CHD is a major contributor to the global burden of childhood illness and death, with an approximate incidence of 0.8% of all live births. Half of all deaths among patients with CHD occur during the first year of life, especially in countries where access to surgery is limited. In low-income countries, limitations of human resources and facilities for cardiac surgery and postoperative management mean that, for many children, correctable congenital heart lesions are not addressed or, if they are, the perioperative period is more hazardous because of complications related to delayed surgery.
Children with CHD have increased risk and severity of infection. Impaired nutrition and pulmonary congestion predisposes to pneumonia and other lower respiratory tract infections. Furthermore, some forms of CHD are associated with genetic abnormalities or syndromes that lead to some level of immunosuppression or increased susceptibility to infection.Reference Wheeler, Jeffries, Zimmerman, Wong and Carcillo 1
This review focusses on aspects of perioperative infection in children with CHD, particularly the frequency of these infections, diagnostic issues, impact on timing of surgery and outcomes, and interventions to reduce perioperative infections.
Methods
Search strategy
A systematic search of the English-language literature was undertaken using PubMed with the following terms: ((Infect* OR “Infection”[Mesh] OR infection OR “perioperative infection” OR “preoperative infection” OR “postoperative infection” OR “intraoperative infection” OR sepsis OR septicemia OR endotoxemia) AND (cardiac OR “congenital heart disease”) AND (child* OR pediatric OR pediatrics OR paediatric OR paediatrics OR infant OR neonat*)).
All studies that evaluated the epidemiology of perioperative infections – preoperative, intraoperative, and postoperative infection – in children with CHD, the impact of infections on health outcomes, and interventions to reduce perioperative infections were identified. Studies with duplicated data were excluded.
Data extraction and outcome measures
After reading the full texts, the eligibility of all studies identified using the inclusion criteria outlined above were independently assessed. Using a standardised data-extraction form, we summarised study details including authors, year of publication, and country or countries where the study was performed; study design; population and number of subjects; outcomes and results including timing of infection (preoperative, intraoperative, and postoperative), type and definition of infections – community- or hospital-acquired infections including bloodstream infection or sepsis, pneumonia, viral infections, infective endocarditis, other and definition used for diagnostic criteria – frequency of infections – prevalence, cumulative incidence, incidence density – type of organism(s), and other – risk factors, predictors, and impact of infections.
Types of infection were grouped as follows: preoperative infections including community-acquired infections and hospital-acquired infections or nosocomial infections; intraoperative infections; and postoperative infections including nosocomial bloodstream infection or catheter-associated bloodstream infection or sepsis, ventilator-associated pneumonia, urinary tract infection or catheter-associated urinary tract infection, and surgical site infection or wound infection.
Outcomes were as follows: frequency and risk factors for perioperative infections; diagnosis of perioperative infections; impact of infection on timing of surgery; impact of infection on outcomes; and intervention(s) to reduce perioperative infections. The frequency of perioperative infections according to two standard metrics was expressed as episodes/1000 patient-days or cases/100 patients – the percentage of patients who developed a perioperative infection. Impact of infections on health outcomes was assessed based on associated mortality and morbidity.
Results
The search identified 16,172 articles, of which 62 satisfied the inclusion criteria (Fig 1). Among eligible published studies, 41 were conducted in high-income countries (Supplementary material, Table 1) and 21 in low- or middle-income countries (Supplementary material, Table 2).
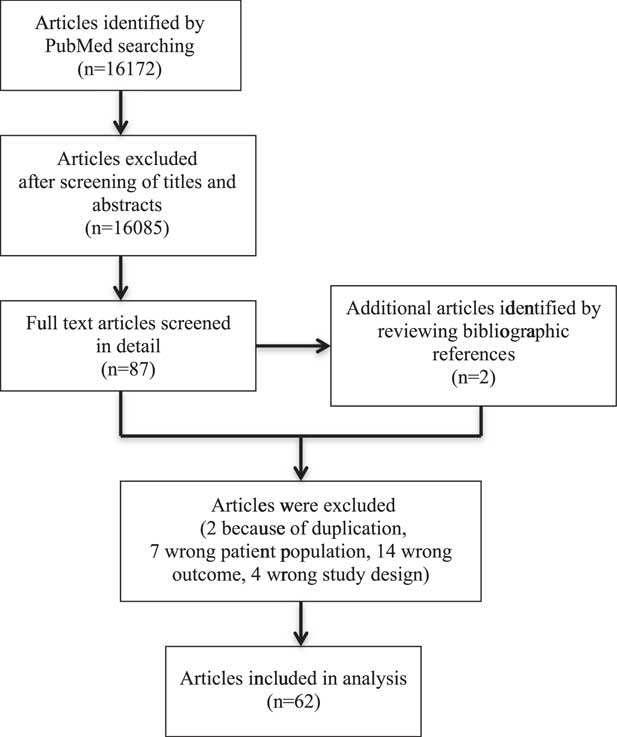
Figure 1 Search strategy for articles.
Table 1 Practical considerations in preventing, identifying, and treating perioperative infections in children with cardiac disease, focussed particularly on low- and middle-income settings.

Epidemiology of perioperative infections in high-income countries
All studies were conducted in tertiary urban or teaching hospitals. Among studies conducted in high-income settings, 15 were in European countries,Reference Algra, Driessen and Schadenberg 2 – Reference Wessel, Simon and Regensburger 16 19 in the United States of America,Reference Allpress, Rosenthal, Goodrich, Lupinetti and Zerr 17 – Reference Woodward, Son, Calhoon, Michalek and Husain 35 one in Australia,Reference Moynihan, Barlow and Alphonso 36 three elsewhere in North America,Reference Glass, Bowman and Chau 37 – Reference Rushani, Kaufman and Ionescu-Ittu 39 and three in Asia.Reference Chiu, Shao and Chen 40 – Reference Shin, Jhang, Park and Yun 42 There were three non-randomised interventional studies,Reference Izquierdo-Blasco, Campins-Marti and Soler-Palacin 6 , Reference Costello, Morrow, Graham, Potter-Bynoe, Sandora and Laussen 22 , Reference Delgado-Corcoran, Van Dorn and Pribble 23 32 cohort studies,Reference Algra, Driessen and Schadenberg 2 – Reference Granbom, Fernlund, Sunnegardh, Lundell and Naumburg 5 , Reference Jaworski, Haponiuk and Irga-Jaworska 7 – Reference Chu, Hornik, Li, Campbell and Hill 20 , Reference Gupta, Sakhuja, MsGrath and Asmar 24 , Reference Murray, Krishnamurthy and Corda 27 – Reference Pasquali, He and Jacobs 29 , Reference Sochet, Cartron and Nyhan 31 – Reference Wei, Azen, Bhombal, Hastings and Paquette 34 , Reference Moynihan, Barlow and Alphonso 36 – Reference Pollock, Ford-Jones and Rebeyka 38 , Reference Chiu, Shao and Chen 40 – Reference Shin, Jhang, Park and Yun 42 three case-control studies,Reference Costello, Graham and Morrow 21 , Reference Harder, Gaies and Yu 25 , Reference Prasad, Dominguez and Zaoutis 30 and three cross-sectional studies.Reference McNeil, Ligon and Hulten 26 , Reference Woodward, Son, Calhoon, Michalek and Husain 35 , Reference Rushani, Kaufman and Ionescu-Ittu 39 The majority of studies were conducted on children, three studies focussed specifically on neonates,Reference Ascher, Smith and Clark 18 , Reference Murray, Krishnamurthy and Corda 27 , Reference Glass, Bowman and Chau 37 and three studies involved both children and adults.Reference Forstner, Lassnigg and Tobudic 3 , Reference Fortun, Centella and Martin-Davila 4 , Reference Shin, Jhang, Park and Yun 42
Preoperative infections
There were 10 studies describing preoperative infections. These included acute respiratory tract infections – upper respiratory tract infection, bronchiolitis, pneumonia, and respiratory syncytial virus infectionsReference Granbom, Fernlund, Sunnegardh, Lundell and Naumburg 5 , Reference Medrano Lopez and Garcia-Guereta 10 , Reference Resch, Kurath-Koller, Hahn, Raith, Kostenberger and Gamillscheg 11 , Reference Chu, Hornik, Li, Campbell and Hill 20 , Reference Chiu, Shao and Chen 40 – sepsis,Reference Ascher, Smith and Clark 18 and infective endocarditis.Reference Fortun, Centella and Martin-Davila 4 , Reference Gupta, Sakhuja, MsGrath and Asmar 24 , Reference Rushani, Kaufman and Ionescu-Ittu 39 , Reference Marom, Levy, Gutwein, Birk and Ashkenazi 41
Among children with cardiac disease, the cumulative incidence of preoperative hospitalisation from respiratory syncytial virus (RSV) infection was 0.5% (2518/549,265) to 9.6% (58/602) in children <2 years of age with mortality of 1.9% of 8127 to 4.9% of 549,265 patients.Reference Granbom, Fernlund, Sunnegardh, Lundell and Naumburg 5 , Reference Resch, Kurath-Koller, Hahn, Raith, Kostenberger and Gamillscheg 11 , Reference Chu, Hornik, Li, Campbell and Hill 20 , Reference Chiu, Shao and Chen 40 Risk factors for hospital admission due to acute respiratory tract infections were malnutrition, infant, male, chromosomal abnormalities, wheezing, inadequate respiratory syncytial virus prophylaxis, and sibling <11 years of age.Reference Medrano Lopez and Garcia-Guereta 10 In children with haemodynamically significant CHD, those who underwent surgery early might be less often hospitalised compared with those who underwent surgery later.Reference Resch, Kurath-Koller, Hahn, Raith, Kostenberger and Gamillscheg 11
In the United States of America, the cumulative incidence of preoperative sepsis in children with CHD was 5.6% (656/11,638).Reference Ascher, Smith and Clark 18 The most common bacteria isolated in children with sepsis and CHDs were Gram-positive organisms (64%), including coagulase-negative Staphylococcus and Staphylococcus aureus. Reference Ascher, Smith and Clark 18 Risk factors for sepsis included young age, high complexity of cardiac surgery, history of cardiothoracic surgery, preoperative length of hospital stay >24 hours, preoperative ventilator use, genetic syndromes,Reference Barker, O’Brien and Welke 19 length of hospital stay >10 days, and cyanotic CHD.Reference Valera, Scolfaro and Cappello 15
Incidence density of preoperative infective endocarditis among children with CHD was 0.32/1000 to 6.1/1000 hospitalisations.Reference Rushani, Kaufman and Ionescu-Ittu 39 , Reference Marom, Levy, Gutwein, Birk and Ashkenazi 41 In a study involving children and adults, the cumulative incidence of infective endocarditis in CHD was as high as 5.5% (45/821).Reference Fortun, Centella and Martin-Davila 4 Community-associated pathogens in children with infective endocarditis included viridans streptococci (38%) and Staphylococcus aureus (19%), whereas healthcare-associated infective endocarditis pathogens were Candida spp (27%), coagulase-negative staphylococci (20%), and Gram-negative bacilli (16%).Reference Marom, Levy, Gutwein, Birk and Ashkenazi 41 Risk factors for preoperative infective endocarditis were cyanotic CHD, atrioventricular septal defects, left-sided lesions, and age <30 years.
Postoperative infections
Many studies have described postoperative infections in children undergoing cardiac surgery. Among those studies, the most common infection studied was surgical site infection with varied incidence of 1.2% (12/981) to 48% (22/46).Reference Algra, Driessen and Schadenberg 2 , Reference Izquierdo-Blasco, Campins-Marti and Soler-Palacin 6 , Reference Allpress, Rosenthal, Goodrich, Lupinetti and Zerr 17 , Reference Delgado-Corcoran, Van Dorn and Pribble 23 , Reference Harder, Gaies and Yu 25 – Reference Murray, Krishnamurthy and Corda 27 , Reference Sochet, Cartron and Nyhan 31 – Reference Turcotte, Brozovich and Corda 33 , Reference Woodward, Son, Calhoon, Michalek and Husain 35 , Reference Glass, Bowman and Chau 37 , Reference Pollock, Ford-Jones and Rebeyka 38 , Reference Shin, Jhang, Park and Yun 42 Risk factors for surgical site infections were duration of surgery,Reference Allpress, Rosenthal, Goodrich, Lupinetti and Zerr 17 , Reference Costello, Graham and Morrow 21 age <1 month,Reference Allpress, Rosenthal, Goodrich, Lupinetti and Zerr 17 , Reference Murray, Krishnamurthy and Corda 27 , Reference Sohn, Schwartz, Yang, Jarvis, Guglielmo and Weintrub 32 blood transfusion,Reference Costello, Graham and Morrow 21 parenteral nutrition,Reference Sohn, Schwartz, Yang, Jarvis, Guglielmo and Weintrub 32 perioperative medical device,Reference Sohn, Schwartz, Yang, Jarvis, Guglielmo and Weintrub 32 excessive bleeding within 24 hours after surgery, and incorrect timing of preoperative antibiotics.Reference Murray, Krishnamurthy and Corda 27
Postoperative bacteraemia occurred in 1.5% (15/992) to 10.2% (13/127).Reference Kansy, Jacobs and Pastuszko 8 , Reference Barker, O’Brien and Welke 19 , Reference Murray, Krishnamurthy and Corda 27 , Reference O’Brien, Marshall, Tarrants, Stroup and Lofland 28 , Reference Glass, Bowman and Chau 37 The most common isolated bacteria in infants with healthcare-associated bloodstream infections included Staphylococcus epidermidis, Escherichia coli, Enterobacter cloacae, Bacillus spp, Staphylococcus aureus, Enterococcus spp, and Klebsiella spp.Reference Glass, Bowman and Chau 37 Fungal infection or invasive candidaemia post-cardiac surgery occurred in 0.4% (6/1540) to 5.9% (10/169).Reference Forstner, Lassnigg and Tobudic 3 , Reference Jaworski, Haponiuk and Irga-Jaworska 7 , Reference Wessel, Simon and Regensburger 16 Risk factors for postoperative bloodstream infections were use of central venous catheters,Reference Murray, Krishnamurthy and Corda 27 , Reference Prasad, Dominguez and Zaoutis 30 blood transfusion, use of steroids, and antibiotic prophylaxis for more than 2 days after surgery.Reference Turcotte, Brozovich and Corda 33
Pulmonary infections
RSV infection was described in 3% of 1737 children after cardiac surgery.Reference Moynihan, Barlow and Alphonso 36 The incidence of nosocomial pneumonia in infants undergoing cardiac surgery was 6.2% (8/127)Reference Glass, Bowman and Chau 37 and incidence density of ventilator-associated pneumonia in children was 17.1/1000 patient-days.Reference Roeleveld, Guijt, Kuijper, Hazekamp, de Wilde and de Jonge 12 Haemophilus influenzae, Moraxella catarrhalis, Staphylococcus aureus, and Pseudomonas aeruginosa were the most common pathogens isolated in children with ventilator-associated pneumonia. Risk factors for ventilator-associated pneumonia were PRISM III score >10 and transfusion of fresh-frozen plasma.Reference Roeleveld, Guijt, Kuijper, Hazekamp, de Wilde and de Jonge 12
Epidemiology of perioperative infections in low- and middle-income countries
Among 21 studies in low- and middle-income countries, four were conducted in China,Reference Sheng, Xing and Hou 43 – Reference Zhang, Yuan and Li 46 four in India,Reference Bakshi, Vaidyanathan and Sundaram 47 – Reference Senthilkumar, Menon and Subramanian 50 three in Brazil,Reference de Araujo Motta, Dalla-Costa, Dominguez Muro, Lenzi, Picharski and Burger 51 – Reference Jacomo, Carmona, Matsuno, Manso and Carlotti 53 two in Saudi ArabiaReference Abou Elella, Najm, Balkhy, Bullard and Kabbani 54 , Reference Shaath, Jijeh, Faruqui, Bullard, Mehmood and Kabbani 55 , and one each in Argentina,Reference Rosanova, Allaria and Santillan 56 Bosnia Herzegovina,Reference Hadzimuratovic, Dinarevic and Hadzimuratovic 57 Iran,Reference Mirzaei, Mirzaei, Sepahvand, Koshkaki and Jahromi 58 Ethiopia,Reference Moges, Gedlu and Isaakidis 59 Guatemala,Reference Vida, Leon-Wyss, Larrazabal, Cruz and Castaneda 60 and Sudan.Reference Mohamed Ali, Berggreen and Nguyen 61 One multicentre study involving 17 low- to middle-income countries included India, Pakistan, Colombia, Russia, China, Dominican Republic, Brazil, Argentina, El Salvador, Ukraine, Peru, Mexico, Belarus, Vietnam, Uganda, Guatemala, and Bangladesh.Reference Jenkins, Castaneda and Cherian 62
There were five different study designs including one randomised controlled trial,Reference Jacomo, Carmona, Matsuno, Manso and Carlotti 53 one non-randomised interventional before–after study,Reference Jenkins, Castaneda and Cherian 62 16 cohort studies,Reference Sheng, Xing and Hou 43 – Reference Wang, Sun, Lv and Tian 45 , Reference Bakshi, Vaidyanathan and Sundaram 47 – Reference Senthilkumar, Menon and Subramanian 50 , Reference Faria, Nicolau, Melek, de Oliveira Nde, Bermudez and Nisihara 52 , Reference Abou Elella, Najm, Balkhy, Bullard and Kabbani 54 – Reference Hadzimuratovic, Dinarevic and Hadzimuratovic 57 , Reference Moges, Gedlu and Isaakidis 59 , Reference Vida, Leon-Wyss, Larrazabal, Cruz and Castaneda 60 , Reference Kabbani, Ismail and Fatima 63 one case-control study,Reference de Araujo Motta, Dalla-Costa, Dominguez Muro, Lenzi, Picharski and Burger 51 and three cross-sectional studies.Reference Zhang, Yuan and Li 46 , Reference Mirzaei, Mirzaei, Sepahvand, Koshkaki and Jahromi 58 , Reference Mohamed Ali, Berggreen and Nguyen 61 Most studies were conducted in children, with two in neonatesReference Bakshi, Vaidyanathan and Sundaram 47 , Reference Hadzimuratovic, Dinarevic and Hadzimuratovic 57 and two involving children and adult patients.Reference Sheng, Xing and Hou 43 , Reference Senthilkumar, Menon and Subramanian 50
Preoperative infection
There were seven studies evaluating preoperative infections among children with CHD in low- to middle-income country settings. In India, the incidence of preoperative infection was 33% (28/84).Reference Patwary, Khan, Marwah, Singh, Shekhawat and Sharma 48 In Brazil, the incidence of sepsis was 4.6% of 127 patientsReference Faria, Nicolau, Melek, de Oliveira Nde, Bermudez and Nisihara 52 and late sepsis was 18% (14/80) in Bosnia Herzegovina.Reference Hadzimuratovic, Dinarevic and Hadzimuratovic 57 The incidence of pneumonia before surgery was 16.5% among 127 children with CHD in Brazil.Reference Faria, Nicolau, Melek, de Oliveira Nde, Bermudez and Nisihara 52 The most common bacteria in infants with preoperative infections included Staphylococcus aureus, Klebsiella spp, and Serratia spp.
In China, the incidence of infective endocarditis related to CHD was 79% (27/34) and infective endocarditis related to rheumatic heart disease was 6% (2/34).Reference Wang, Sun, Lv and Tian 45 Bacteria was isolated from children with preoperative infective endocarditis including Staphylococcus aureus (58%), Strepcococcus viridians (8%), Enterococcus faecium (8%), other Gram-positive cocci (17%), and other Gram-negative bacilli (3%).Reference Wang, Sun, Lv and Tian 45 Among children and adults with culture-positive infective endocarditis, viridans group streptococci (56%), Staphylococcus spp (15%), Pseudomonas spp (7%), Corynebacterium diphtheriae (4%), Acinetobacter baumannii (4%), Salmonella enterica serovar Typhi (4%), and Granulicatella adiacens (4%) were isolated.Reference Senthilkumar, Menon and Subramanian 50 In Sudan, 160 children with CHD might develop rates of dental caries and gingivitis as high as 4 and 2%, respectively.Reference Mohamed Ali, Berggreen and Nguyen 61
Postoperative infection
Among studies evaluating postoperative infections, the prevalence of infection was varied ranging from 7.8% of 203 children in Iran to 40% of 300 children in China.Reference Zhang, Yuan and Li 46 , Reference Mirzaei, Mirzaei, Sepahvand, Koshkaki and Jahromi 58 Microbes isolated from children with postoperative infection were 66.6% Gram-positive and 26.7% Gram-negative bacteria, and 6.7% were fungi. The most common pathogens were Staphylococcus epidermidis, Staphylococcus aureus, Enterococcus spp, Pseudomonas aeruginosa, and Candida albicans.Reference Zhang, Yuan and Li 46 Risk factors for postoperative infections were length of hospital stay, use of combined antibiotics, use of hormone therapy, mechanical ventilation, and indwelling central venous catheter.Reference Zhang, Yuan and Li 46
The incidence of postoperative sepsis or bloodstream infection across 17 countries was 7% of 15,049 in children, and 21% (17/330) in neonates, after cardiac surgery.Reference Bakshi, Vaidyanathan and Sundaram 47 , Reference Sahu, Siddharth and Choudhury 49 , Reference Abou Elella, Najm, Balkhy, Bullard and Kabbani 54 , Reference Rosanova, Allaria and Santillan 56 , Reference Jenkins, Castaneda and Cherian 62 The most common pathogens isolated were Gram-negative bacteria in 67%, Pseudomonas aeruginosa in 28%, and Enterobacter spp in 22% of children with postoperative bloodstream infection.Reference Abou Elella, Najm, Balkhy, Bullard and Kabbani 54 Risk factors for bloodstream infections after cardiac surgery were malnutrition, high complexity of surgery, delayed sternal closure, prolonged central venous catheter use, and prolonged ICU and hospital stay.Reference Abou Elella, Najm, Balkhy, Bullard and Kabbani 54 Candidaemia occurred in 0.07% children.Reference de Araujo Motta, Dalla-Costa, Dominguez Muro, Lenzi, Picharski and Burger 51 Risk adjustment for congenital heart surgery (RACHS)-1 score ⩾3, use of acid suppression, and thrombocytopaenia were independent risk factors for candidaemia.Reference de Araujo Motta, Dalla-Costa, Dominguez Muro, Lenzi, Picharski and Burger 51
The incidence of surgical site infection was 2.5% of 350 children with CHD in Argentina to 12.7% (55/330) in India,Reference Bakshi, Vaidyanathan and Sundaram 47 , Reference Sahu, Siddharth and Choudhury 49 , Reference Rosanova, Allaria and Santillan 56 with Gram-positive cocci being the most frequent pathogens isolated.Reference Rosanova, Allaria and Santillan 56 The incidence of nosocomial pneumonia approached 21% (67/331) in China to 44% of 6864 children in IndiaReference Tan, Sun, Zhu, Zhang, Li and Shu 44 , Reference Sahu, Siddharth and Choudhury 49 , Reference Jacomo, Carmona, Matsuno, Manso and Carlotti 53 and ventilator-associated pneumonia was 6.2% (105/1688) in China to 18.3% of 160 children in Brazil.Reference Sheng, Xing and Hou 43 , Reference Jacomo, Carmona, Matsuno, Manso and Carlotti 53 , Reference Shaath, Jijeh, Faruqui, Bullard, Mehmood and Kabbani 55 The most common pathogens isolated in children with ventilator-associated pneumonia were Gram-negative bacilli, followed by Gram-positive cocci and fungi.Reference Sheng, Xing and Hou 43 , Reference Tan, Sun, Zhu, Zhang, Li and Shu 44 , Reference Shaath, Jijeh, Faruqui, Bullard, Mehmood and Kabbani 55 Risk factors for ventilator-associated pneumonia included prolonged cardiopulmonary bypass, use of parenteral nutrition, ICU length of stay,Reference Shaath, Jijeh, Faruqui, Bullard, Mehmood and Kabbani 55 mechanical ventilation, extubation failure, emergency surgery, and blood transfusion.Reference Sheng, Xing and Hou 43
Around 7% children developed catheter-associated urinary tract infections,Reference Sahu, Siddharth and Choudhury 49 , Reference Kabbani, Ismail and Fatima 63 with Gram-negative bacteria most commonly isolated. Duration of foley catheter, congenital anomalies of the kidney and urinary tract, and genetic syndromes were independent risk factors for catheter-associated urinary tract infections.Reference Kabbani, Ismail and Fatima 63
Impact of infection on timing of surgery (global)
There were no studies evaluating the impact of perioperative infections on timing of cardiac surgery. We could only find studies that evaluated the impact of timing surgery on later occurrence of infections. Early surgery was associated with less frequent hospitalisations owing to respiratory syncytial virus infections in children with haemodynamically significant CHD.Reference Resch, Kurath-Koller, Hahn, Raith, Kostenberger and Gamillscheg 11 Older postnatal age at surgery might increase preoperative infections in infants born small for gestational age compared with non-small gestational age.Reference Wei, Azen, Bhombal, Hastings and Paquette 34
Impact of infections on health outcomes (global)
Several published studies in high-income countries evaluated the impact of infection on outcomes including mortality and other morbidity or complications related to infections. Studies on preoperative and postoperative infection conducted in high-income countries revealed that those infections might be associated with increased mortality and length of hospital stay. Hospitalisation related to preoperative respiratory syncytial virus infections was associated with mortality rates of 1.9% of 549,265 in Taiwan to 4.9% of 549,265 in the United States of America.Reference Chu, Hornik, Li, Campbell and Hill 20 , Reference Chiu, Shao and Chen 40 Children with preoperative infective endocarditis related to CHD had mortality rates of 2.8% of 3840 children in the United States of America to 12% (6/51) in Israel.Reference Gupta, Sakhuja, MsGrath and Asmar 24 , Reference Marom, Levy, Gutwein, Birk and Ashkenazi 41 A study in Spain involving children and adolescents with infective endocarditis demonstrated mortality rates of 24% of 821 children with CHD.Reference Fortun, Centella and Martin-Davila 4
Children with postoperative infections had increased mortality, prolonged length of stay, and increased healthcare costs. Nosocomial infection increased healthcare costs and length of stay.Reference Pasquali, He and Jacobs 29 Postoperative viral infection was associated with prolonged paediatric ICU stay and prolonged intubation.Reference Moynihan, Barlow and Alphonso 36 Postoperative major infections including bacteraemia, mediastinitis, and endocarditis were associated with increased mortality and length of hospital stay.Reference Kansy, Jacobs and Pastuszko 8 In a study conducted in Korea, sternal wound infections were associated with mortality rates as high as 18.2% (28/154).Reference Shin, Jhang, Park and Yun 42 The adverse impact of surgical site infection on length of stay, prolonged mechanical ventilation, and need for vasoactive agents were also demonstrated.Reference Sochet, Cartron and Nyhan 31
In low- to middle-income countries, studies evaluating the impact of perioperative infections on health outcomes are limited. Preoperative infection in children with CHD may be associated with a fourfold increase in mortality.Reference Patwary, Khan, Marwah, Singh, Shekhawat and Sharma 48 Ventilator-associated pneumonia was associated with mortality rates of 11% of 137 children in Saudi Arabia to 25.7% (27/105) in China.Reference Sheng, Xing and Hou 43 , Reference Shaath, Jijeh, Faruqui, Bullard, Mehmood and Kabbani 55 A multicentre study conducted in 17 low- to middle-income countries demonstrated an association between postoperative major infection and mortality of 6.3% of 15,049 children.Reference Jenkins, Castaneda and Cherian 62
Interventions to reduce perioperative infection and their effectiveness (global)
There were three intervention studies conducted in high-income countries to reduce postoperative infections including catheter-associated bloodstream infection and surgical site infection. A quality improvement study using interrupted time series design implemented a multifaceted intervention to reduce catheter-associated bloodstream infection. These included a central line-associated bloodstream infection prevention initiative including establishment of a unit-based infection control, nurse position, education, real-time feedback on central line-associated bloodstream infection data, implementation of central venous line bundles, and introduction of daily goal sheets on rounds. After implementing these measures, central line-associated bloodstream infection rates significantly decreased from 7.8 infections per 1000 catheter-days to 2.3 infections per 1000 catheter-days.Reference Costello, Morrow, Graham, Potter-Bynoe, Sandora and Laussen 22 A before-and-after study implemented an interdisciplinary infection control programme including preoperative, intraoperative, and postoperative measures to reduce surgical site infection. After implementing the intervention, the incidence of surgical site infection decreased significantly from 10.9% (95% confidence interval (CI) 4.7–18.8) to 1.92% (95% CI 0.4–5.52) in the pre- and post-intervention period, respectively.Reference Izquierdo-Blasco, Campins-Marti and Soler-Palacin 6 Another before-and-after study implemented measures to reduce surgical site infection using chlorhexidine in the operative and postoperative periods, standardised intravenous antibiotic within 5–60 minutes of the initial surgical incision, with initiation of cardiopulmonary bypass, and every 3 hours in the intraoperative period, antibiotics for 48 hours, and dressing removal at 48 hours in the postoperative period. These measures were associated with a reduction of sternal wound infection rates from 3.8 to 2.1%.Reference Delgado-Corcoran, Van Dorn and Pribble 23
There were two intervention studies conducted in low-to middle-income countries. The first study was a randomised controlled trial aimed to reduce the risk of ventilator-associated pneumonia. The patients were randomised to receive oral hygiene with 0.12% chlorhexidine gluconate or placebo preoperatively and twice a day postoperatively until paediatric ICU discharge or death. After implementing the intervention, the incidence of nosocomial pneumonia was 29.8 versus 24.6% (p=0.46) and the incidence of ventilator-associated pneumonia was 18.3 versus 15% (p=0.57) in the chlorhexidine and the control group, respectively.Reference Jacomo, Carmona, Matsuno, Manso and Carlotti 53
Another study conducted in 17 low- to middle-income countries used a before-and-after study design. An intervention was implemented using webinars that targeted three key drivers: safe perioperative practices, infection reduction, and team-based practice and audited registry data. After implementing the intervention, the risk-adjusted in-hospital mortality was significantly lower in both 2011 (standardised mortality ratio 0.71, 95% CI 0.62–0.81) and 2012 (standardised mortality ratio 0.76, 95% CI 0.69–0.83) relative to 2010.Reference Jenkins, Castaneda and Cherian 62
Discussion of perioperative infections in low- and middle-income countries
The limited studies of children with CHD in low- and middle-income countries demonstrate that perioperative infections are common. Many risk factors exist for infection in children with CHD and some children have multiple risk factors that may accrue if there is delayed presentation, inadequate treatment, or poor nutrition.
Poor nutrition is associated with adverse outcomes in children undergoing cardiac surgery, including infection.Reference Mitting, Marino, Macrae, Shastri, Meyer and Pathan 64 There is a complex interaction between heart disease, malnutrition, immunity and infection, and adverse outcomes or complications. During starvation, cardiac myocytes may atrophy. Children suffering from severe malnutrition may exhibit cardiovascular abnormalities including hypotension, cardiac arrhythmias, cardiomyopathy, or cardiac failure.Reference Ocal, Unal, Zorlu, Tezic and Oguz 65 Malnutrition impairs many aspects of immune function, including mucosal barrier function, microbiocidal activity of granulocytes, reduced T-cell function, and reduced complement activity.Reference Rytter, Kolte, Briend, Friis and Christensen 66 Micronutrient deficiencies have a myriad of effects on immunity and cardiac function: severe iron deficiency anaemia can lead to high-output cardiac failure or reduced left ventricular contractility; thiamine deficiency causes vasodilatation and high-output cardiac failure; and selenium deficiency weakens myocyte function. Electrolyte imbalances are more common in children with severe malnutrition and cardiac disease and have many effects on the heart. Severe hypophosphataemia, for example, weakens heart muscle and reduces stroke volume, and hypomagnesaemia increases the risk of arrhythmias. Pulmonary congestion increases susceptibility to pneumonia and other lower respiratory tract infections in children with left to right shunts, which in turn increases exposure to antibiotics and increases the likelihood of antibiotic-resistant bacterial colonisation. This puts the child at an increased risk of serious invasive bacterial sepsis during and after surgery. Several gene polymorphisms associated with CHD have been linked with an increased susceptibility to sepsis, and several malformation syndromes or chromosomal syndromes, including DiGeorge syndrome and CHARGE syndrome, link CHD with immunodeficiency. Chronic hypoxia associated with cyanotic CHD may affect immune responses. Children with CHD frequently are exposed to invasive devices, which increase the risk of nosocomial infection. Ischaemia–reperfusion injury following cardiopulmonary bypass frequently results in a state of reduced functional immune response, which also increases the risk of nosocomial infections.Reference Wheeler, Jeffries, Zimmerman, Wong and Carcillo 1
The impact of these diverse risk factors on perioperative mortality and morbidity in CHD in developing countries is uncertain, but they need to be taken into account in surgical planning. Children with CHD need an individualised risk assessment while awaiting surgery, and this involves an assessment of infection risk, nutritional intake, growth and micronutrients, and adequacy of control of cardiac failure.
Bacterial infection epidemiology
While Gram-positive infections were still the most common cause of postoperative sepsis in high-income countries, Gram-negative sepsis was prevalent in children with postoperative bloodstream infections in low- to middle-income countries. Gram-negative sepsis is associated with significant morbidity, higher mortality, and development of antibiotic resistance.
About one-third of children with CHD developed preoperative infection in low- to middle-income countries. We could find no study evaluating the impact of perioperative infections on timing of surgery in low- or middle-income settings, although early surgery was associated with less frequent hospitalisations owing to acute infections in children with haemodynamically significant CHD. Whether the risk of cardiac surgery in children with preoperative infections can be mitigated in any way if surgery has to proceed is still uncertain.
Implications for patient care and further research
Formulating effective screening and prevention strategies to reduce infections is important. This requires early detection of perioperative infections, prompt management, adequate postoperative care, and early nutritional support. There is considerable scope for further research, in particular focussing on the influence of infection on the timing of surgery, as well as specific infections, which have received insufficient attention in this patient population, including preoperative Gram-negative bacteraemia, human immunodeficiency virus, and tuberculosis.
We propose 12 practical rules to reduce perioperative infections among those children in low- and middle-income countries (Table 1).
Acknowledgements
None.
Financial Support
This review received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of Interest
None.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1047951117002578




