related distress directly predict dimensions of mindful parenting.
Hypothesis 4: The indirect effect of paternal negative affectivity on nonjudgmental receptivity at two years postpartum via impaired father-infant bonding during the first six months postpartum, 95% CI [−.033, −.001], was significant.
Discussion
The goal of this study was to examine the unique effects of maternal and paternal trauma-related distress (i.e., traumatic intrusions and avoidance) and general negative affectivity (i.e., low mood, anhedonia, difficulties concentrating) during pregnancy on mindful parenting during toddler age through impaired parent–infant bonding. In general, results demonstrate the impact of parental psychopathology during pregnancy, prior to the birth of the child, on mindful parenting more than two years later. Specifically, results indicate that unique dimensions of maternal trauma-related distress during pregnancy have direct associations with specific facets of mindful parenting when controlling for negative affectivity and parent–infant bonding. Further, general negative affectivity, which underlies internalizing disorders, is associated with several dimensions of mindful parenting among both mothers and fathers through impaired parent–infant bonding.
The role of traumatic avoidance and intrusions in mindful parenting
Maternal trauma-related distress during pregnancy was uniquely associated with certain elements of mindful parenting, even when controlling for the underlying general negative affectivity common among PTSD and other internalizing disorders such as depression; however, this association was not explained by impaired mother-infant bonding. Specifically, avoidance symptoms during pregnancy appeared to interfere with maternal emotional awareness during parenting interactions with their toddlers. This finding suggests that mothers who engage in more avoidance to suppress their own negative emotions may experience greater difficulties recognizing when their emotions impact their parenting behaviors. Notably, mother-infant bonding difficulties did not mediate the association between maternal avoidance and mindful parenting in the present study. Thus, it may be that maternal avoidance directly impacts parenting behaviors. This finding builds upon research highlighting the impact of avoidance on increased withdrawal, insensitivity, and non-responsivity in observed parenting behaviors, as well as decreased positive engagement (Brockman et al., Reference Brockman, Snyder, Gewirtz, Gird, Quattlebaum, Schmidt, Pauldine, Elish, Schrepferman, Hayes, Zettle and DeGarmo2016; van Ee et al., Reference van Ee, Kleber, Jongmans, Mooren and Out2016).
Contrary to our hypothesis that both traumatic intrusions and avoidance would impair mindful parenting, higher levels of maternal intrusion symptoms during pregnancy were associated with increased nonreactivity during parenting interactions. That is, mothers who experienced more intrusive memories tended to notice and consider their own negative emotions before responding to their children during parenting interactions. Notably, this effect was present only when controlling for traumatic avoidance and negative affectivity (and other model controls), suggesting that maternal intrusions, distinct from other dimensions of internalizing symptoms, might enhance nonreactivity during parenting interactions. One potential explanation for this unexpected finding is that mothers experiencing more intrusion symptoms (i.e., unwanted thoughts/memories of something bad that happened) are more consistently confronted with their emotions, and this increased engagement with their internal experiences might result in mothers being more aware of their emotions in the context of parenting interactions. This would suggest that it may not be the presence of intrusion symptoms that negatively impacts parenting, but rather the ways in which mothers cope with these symptoms (e.g., by avoiding thoughts, feelings, places associated with the unpleasant event) that interfere with the ability to parent mindfully. Alternatively, it may be that after accounting for shared variance with negative affectivity and avoidance, the traumatic intrusions subscale captures a degree of willingness to approach unwanted thoughts and feelings, which in turn predicts more mindful parenting. However, this novel and unexpected finding requires replication before more definitive interpretations can be made, especially given the exploratory nature of the analyses examining distinct dimensions of mindful parenting. Interestingly, there were no direct or indirect effects of trauma symptoms reported by fathers on dimensions of mindful parenting within this unified framework. Thus, it appears that prenatal trauma-related distress among mothers, but not fathers, might be most influential with regard to subsequent mindful parenting during toddler age.
Impaired bonding mediates the effect of negative affectivity on mindful parenting
For both mothers and fathers, negative affectivity during pregnancy predicted parent–infant bonding impairments over the first six months postpartum. Further, significant indirect effects emerged from maternal negative affectivity to present-centered attention, nonjudgmental receptivity, and nonreactivity through impaired mother-infant bonding, suggesting that maternal negative affectivity is a robust predictor of deficits in multiple aspects of mindful parenting. Similarly, there was a significant indirect effect of paternal negative affectivity on nonjudgmental receptivity through impaired father-infant bonding during the first six months postpartum. This finding suggests that higher levels of negative affectivity during pregnancy interfered with father-infant bonding, which subsequently impacted fathers’ ability to be open and nonjudgmental in parenting interactions with their toddlers.
Given the lack of empirical and theoretical guidance, we did not offer a priori hypotheses about which dimensions of mindful parenting would be undermined by paternal psychopathology during pregnancy; however, it is notable that paternal negative affectivity specifically undermined nonjudgmental receptivity (i.e., allowing their toddler to express their ideas or emotions despite disagreeing with them), whereas maternal negative affectivity exerted more global effects on mindful parenting. One possible explanation is that paternal negative affectivity may contribute to a negative perceptual bias (e.g., depression-distortion hypothesis; Gartstein et al., Reference Gartstein, Bridgett, Dishion and Kaufman2009; Richters, Reference Richters1992), thereby increasing the likelihood that fathers perceive their toddlers’ behaviors as negative. These fathers may, in turn, perceive their toddlers’ behaviors as negative may experience greater difficulty remaining non-judgmental during parenting interactions. Future research examining how psychopathology differentially impacts mindful parenting behaviors among fathers versus mothers (in dual-parenting households comprised of heterosexual couples) is needed to test these hypotheses.
Taken together, these findings are consistent with a large body of literature on the impact of parental depressive symptoms on parent–infant bonding (Moehler et al., Reference Moehler, Brunner, Wiebel, Reck and Resch2006; Nonnenmacher et al., Reference Nonnenmacher, Noe, Ehrenthal and Reck2016), as well as research suggesting parents with both PTSD and depression experience more severe bonding difficulties (Parfitt & Ayers, Reference Parfitt and Ayers2009). Further, the present study extends past research by identifying the underlying dimension of negative affectivity common to mood and anxiety disorders as driving these effects. Notably, unlike past research examining PTSD and depression symptomology within a categorical framework among individuals meeting diagnostic criteria, the dimensional approach utilized here revealed that parental trauma-related distress did not predict impairments in bonding. This suggests that the underlying negative affectivity common to internalizing disorders, rather than trauma-specific symptom clusters, contributes to bonding difficulties. Although rates of psychopathology were relatively low, as expected for a community sample, rates were comparable to other studies examining dimensional symptoms among pregnant samples (Grekin et al., Reference Grekin, O’Hara and Brock2021). Nonetheless, maternal traumatic avoidance did exert a negative, direct influence on mindful parenting of toddlers, and future research is needed to understand potential mechanisms explaining this association.
Theoretical and empirical implications
Before turning to implications, several limitations of the present study should be considered. First, the sample was comprised of heterosexual, cohabiting couples who primarily identified as White and were from middle-class backgrounds, thereby limiting the generalizability of the results; thus, research examining similar processes among more diverse populations (e.g., among sexual and racial minorities) is needed. Further, the present study focused on a community sample rather than a clinical sample, and additional research is needed to understand how results might differ for parents experiencing clinically significant levels of psychopathology during pregnancy. Although the majority of participants reported exposure to at least one potentially traumatic event on the LEC-5, our measurement of parental psychopathology was dimensional and therefore not designed to assess PTSD categorically as consistent with DSM-5 diagnostic criteria. Nonetheless, by examining parental psychopathology dimensionally, we demonstrated that specific dimensions of trauma-related distress may impact parenting even if they do not reach clinical or diagnostic significance.
Second, mindful parenting was only assessed at two years postpartum; therefore, we could not control for change processes occurring over time. A next step in this research is to examine if and how mindful parenting evolves and changes during early childhood, and whether parental psychopathology and parent–infant bonding influence this dynamic process. It is also important to note that the IEM-P was originally designed to assess mindful parenting among parents of adolescents. The IEM-P is also limited to only 2 items per dimension of mindful parenting, and past research has largely relied on a total scale score. In the present study, a series of confirmatory factor analyses suggested that mindful parenting may not be unidimensional in nature. Further, there was evidence of unique criterion validity for each subscale score. As such, it will be important for future research to investigate the factor structure of mindful parenting with a particular focus on investigating measurement invariance across different developmental stages (e.g., toddlerhood to preschool-age). Studies exploring the unique antecedents and consequences of distinct dimensions of mindful parenting (e.g., emotional awareness), perhaps utilizing expanded scales covering more features of each dimension, are also warranted. For instance, a Dutch measure (IM-P) builds on items in the IEM-P by measuring additional facets of mindful parenting (e.g., self-regulation in parenting, compassion for self and child) and has been validated among parents of adolescents (de Bruin et al., Reference de Bruin, Zijlstra, Geurtzen, van Zundert, van de Weijer-Bergsma, Hartman, Nieuwesteeg, Duncan and Bögels2014) with exploratory factor analyses revealing a six-factor structure.
Third, all data were collected using self-report questionnaires, raising the possibility of shared method bias; however, a recent study found self-reported mindful parenting to be closely related to observable parenting behaviors (Duncan et al., Reference Duncan, Douglas Coatsworth, Gayles, Geier and Greenberg2015). Nonetheless, future studies utilizing observational measures would enhance our understanding of how parental psychopathology impacts mindful parenting.
Finally, given the limited literature addressing trauma-related psychopathology and mindful parenting, we did not offer hypotheses regarding the particular dimensions of mindful parenting that might be impacted by parental psychopathology during pregnancy. Future research is needed to replicate findings and make more definitive conclusions about the specific ways in which parental psychopathology differentially impacts bonding and subsequent mindful parenting behaviors.
Despite these limitations, the present study has several theoretical and practical implications. First, it highlights the potential impact of negative affectivity on bonding impairments and subsequent parenting difficulties and supports a growing body of literature emphasizing the importance of examining the unique contributions of both mothers and fathers in family systems research (Cabrera et al., Reference Cabrera, Volling and Barr2018; Volling et al., Reference Volling, Cabrera, Feinberg, Jones, McDaniel, Liu, Almeida, Lee, Schoppe‐Sullivan, Feng, Gerhardt, Dush, Stevenson, Safyer, Gonzalez, Lee, Piskernik, Ahnert, Karberg, Malin, Kuhns, Fagan, Kaufman, Dyer, Parke and Cookston2019). Second, our finding that maternal avoidance symptoms during pregnancy contribute to diminished emotional awareness in parenting interactions during toddler age provide support for examining prenatal trauma-related distress reported by parents in the context of parental meta-emotion philosophy and the perinatal interactional model. Specifically, mothers who report more avoidance symptoms during pregnancy may experience greater emotional dysregulation, which could subsequently interfere with their ability to recognize how their own emotions, as well as their child’s emotions, impact their parenting behaviors. In addition, the present study informs the action-control framework, which posits that parental psychopathology interferes with child-oriented action through impairments in internal processes (e.g., cognitive, affective). Results suggest the possibility—which could be tested in future work—that maternal traumatic avoidance may contribute to difficulties in mindful parenting by interfering with affective processes (e.g., emotional awareness), whereas underlying negative affectivity may undermine cognitive aspects of mindful parenting (e.g., present-centered attention) through impaired bonding.
Taken together, the current findings highlight the lasting impact of parental psychopathology, in the form of general negative affectivity and, to a lesser extent, trauma-related distress during pregnancy, on subsequent parenting behaviors. Consistent with literature on perinatal distress, depression, and anxiety (e.g., Austin, Reference Austin2004), early intervention efforts to reduce subthreshold symptoms of prenatal psychopathology among mothers and fathers may promote healthy bonding with infant and optimal parenting behaviors, which, subsequently contributes to more adaptive child socioemotional outcomes. Indeed, mindfulness training during the prenatal period may not only buffer the effects of prenatal stress, but also improve parental awareness and self-regulation, thereby allowing parents to devote more emotional resources to responding to distressed children and enhancing the overall parent–child relationship (Potharst et al., Reference Potharst, Aktar, Rexwinkel, Rigterink and Bögels2017; Shaddix & Duncan, Reference Shaddix, Duncan, Ivtzan and Lomas2016). Further, among mothers with subthreshold levels of trauma-related distress, additional prevention efforts targeting avoidance behaviors and bolstering emotional awareness (e.g., mindfulness techniques, in vivo exposure to feared stimuli) may be warranted. Last, given that pregnant women and their partners engage more regularly with the healthcare system, models of integrated perinatal care offer an ideal opportunity for increased screening and intervention efforts (Lomonaco-Haycraft et al., Reference Lomonaco-Haycraft, Hyer, Tibbits, Grote, Stainback-Tracy, Ulrickson, Lieberman, van Bekkum and Hoffman2019).
Acknowledgements
This research was funded by several internal funding mechanisms awarded to PI Rebecca Brock from the University of Nebraska-Lincoln (UNL) Department of Psychology, the Nebraska Tobacco Settlement Biomedical Research Development Fund, and the UNL Office of Research and Economic Development. We thank the families who participated in this research and the entire team of research assistants who contributed to various stages of the study. In particular, we thank Erin Ramsdell, Jennifer Blake, and Kailee Groshans for project coordination.
Conflicts of Interest
None.









