Introduction
CHD is the most common birth defect worldwide, with many patients requiring surgery before adulthood.Reference MacGillivray and Lin1,Reference Reller, Strickland, Riehle-Colarusso, Mahle and Correa2 Although advancements in care improved the mortality of CHD,Reference Spector, Menk and Knight3 morbidity still exists, impacting families. Patients experience this reality not only in terms of physical health but also psychological health and overall quality of life.Reference Brown, Pagel and Ridout4–Reference Francis, Prothasis, George and Stoica6 Consequently, providers are shifting their attention towards management strategies that improve experiences both within and outside of the hospital for families.
Specifically, returning to baseline in the early surgical recovery phase is an area of potential improvement, as little is known about the family experience during this time. One recent project analysed the effects of peri/postoperative CHD morbidities on familial and patient quality of life, with an overall negative impact at 6 weeks, but normalising by 6 months after surgery.Reference Wray, Ridout and Jones7,Reference Wray, Ridout and Jones8 Still, a recent systemic review found only 10 articles that examined the transition home in terms of quality of life for CHD families across almost 30 years (1989–2016).Reference March9 In brief, more robust data about family perspectives could help providers better serve patients throughout these first weeks home after surgery.
To complicate this peri/postsurgical dilemma, standardised protocols in symptom management for surgical paediatric patients do not readily exist. Pain management guidelines for CHD patients are more recently being created,Reference Gal, Clyde and Colvin10 but direction still lacks concerning the other plethora of symptoms that traditionally have been considered necessary side effects of the early postoperative phase. An “Enhanced Recovery After Surgery” program addresses this need for patients.11 Enhanced Recovery After Surgery, while widely implemented in adult surgery, is only recently being utilised in paediatrics. Within our centre, we have implemented such a program, with the goals of minimising opiates, nausea/vomiting, delirium, and delayed ambulation. This project ultimately aims to enhance patient-centred experiences of paediatric patients and families after CHD surgery.
While the Enhanced Recovery After Surgery program heavily targets inpatient postsurgical recovery, the transition and early period at home postoperatively is a time period of further potential intervention and improvement. This preliminary project specifically aims to qualitatively understand CHD family perspectives on the immediate postoperative recovery phase early after returning home by assessing family experiences within the Enhanced Recovery After Surgery program.
Materials and methods
This qualitative assessment of families was carried out within the scope of a broader implementation of an Enhanced Recovery After Surgery program. Patients aged 4–21 years undergoing cardiac surgery at a large volume centre were included. Inclusion cohort was initially focused to high-volume, relatively low acuity conditions with anticipated postoperative trajectories based on the complexity and historical knowledge of the surgery. The cohort was then broadened in a step-wise approach to include all patients ≥4 years old and patients of any age undergoing the Fontan surgery, with the exclusion of major developmental delay or undergoing a repair combining multiple lesions or far outside the normal time period for such surgery.
For six months from April 2023 to December 2023, patients meeting eligibility criteria were identified and deemed Enhanced Recovery After Surgery patients. Only Enhanced Recovery After Surgery patients were included in this cohort to assess early post-discharge symptoms and barriers. Prior to surgery, patients (and parents) met at a preoperative meeting with a nurse navigator. On the day of surgery, they were enrolled in the Enhanced Recovery After Surgery program by the surgeons and information was also shared from the anaesthesia team. During the patient hospitalisation, a checklist was placed on the patient chart and door indicating they were an Enhanced Recovery After Surgery patient, with goals transparently expressed to all stakeholders (surgeons, anaesthesia, nurses, fellows, advanced practice practitioners, and paediatric specialists), but without prescriptive processes to be followed.
Targeted goals included minimising opiate exposure, early ambulation, limiting delirium, nausea and emesis, and early extubation in the operating room whenever possible. All stakeholders involved in care were notified beforehand both via a daily email that includes upcoming surgeries and during a preoperative multidisciplinary conference.
Following the patients’ hospitalisation, during which patients spent time in the ICU and the general cardiology floor, patients were discharged and their contact information (email and phone) was recorded in the medical record, as is standard for all patients in the institution. At one month post-surgery, families were contacted via a hospital-specific phone number by a member of the research team (K.B., K.H.). If there was no response, the team attempted to contact the family three times within a 3 months postoperative timeframe (Figure 1). Contact strategy was consistent with healthcare-related survey methodology guidelines from the Dillman total design survey method.Reference Hoddinott and Bass12
Figure 1. A diagram of the Enhanced Recovery After Surgery (ERAS) program, readily used in adult surgery, and more recently being applied to pediatrics. This study assesses the CHD family experience within the first week home after partaking in this program.
Each family was asked the same questions in the same order and manner. Questions targeted the first week at home following discharge and included a combination of open-ended questions and a review of a list of symptoms and whether or not those symptoms were present. The questions were reviewed by both content experts and qualitative research experts prior to disseminating to families.
Observational data analysis was completed comparing responses via means, medians, and simple percentages. Qualitative measurement was conducted via thematic analysis utilising language clustering with open-ended questions. Our institutional review board approved the entirety of this study. Consent was not obtained as data were collected as part of an operational improvement project.
Results
Over a period of six months, there were 27 patients enrolled in the Enhanced Recovery After Surgery program, 23(85%) of which their parent was successfully contacted and agreed to responding to follow-up questions (Table 1). Of those who did not report their post-discharge course, two (7%) had complicated courses resulting in either an unexpected mortality for one patient and a very prolonged hospital course for another. One (3.5%) patient’s family was never able to be reached via contact information and an additional one (3.5%) declined.
Table 1. Surgical repair and demographics of patients contacted in the early post-operative period for this preliminary study
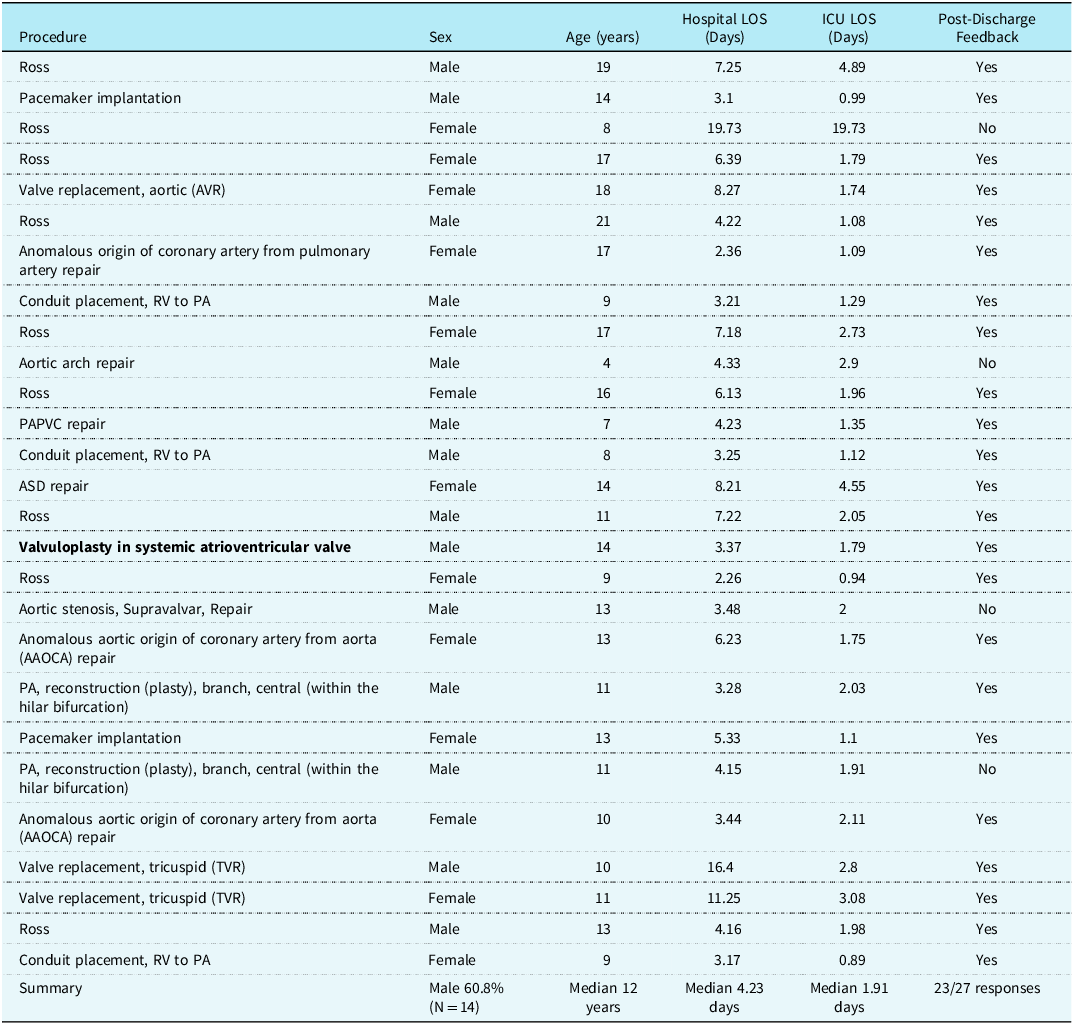
Of patients whose parents responded, 14 were male (60.8%) and median age was 12 years (4–21). Fifteen of the 23 patients (65%) were geographically from out of state, which is consistent with patients undergoing heart surgery within the institution, which covers a geographic region of five states. All patients went directly home following discharge, without any time in a skilled nursing facility or any other medical institution.
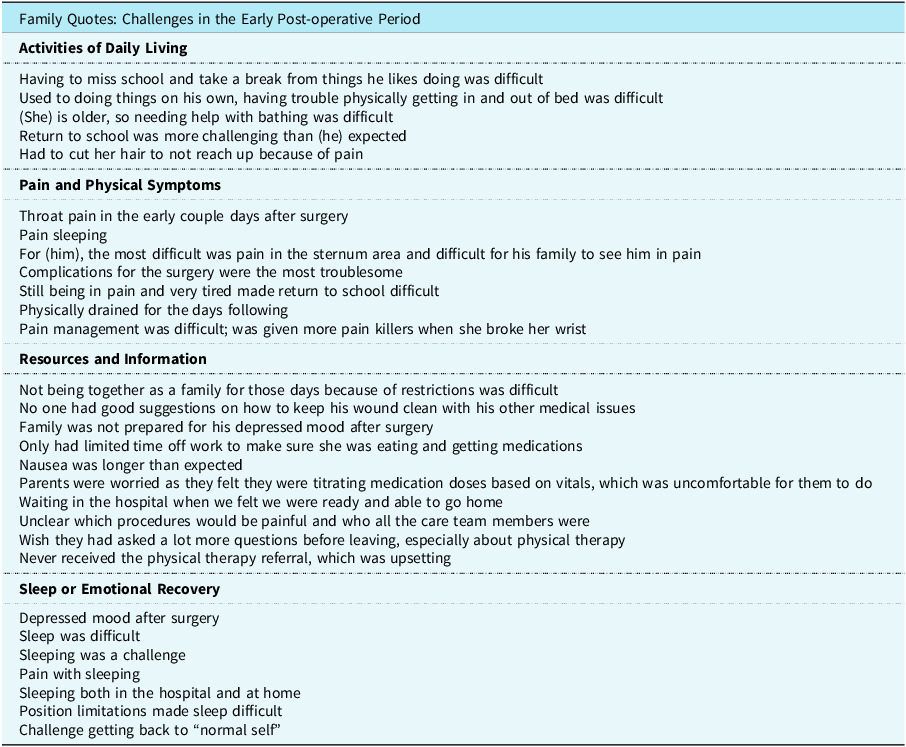
Open-ended responses were categorised by qualitative analysis of what was the “most challenging part” and the “easiest part” of recovery (Table 2). The categories that “challenging” responses clustered to were sleep challenges (N = 18, 18%), activity of daily living (N = 9 [39%] including returning to activity [N = 6, 26%] and difficulty taking medications [N = 3, 13%]), pain and physical symptoms (N = 9 [39%] including pain [N = 13, 57%], constipation or other bowel or urinary difficulty [N = 8, 35%]), appetite changes [N = 5, 22%] and nausea [N = 2, 8%]), and lack of resources or expectations following discharge (N = 9, 39%). The categories that “easiest” responses clustered to were similar for different patients, with pain and physical symptoms (N = 8, 35%), satisfaction with resources and expectations (N = 7, 30%), quick return to activities of daily living (N = 5, 22%), and ease of sleep or emotional recovery (N = 4, 17%).
Table 2. CHD family quotes concerning their experiences and symptoms during the first week home after surgery
When asked if a variety of standard topics were challenging in the first 7 days at home, parents responded with results outlined in Figure 2. Of note, participants struggled most with sleep (78%), returning to activity (70%), and pain (57%).

Figure 2. Family responses to being asked whether or not specific challenges were experienced within seven days following discharge of their admission for surgery.
Discussion
To optimally serve patients and families in recovery from CHD surgery, understanding needs and challenges early upon discharge home is necessary. Rehabilitation back to baseline state, while supported by early recovery and symptom mitigation in the hospital, must continue in the early phase at home after surgery. In the first week home after surgery, families enrolled in the Enhanced Recovery After Surgery program struggled most with sleep, activity level, and pain. Challenges faced commonly while in the hospital, such as nausea or vomiting, feeding, urinary or bowel difficulties, were less commonly cited. These findings, while informative for future iterations of the local Enhanced Recovery After Surgery program, are new data about a time period rarely assessed in the CHD literature.
Sleep
Sleep difficulties, while expected in the hospital, was the most frequent symptom and complaint encountered in the home environment. The impact of sleep on healing and recovery is clear: lack of adequate sleep increases metabolic requirements, alters immune competence, and increases pain.Reference Smith, Besunder and Betters13 The many family responses citing pain as a contributing factor to poor sleep are therefore fairly understandable. Consequently, ensuring that patients have adequate pain regimens for home could address not only pain complaints, but also improve sleep by breaking this cycle of symptoms.
A frequently mentioned issue contributing to poor sleep involved positioning. Many children preferred to sleep prone, which cannot occur immediately for every patient post-sternotomy. While few interventions can likely address this problem before proper healing, noting its importance to families can help providers monitor patient recovery more purposefully. For older children and adolescents, lack of sleep (and the relationship with pain as mentioned) contributed to challenges returning to school, further exacerbating delay with return to baseline status.
Efforts have been made to study interventions that enhance sleep for postsurgical CHD families, including providing sleep masksReference Dai, Xie, Liu, Chen and Cao14 and parental educational interventions for surgical expectations and support.Reference Jin, Chen, Fang, Li, Yang and Liu15 Both are relatively cost effective, and could further address sleep difficulties faced by many postsurgical CHD families. Better understanding of sleep regimens and the barriers to effective sleep for CHD families will be vital in enhancing their quality of life.
Activity level
Returning to baseline daily activity is a common postoperative goal for both providers and families, as suggested during our interviews. Barriers reported by families include pain and lack of guidance. Prolonged immobility can increase the risk of weakness and delirium, while early mobility likely reduces complications and comorbidities in critically ill patients during their recovery phaseReference Smith, Besunder and Betters13 Addressing this need would therefore not only better quality of life but also likely medical outcomes. While this was an intervention of the broader inpatient focus of the Enhanced Recovery After Surgery program, and even with widespread efforts within critical care to address early ambulation in the hospital, continued focus on early ambulation in the early home phase is not reported.
Of particular concern for children with CHD is the historical reality that they live more sedentary lifestyles. This may be in part from physiologic limitations, but data suggest contribution from parental overprotection, viewing the child as fragile and with limited self-efficacy.Reference Reybrouck and Mertens16,Reference Ramanan, Lee, Maharajh, Webster and Longmuir17 Exercise training programs for children with CHD, particularly those with palliative surgeries with the expectation of peak exercise limitations, offers a path forward to ensure adequate fitness.Reference Duppen, Takken and Hopman18 Currently, work is being developed specifically for CHD families receiving surgical and catheterisation interventions.Reference Ramanan, Lee, Maharajh, Webster and Longmuir17 Such programs have been successful in early phases, without evidence of adverse outcomes.Reference Fernie, Wylie, Schäfer, Carnegie, Miyamoto and Jacobsen19 With more programs and provider awareness, patients can strive to not only quickly meet but also surpass their baseline activity levels, overall improving family quality of life.
Pain
While pain in the postoperative phase is a more commonly analysed experience for children with CHD, about half of families interviewed still report difficulties. Two significant barriers to addressing these needs include inadequate pain assessment scores amongst varying ages and prioritising the haemodynamic fluctuance that comes with cardiac surgery.Reference Pollak and Serraf20 While there remains much subjectivity in addressing pain, provider awareness that persistent pain can adversely affect the immune system, delay wound healing, and as discussed above, impair sleep, may allow for more preventative and aggressive treatment of pain.Reference Smith, Besunder and Betters13
The recent development of pain management guidelines for surgical CHD patients is also encouraging, as more standardised procedures and expectations may help families and providers alike when considering discharge pain regimens.Reference Gal, Clyde and Colvin10 Focused techniques for early inpatient postoperative pain, such as nerve blocks and early use of ketorolac, were utilised in the Enhanced Recovery After Surgery program, but these mechanisms do not extend to the postoperative phase at home. Balancing non-pharmacologic aspects of pain (including sleep and exercise as discussed above), as well as further insight into alternative extended pain medications aside from opiates (such as more aggressive use of non-steroidal anti-inflammatory drugs or GABA analogues), may offer improved options for pain mitigation upon returning home.
Unique concerns
Chromosomal abnormalities or comorbid syndromes are present in as many as 18% of patients with CHD.Reference van Nisselrooij, Lugthart and Clur21,Reference Yasuhara and Garg22 Several families reported unique concerns among patients with comorbid conditions, particularly those with developmental delays. Challenges included cleanliness of sternal wound, understanding of the expectation of discomfort, and further issues with impaired sleep. The occupational realities that all families with children undergoing surgery face—such as work loss in the inpatient and early outpatient times—can be exacerbated with children with complex medical disease aside from their CHD, who may have delayed return to baseline.Reference Hummel, Ludomirsky and Burgunder23 Specific focus within this population, including need for physical and/or occupational therapy to transition to home following discharge, could optimise the service that teams provide families.
Communication and feedback
Given the positive and negative experiences that highlighted the desire for readily available medical guidance, frequent and open communication between families and team members underlies the challenges families face upon return home. When asked what made recovery easy, comments addressed expectations from the care team, though there were frequent responses from families lamenting the communication of follow-up trajectory, physical therapy instructions, and contingency plans.
Two-way communication and feedback loops about what is and is not working between patients/families and care teams undergoes a dramatic shift upon discharge from inpatient to outpatient. While inpatient, there is frequent dialogue with real-time access to providers. While communication options exist following discharge, often in the form of clinic numbers or electronic health record messaging, these mechanisms are not real time, with often staggered responses. The standard of follow-up clinic visits days or weeks later creates an expectation that that is the time to discuss concerns, which may limit the opportunity to intervene early on problems or stressors. Inadequate support to families, particularly those of unique challenges—be it caring for children with complex disease or families with fewer resources—may, unsurprisingly, be at risk of higher psychological distress and lower well-being over time.Reference Jackson, Frydenberg, Liang, Higgins and Murphy24
To aid in early discharge communication, utilisation of digital tools (such as real-time two-way communication via app or text-based modules) or patient connectors (nurses or equivalent roles to follow-up actively with patients) may aid in the stress and recovery postoperatively, particularly once patients are at home. Additionally, wearable technology is beginning to be a focus of surgical or hospital recovery. The data procured from such an intervention in this patient population—both inpatient and outpatient—could inform future interventions by healthcare teams and by patients themselves by rapid feedback of their symptoms. Lastly, utilising the CHD community via online groups or representative families who can share experiences can optimise expectations for families.
Limitations
As this is a small, homogenous sample, further research is necessary to evaluate whether this information is centre specific. Most notably, while the results of early discharge barriers are informative, this is a purely intervention cohort with the findings in this paper being purely descriptive of an early iteration of the program that will help drive future states. Further work comparing Enhanced Recovery After Surgery patients to those outside of the program could elucidate both the existence and specifications of differences allotted by the implementation of Enhanced Recovery After Surgery. Ongoing work outside the scope of this descriptive paper is assessing the relationship of the Enhanced Recovery After Surgery program on clinical inpatient metrics as compared to similar patients prior to roll-out of the program. Additionally, infants were excluded, as Enhanced Recovery After Surgery is targeted primarily on ambulatory patients with a focus on returning to baseline symptomatically. This consequently excludes a large proportion of CHD surgical patients who may exhibit signs of specific struggles (i.e. feeding difficulties) due to their age more frequently. Another small but still limiting factor involves the timeline of family responses; families were called anywhere from 1 to 3 months post-procedure, and this variable, while narrow, may have contributed to perceived difficulties and overall perspectives.
Conclusion
Following discharge in the early phase of recovery from CHD surgery, patients and families continue to struggle with distinct symptoms, particularly sleep, daily activity, and pain. To optimise quality of life, care teams within heart centres can optimise services provided with uninhibited access to medical guidance and support and to alleviate stressors and allow early intervention of concerns at home. Ultimately, further research could support the development of a standardised process to address these difficulties and improve the immediate postoperative quality of life of families with CHD and other surgical conditions.
Acknowledgements
We would like to acknowledge first and foremost the families that contributed to the data of this study. We would also like to acknowledge the surgical, ICU, cardiac, and floor teams that contributed to these family’s experiences.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Competing interests
The authors declare none.
Ethical standard
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national guidelines on human experimentation (IRB 00163861) and with the Helsinki Declaration of 1975, as revised in 2008, and has been approved by the institutional committees (University of Utah IRB Committee).







