The current COVID-19 (coronavirus disease 2019) pandemic has not only caused a massive upheaval in how we practice paediatric cardiology but also prompted us to reflect with a wider global collaborative lens to how we provide education and training in congenital cardiology. Reference McMahon, Tretter and Redington1 Reflecting on the progress of paediatric cardiology in Europe, it is clear that the speciality originally developed organically, in response to the needs of patients with CHD, rather than in a strategic planned fashion. It is also worth bearing in mind that we are a relatively new speciality, one in which many European cardiologists had to train themselves, fight for speciality recognition, and struggle to secure resources to build the speciality to high standards both in terms of patient care and outcomes. Although enormous strides have been secured in the quality of patient care, now is a pivotal time for us to evaluate where European training stands and determine what is a reasonable uniform standard or set of standards against which we can benchmark training across Europe. This should encourage quality, make equivalence more apparent, and encourage trainees to spend time training in European countries other than their own. It may also help stem the current exodus of excellent trainees and consultants to the United States and Canada. Reference Crossland, Ferguson and Magee2
Paediatric cardiology training requirements in North America are relatively standardised under the umbrella of the Accreditation Council for Graduate Medical Education (acgme.org) with several guidelines endorsed by the American Heart Association, American College of Cardiology, and American Academy of Pediatrics. 3–Reference Stout, Valente and Bartz8 Juxtaposed with this, there are multiple different pathways to training in paediatric cardiology in Europe. Several useful position papers have been published for general paediatric cardiology and specialist training from the Association for European Paediatric and Congenital Cardiology working groups including the recently published recommendations on training and completion of a logbook for trainees. Reference Heying, Albert and Voges9–Reference Reinhardt, Hansmann and O’Sullivan15 In the United States, there is a well-established Board Certification examination, and although some European countries have their own exit examination, efforts are underway towards harmonisation in Europe. Educational experts vary in their opinion of the validity of an “exit examination” in guaranteeing the quality of an accredited trainee but it might be a useful surrogate where other assessment tools are limited.
The number of patients transitioning from paediatric to adult congenital services is increasing each year. Reference Moons, Bratt and De Backer16 In several countries, adult CHD has now evolved as its own distinct speciality from paediatric cardiology. The manpower shortage to care for these patients however remains a major challenge. Reference Moons, Bratt and De Backer16
We hypothesised that the organic evolution of paediatric cardiology and adult CHD is also reflected in fellow training structures, manifested by a significant disparity in training between European countries ranging from formally organised accredited cardiology fellowship (± exit examination), informal but substantial cardiology training (typically without exit examination), to no training. This study aimed to clarify the current status of training of European paediatric, and adult CHD cardiologists determine whether exit examinations are undertaken and what certification is provided in such countries. The ultimate goal is to drive standardisation and provision of high-quality training with the long-term goal of ensuring equitable provision of high-quality paediatric cardiology and adult CHD healthcare across all European countries.
Methods and materials
In December 2020, a structured approved questionnaire was designed to ascertain the structures and level of training for all paediatric cardiologists in European training centres. After several iterations, approved and sanctioned by two independent paediatric cardiologists and the Association for European Paediatric and Congenital Cardiology council, a questionnaire was finalised.
The national delegate for each respective country registered with the Association for European Paediatric and Congenital Cardiology was invited by e-mail to participate in the study. A second and third e-mail invitation was sent to the national delegate over a 6-week period failing a response to the initial invitation. Failing those invitations we attempted to make telephone contact with the delegate to encourage participation. Failing that we contacted the national training lead if we could not reach the national delegate. Failing to respond to those measures, the delegate or lead was deemed uncontactable.
The questionnaire was circulated to the national delegate for each European country (Appendix 1). The questionnaire detailed the number of training programmes, number of general congenital cardiology fellows (or trainees), trainee characteristics, curriculum, rotations, entry criteria, exit criteria, qualifications, and advanced subspecialist training (electrophysiology, advanced imaging, cardiac catheterisation etc.). Open-ended questions searched for strengths and weaknesses of the programme.
A group of European adult CHD cardiologists were surveyed by a senior member of the Association for European Paediatric and Congenital Cardiology adult CHD working group to ascertain training entry, training streams and presence of examination and certification within the adult CHD field.
Definitions
“Formal accredited training” was defined as a nationally recognised (accredited) structured training programme in a country where the Ministry of Health recognises the subspeciality of paediatric cardiology. The training programme is of sufficient standard to complete basic paediatric cardiology training to function independently as a paediatric cardiologist.
“Informal but substantive training” was defined as being of sufficient standard to complete basic paediatric cardiology training to function independently as a consultant paediatric cardiologist. However, the training is either not formally recognised (accredited) or the Ministry of Health in that country does not (or refuses to) recognise paediatric cardiology as a distinct subspeciality of medicine.
“Paediatric cardiologist” was defined as a doctor who fully completed paediatric cardiology training (± completed a certifying cardiology examination), was appointed to a public hospital or clinic and actively delivered care as a specialist to children and/or adolescents with congenital heart disease. This does not include trainees who have merely completed their fellowship training. We did not use the term “consultant” only because it was not recognised in some countries, for example Italy and Germany.
“Competency-based medical education” encapsulates education which focuses on fulfilling critical competencies the trainee must acquire to meet the healthcare needs of their patients (e.g. the Canadian Medical Education Directive for Specialists (CanMEDS) roles of medical expert, communicator, collaborator, leader, health advocate, scholar, and professional) (Fig 1).

Figure 1. Competency-based medical education. A paediatric cardiology fellow undergoes end of year assessment by two trainers at an OSCE echocardiography station. Entrustable professional activities are increasingly been used to bridge competencies and clinical practice with trainees assessed on their capability (entrustment scale).
“Education” relates to gaining theoretical knowledge relevant to a specific field. “Training” relates to the action of learning practical skills, acquiring knowledge and experience.
“Gross Domestic Product” is the total value of all goods and services that are produced within a country’s borders during a specific time (2020 in this paper).
Statistics
Data were expressed as median and range. Population data were expressed against number of paediatric cardiologists, and gross domestic product was correlated with paediatric cardiologist numbers. The coefficient of determination (R2) was calculated for the regression of paediatric cardiologist numbers on gross domestic product. Ethical approval was received from Children’s Health Ireland at Crumlin, Dublin, Ireland for the study.
Results
Thirty national delegates registered with the Association for European Paediatric and Congenital Cardiology out of 33 (91%) responded to the invitation. Delegates reported that twenty countries (67%) have well-defined formally recognised paediatric cardiology fellowship programmes (20 certified), seven (23%) have substantial informal (not registered/certified) training, and three (10%) have limited or no programme (Table 1). Two national delegates (7%) reported that their country had no paediatric cardiology training (Cyprus and Iceland) (Fig 2). Some delegates initially reported their country offered no training but when they described what was provided, they did provide informal training, admittedly neither officially recognised nor certified. The delegate from Greece reported that there is “no formal training or fellowship but some hospitals provide training which is neither accredited nor a tested educational programme.”
Table 1. Characterisation of paediatric cardiology training among 30 AEPC countries.
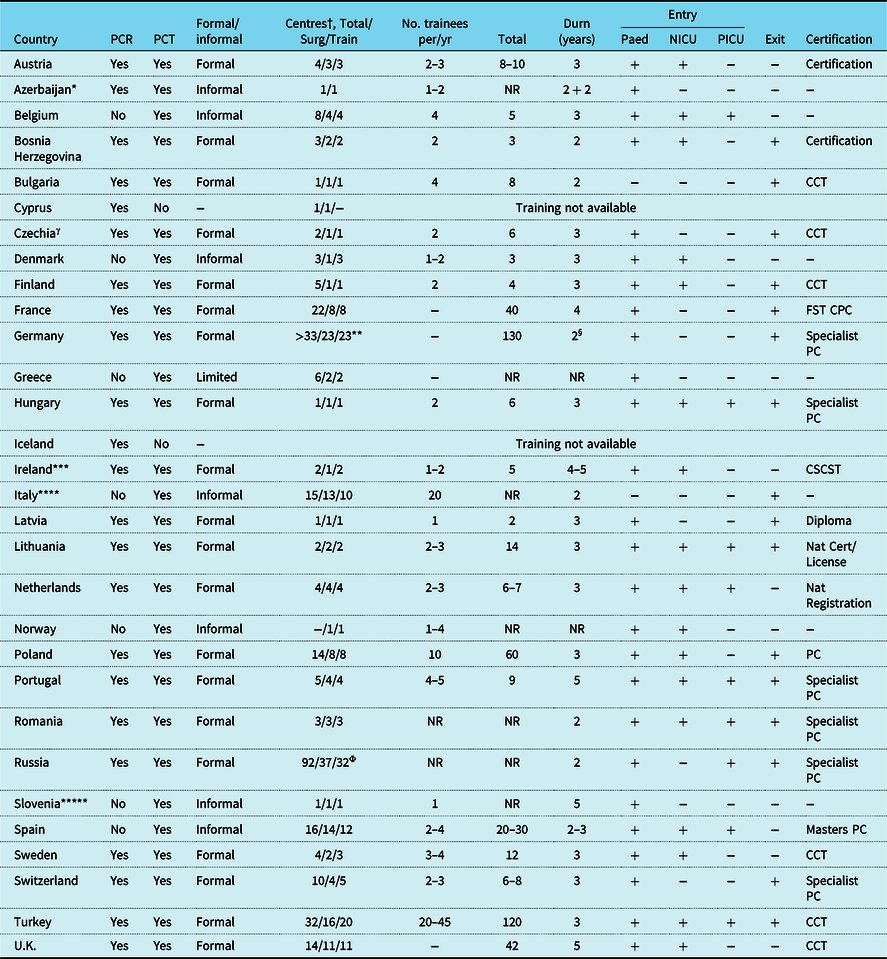
Cert, certificate; CCT, certificate of completion training; CSCST, Certificate satisfactory completion specialist training; Durn, duration of training (years); FST CPC, Formation Specialisee Transversale de Cardiologie Pediatrique et Congenitale; NICU, neonatal intensive care; Nat, national; NR, not recorded; Paed, paediatrics; PC, paediatric cardiology; PCR, Paediatric cardiology recognised subspeciality; PCT, paediatric cardiology training; PICU, paediatric intensive care; F/I, Formal or informal organisation of training
† Centres: Total paediatric cardiology centres in country (excluding private practice departments)/ Surgical centres/Training centres
* Azerbaijan trainees spend 2½ years training at home and then 2½ training in Turkey
** Full training
*** Ireland has a shared All Island CHD Network with training shared between Dublin (surgical centre) and Belfast
**** Italy a mix of formal and informal training with most centres providing informal training
***** In Slovenia there is no official training programme but trainees informally train in paediatric cardiology and spend time abroad (UK, Germany, Czech Republic)
Φ 92 is total number of paediatric cardiology/cardiothoracic surgical centres (joint adult-paediatric surgical centres) 37 of which perform complex neonatal congenital cardiac surgery (Bockeria LA. et al. Cardiovascular Surgery 2019. Moscow, A.N. Bakulev National Research Center of Cardiovascular Surgery, 2020.ISBN 978-5-7982-0420-5)
§ Duration training 2 years, reduced from 3 years since 2020
γ Czechia or Czech Republic
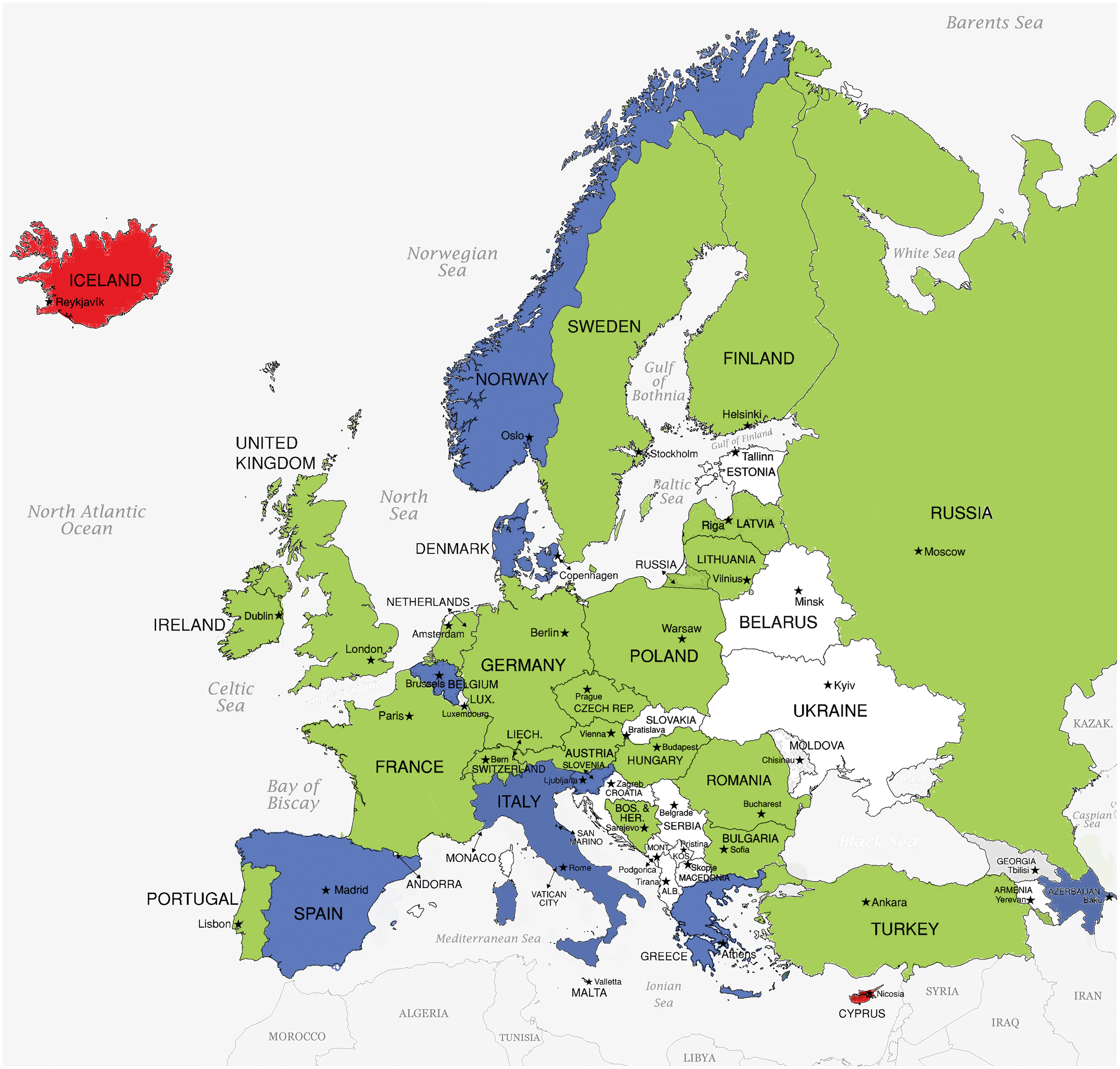
Figure 2. Paediatric cardiology training programme status across AEPC countries. Green represents a country with a formally recognised paediatric cardiology training programme. Blue represents a country with informally recognised paediatric cardiology training programme or partial training with a partner country. Red represents a country with no paediatric cardiology training programme. White represents a country which did not participate in the study.
Recognition of paediatric cardiology and consultant numbers
In seven countries (23%), paediatric cardiology is not recognised as a distinct speciality by the respective Ministry of Health (Spain, Italy, Norway, Denmark, Belgium, Slovenia, and Greece) (Fig 3). Belgium is in the process of application for speciality recognition. There was one paediatric cardiology centre per 2.66 million population (range 0.87–9.64 million), one cardiac surgical centre per 4.73 million population (range 1.63–10.72 million), and one training centre per 4.29 million population (range 1.63–10.72 million population). The median number of paediatric cardiologists per country was 47 (range 3–1139). The median number of paediatric cardiologists was 4.2 per million population (range 0.9–11.8 cardiologists per million population) (Table 2 and Fig 4).

Figure 3. Paediatric cardiology subspeciality recognition by governments across AEPC countries. Green represents countries whose Ministry of Health recognise paediatric cardiology as a distinct subspeciality. Red represents countries whose Ministry of Health do not recognise paediatric cardiology. White represents a country which did not participate in the study.
Table 2. Paediatric cardiologists per million population and GDP in 30 countries.
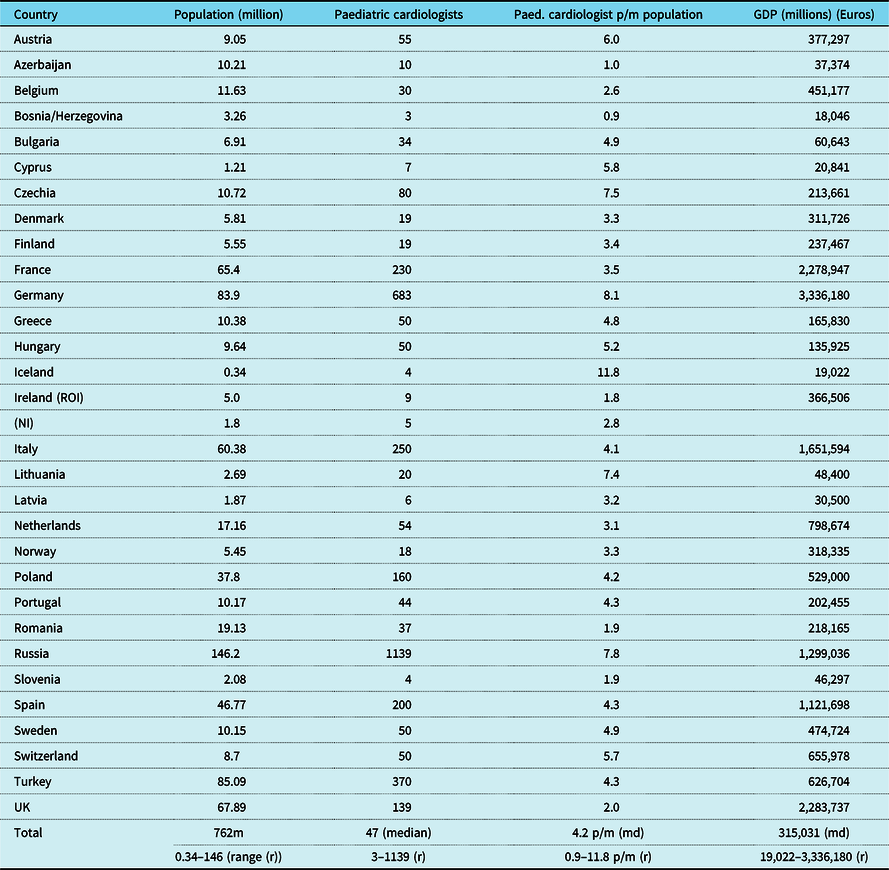
Czechia, Czech Republic; GDP, gross domestic product (2020 statistica.com); (m) in millions; (md) median; NI, Northern Ireland; No., number; p/m, per million; Paed., Paediatric; (r) range; ROI, Republic of Ireland; Rp, Republic; UK, United Kingdom
Data collated at October 2021

Figure 4. Relationship of total number of paediatric cardiologists and gross domestic product.
Origin of trainees
In each training country, the majority of trainees are citizens of that country of origin. Eight countries took trainees from one or more other European countries. Eight countries reported taking trainees from around the world. Eight countries also reported hosting fellows from low and middle-income countries for training, six of which have formal accredited training programmes (Austria, France, Germany, Netherlands, United Kingdom, and Sweden).
Paediatric cardiology training programmes in Europe
There was a wide variation in the structure and duration of training programmes between the different countries (Table 1). The median duration of training was 3 years (range from 2–5 years). The median core training was 2 years with 1-year advanced training. Although all programmes offered general cardiology training, advanced subspecialist training in imaging, electrophysiology, catheterisation, heart failure/transplantation, and pulmonary hypertension were typically limited to larger countries. Within individual countries, there was a wide variation in the number of training programmes (median of 3 with a range 0–32).
Entry level and entry mode is usually competitive and interviewed nationally or regionally. There appears to be a broad level of experience required before commencing paediatric cardiology training in the majority of countries. Thirty delegates provided a breakdown of entry criteria to training including general paediatric training (n = 26), neonatal intensive care (n = 18), or paediatric intensive care training (n = 11). Only eight countries matched training posts with the need for consultant paediatric cardiologists at the end of training period. Some countries reported dual entry possibilities from paediatrics or from adult core training to paediatric cardiology as well as adult CHD training.
Curriculum
Of the 30 countries, 22 reported having a specifically designed curriculum, which was a written document in each country. The competencies or capabilities expected to be reached by the trainees are delineated in 20 of these documents. A curriculum committee is established in 18 of the countries. The majority of the curricula have been established or re-evaluated in the last 10 years. The oldest reported was from 20 years ago, which had undergone revisions. Only five countries reported specifically using a competency framework, identified as the General Medical Council framework in four of the countries. Only four countries reported use of competency-based medical education with graded levels of entrustment as a theoretical framework in training.
Structure of training
The supervisory governance structure varied markedly between different countries. In 12 countries, there was both a national and local training director, and in 8 countries, there was a local fellowship director. There was a specific design to training with increasing complexity of training throughout fellowship in 14 countries. Sixteen countries reported provision of an annual schedule of rotations to their respective fellows.
Educational governance
Trainers involved in constructing the curriculum and delivery of educational training varied significantly between countries. In 11 countries, some trainers had undertaken formal qualifications in medical education (Masters in Medical Education in 6 countries). In 11 countries, trainers were involved in medical education research, and in 12 countries, faculty were attending medical educational research meetings (either abroad or in their home country). In 13 countries, trainees were assigned a trainer, and 6 countries assigned a “buddy” trainee to support the junior trainee. Three countries reported establishing a committee to deal with the struggling trainee, delivered through the educational supervisors, the respective Deanery or the College of Cardiology who visited the centre with input from trainees during that visit. The "annual review of competence progression" in one country provided an opportunity to assess the struggling trainee and provide supportive solutions.
Breakdown of training exposure
Twenty-seven delegates provided a complete breakdown of pre-certification guaranteed training exposure (Table 3). These included outpatient care (n = 27, 100%), inpatient care (n = 27, 100%), ICU (n = 25, 93%), echocardiography (n = 26, 96%), cardiac catheterisation (n = 24, 89%), electrophysiology (n = 20, 74%), heart failure/transplantation/pulmonary hypertension (n = 15, 56%), MRI/CT (n = 19, 70%), preventive cardiology (n = 14, 52%), adult CHD (n = 16, 59%), and cardiac morphology (n = 11, 40%). Two additional countries required trainees to attend an international morphology course (not provided by their own centre). Other specific training mentioned by delegates included foetal echocardiography (n = 2), genetics (n = 1), ethics (n = 1), and device therapy (n = 1).
Table 3. Characterisation of paediatric cardiology training available in centres in 27/30 AEPC countries.

ACHD, adult congenital heart disease; Ad, advanced; Cath, cardiac catheterisation; CT, computed tomography; EP, electrophysiology; HF, heart failure/transplantation/pulmonary hypertension; ICU, intensive care unit; MRI, magnetic resonance imaging; Prev, preventive cardiology
* Advanced training of trainees from Azerbaijan undertaken in Turkey and Russia
** Offered in the newly developed Russian 3-year programme to be approved
*** ACHD in Switzerland is trained in the adult department in adult hospitals with another curriculum and requirements than paediatric cardiology. There is a close collaboration, but regular training for a paediatric cardiologist interested in ACHD is normally only undertaken after completion of the training as a paediatric cardiologist. Addition to Swiss training: 6 months (of the 3 years required) can be completed in either adult cardiology or cardiology research
# Varies from centre to centre. Practical training in specific areas may require movement to another centre in the country (e.g. for electrophysiology training). Obligatory to have 1-month training in an adult cardiology unit
Logbook record of training
Eighteen countries reported use of a paper logbook to document trainee procedures including echocardiograms and catheterisations performed. Nine countries had an electronic logbook. Ten countries reported use of a programmatic assessment (defined as multiple different assessment tools at multiple different time points over the course of training) approach in evaluating trainees. Regular reviews of trainee performance with feedback were reported in 10 countries. Over 23 countries welcomed the introduction of an electronic logbook being developed by the Association for European Paediatric and Congenital Cardiology.
Exit examination
Sixteen countries (53%) provided an exit examination (Table 1). This varied considerably including a written examination in one country, an oral examination in 2 countries, combined oral/written examination in 3 countries, and in the remaining 10 countries a combination of written, oral, objective structured clinical examination, and long case examinations. Although several countries did not provide an exit examination, some did provide very detailed regular assessments in lieu of this including work-based assessments, multisource feedback, multiple consultant reviews in addition to an “annual review of competence progression” (e.g. United Kingdom). The United Kingdom training programme also recommends trainees achieve a score of >50% in a (formative) “Knowledge-Based Assessment” (available nationally to attempt annually) by the end of core (3 years) training and prior to embarking on higher (2 years) subspecialist training. Completion of the final “annual review of competence progression” after the indicative 5 years of training (i.e. 2 years of subspecialisation while continuing general training) is then passed to the General Medical Council for final approval and registration of Certificate of Completion of Training. So it could be viewed that thUnited Kingdom “Knowledge-Based Assessment” is an “exit exam” in all but name, to mark attainment of core training knowledge.
Certification
Twenty delegates (67%) reported their countries provide trainees with formal certification in paediatric cardiology after completion of training. In seven cases, this comprised a Certificate of Completion of Training (CCT) or Certificate of Satisfactory Completion of Specialist Training (CSCST). In other centres, a national certificate, for example Formation Specialisee Transversale de Cardiologie Pediatrique et Congenitale in France, Specialisation in Paediatric Cardiology, was provided by the Swiss ministry, Diploma of Paediatric Cardiology in Poland, or a National Formal Certificate (paediatrics and paediatric cardiology) in Lithuania.
Advanced subspecialist training
Advanced training is defined as a dedicated subspecialist period of training in, for example advanced imaging, electrophysiology, cardiac catheterisation or heart failure/transplantation. This is equivalent to the fourth year of training in North America. Many delegates reported their countries had inadequate resources for advanced subspecialist training resulting in their trainees going to larger European (n = 25), Canadian (n = 12), or U.S. centres (n = 15) to complete advanced training. Some countries have formal/informal partnerships with United States/Canadian centres (Dublin has a recent partnership with Texas Children’s Hospital and Oslo has informal relationship with Toronto Hospital for Sick Children (SickKids)). Other trainees organise their own fellowship training in North American, Canadian, or other centres. Some trainees have also moved to the United Kingdom and entered the full United Kingdom Paediatric Cardiology training programme, but to date this has been a longer route. Some delegates reported notable exceptions, for example Poland has a 3-year grant to train several paediatric cardiac interventionalists including use of virtual teaching in a simulation laboratory.
Distinct training schemes and flexibilities
Some national delegates description of their training did not fit easily into any one specific characterisation. In some countries, there is more than one route to train in paediatric cardiology; for example, in Italy one can train in paediatric cardiology via two different streams having received prior training in general paediatrics or in adult cardiology. This is also true for adult CHD; for example, in the United Kingdom, adult CHD training can be delivered either from “paediatric cardiology” or from adult cardiology training programmes. United Kingdom “paediatric cardiology” also has dual entry possible from either paediatric or adult medicine.
Azerbaijan
“Paediatric Cardiology has been recognised as a distinct specialty since 2019. There is a 5-year training programme including paediatric cardiology and neonatology during which trainees rotate through public and private hospitals. Although there is limited training in foetal cardiology and cardiac ICU, trainees move to Turkey and Russia for additional training sometimes as much as 50% of their training. After completion of training, there is no exit examination but trainees receive recognition from Ministry of Health and are eligible to become members of the Azerbaijani Cardiology Association, which is recognised by the European Society of Cardiology.”
Bulgaria
“In Bulgaria, there are 2 different streams to training in paediatric cardiology. The first stream is as a second specialty (2 years) after completion of general paediatrics training (4 years). The second stream is to complete specialised paediatric cardiology training (2 years) after a shorter duration of general paediatric training (2 years).”
Denmark
It was reported that even though paediatric cardiology (like other paediatric subspecialities) has a training programme defined and recognised by the Danish paediatric and cardiology society, paediatric cardiology is not recognised as a subspeciality by the ministry of Health in Denmark. After 4 years of general paediatric training or 5 years of cardiology training, there is a well-defined 3-year training programme (Table 3) but neither an exit examination nor formal certification other than from the two Danish societies.
France
Paediatric and Congenital Cardiology has been recently recognised as a specific specialty. There are separate 5-year programmes for training in Paediatrics and in Cardiology, both including a 1-year training period for Paediatric and Congenital Cardiology for future paediatricians and adult cardiologists. This 1 year of training is then further completed by a 2 years fellowship training in medical-surgical high-volume centres where it is possible to learn all congenital skills. There is an e-learning programme for Paediatric Cardiology and Adult Congenital Cardiology dedicated for trainees.
Greece
It was reported that there is no formal training. There is very limited informal training. “Most are trained as general paediatricians via the certified national training programme and then either go abroad and follow the training of the country they selected (some for 1, 3, or 6 months and others for 3 years or more) or stay in Greece and get informal training which is not consistent with a pre-certified or tested educational programme. In April 2021, the national society of Paediatric Cardiology have proposed a training plan including certified training centres, strict training time frame, log book, and exit examination which hopefully will soon be implemented.”
Ireland
An All Island Congenital Heart Network programme has been established with training shared across the island between the Republic of Ireland and Northern Ireland. Trainees spend most of their training in the surgical centre in Dublin but also have the opportunity to rotate through the Belfast programme.
Italy
It has been reported that “there are several centres with paediatric cardiology and adult congenital cardiology where it is possible to learn congenital skills. There are few cardiology postgraduate schools with a training specific programme in congenital cardiology.” Italy does not recognise paediatric cardiology as a subspeciality. There are separate paediatric (5-year programme) and cardiology (4-year programme) training streams. Paediatrics is a 5-year programme the first 3 years of which are general paediatric and the last 2 years paediatric cardiology training. Other centres train in cardiology offering paediatric cardiology as part of the training programme. There is an exit examination and Diploma of Specialization. Most trainees complete PhD or Masters after this certification. Many consultant paediatric cardiologists are only recognised as paediatricians in Italy.
Norway
“There is no formal structure and paediatric cardiology is not recognised as a subspecialty … All paediatricians working in the field of congenital cardiology are encouraged to spend at least 3 months in the surgical centre. A 1-year clinical paediatric cardiology and hands-on echo course is held at the surgical centre covering the core curriculum in 10 days of active teaching and training. Many of the cardiologists working in Oslo have spent 1 year abroad for subspecialty fellowships mostly at SickKids in Toronto.”
Poland
It was reported that paediatric cardiology training consists of two possible streams. The first stream is 3 years of general paediatrics and neonatology followed by 3 years of cardiology. After the first 3 years of general paediatric training, the fellow does not become a specialist in paediatrics. The second stream of training occurs after 5 years of paediatric training and comprises 3 years of paediatric cardiology.
Slovenia
“Paediatric cardiology is not officially recognised as a subspeciality by the Ministry of Health and the Slovenian Medical Chamber. Paediatricians, working in the field of paediatric cardiology receive their training at Department of Paediatric Cardiology at University Children’s Hospital Ljubljana. Training is personally tailored for each candidate according to published international guidelines. Each trainee is encouraged to spend a part of her/his training abroad in a recognised paediatric cardiology centre. Training is not formal, there is no exam at the end of training period. A young paediatrician who decides to work in the field of paediatric cardiology is considered to be in training for approximately 5 years.”
Spain
It was reported there was “no official paediatric cardiology training. There is a Master degree in paediatric cardiology in conjunction with universities, after completion of general paediatrics training and more recently a specific Masters for adult congenital cardiology in hospitals with experience in adolescents and adult with CHD. After finishing the training as a paediatrician, you can gain access to different universities hospitals to complete the training. For adult congenital cardiology access, you gain access after completing the adult cardiology training.”
Cardiovascular research during paediatric cardiology training
Of sixteen delegates who responded to the research part of the questionnaire, only five (31%) reported a research component to training (Table 4). Only three of the five delegates reported a dedicated formal time for research (median of 3 months). The majority of delegates (69%) reported either no dedicated time or informal time dedicated to research. Research requirements of training programmes are outlined in Table 4.
Table 4. Cardiovascular research during paediatric cardiology training among 16 AEPC countries.
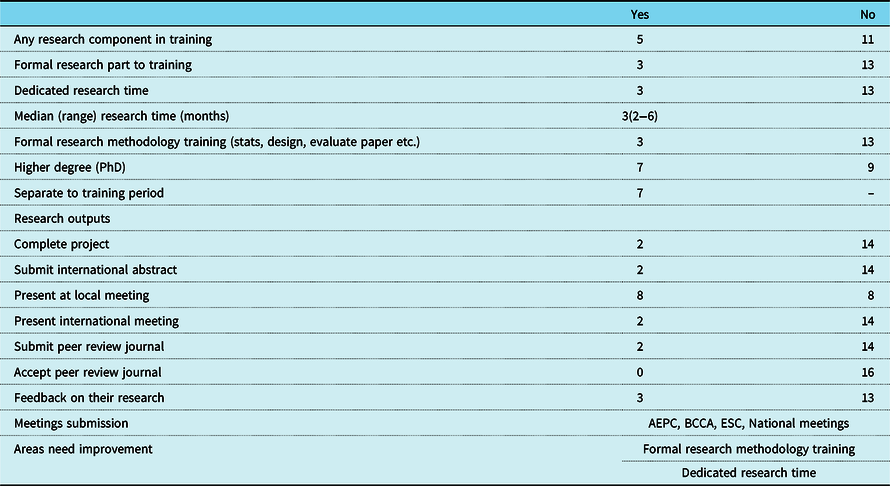
AEPC, Association for European Paediatric and Congenital Cardiology meeting; BCCA, British Congenital Cardiac Association; ESC, European Society Cardiology
Paediatric cardiology trainee travel to other countries
Of sixteen delegates who responded, fourteen (88%) reported their trainees travel abroad for further training. The countries trainees travel to and indications for travel are outlined in Table 5. Fifteen delegates reported either an informal (Oslo with Toronto SickKids) or no relationship with international centres. One delegate reported a recent partnership with Texas Children’s Hospital, Houston, Texas.
Table 5. Foreign travel for training by paediatric cardiology trainees from 16 AEPC countries.
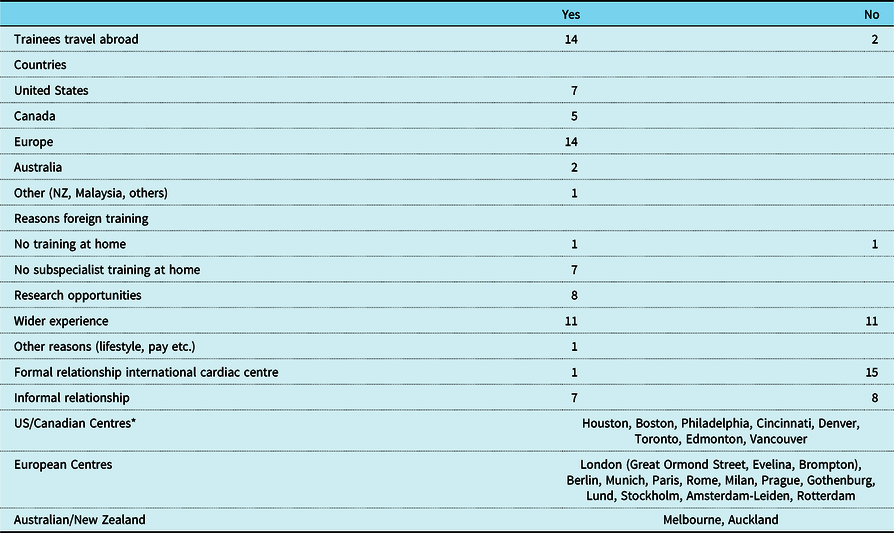
NZ, New Zealand; US, United States of America
* Listing of international centres provided by delegates is not exhaustive but the majority of centres are listed
Regression on gross domestic product
Although there was an estimated relationship between the total number of paediatric cardiologists and gross domestic product (R2 = 0.41) (Fig 5), this result weakened when adjusted for cardiologists per million population (R2 = 0.014). Of note, the two countries (Iceland and Cyprus) with no paediatric cardiology training programme had the lowest gross domestic product (19,022 and 20,841 million euros, respectively) of the countries studied.

Figure 5. Relationship of paediatric cardiologists per million population and gross domestic product.
Training in transition care
Only five (31%) of sixteen delegates reported formal training on transition of patients from paediatric to adult services.
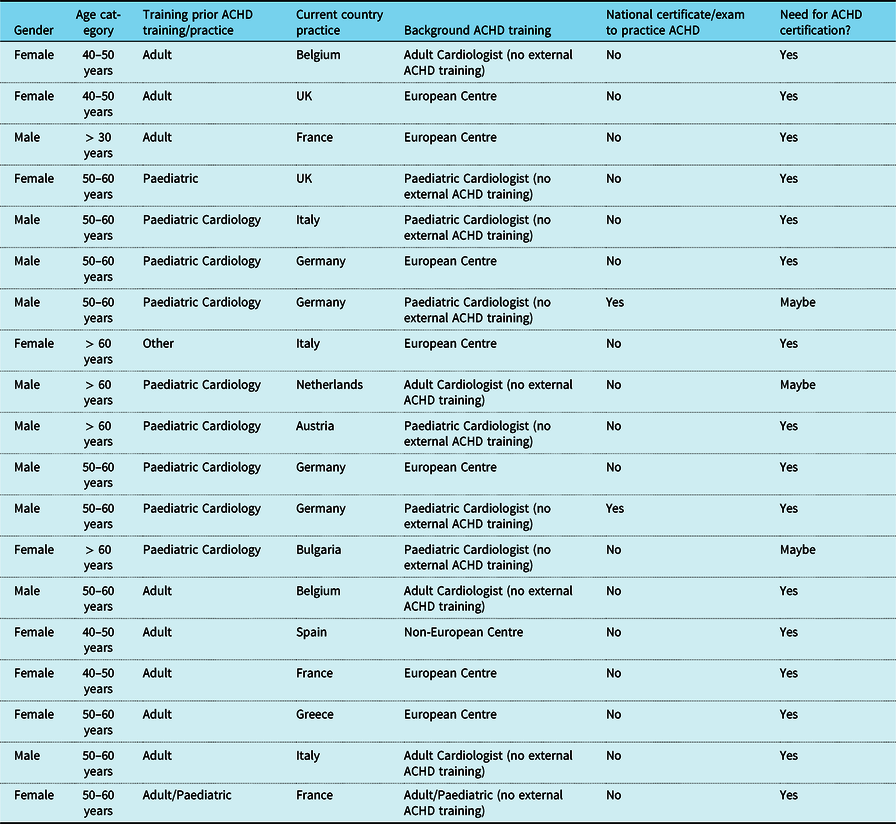
Adult CHD training in Europe
Nineteen adult CHD consultants responded to a survey on entry criteria, their training, and their opinion on need for certification and examination (Table 6). There was a wide variation in entry criteria and forms of adult CHD training (via adult or paediatric cardiology specialities). Only two respondents from Germany reported a formal and certified training programme (German cardiology and paediatric cardiology society) which is needed to practice in their country and ends with a formal oral examination. In addition, some local medical councils in Germany have started a formal training programme for paediatric and adult cardiologists, which is also certified with a formal oral examination. In France, adult CHD training is included in both paediatric and adult congenital programmes but there is no exit examination or certification for adult CHD. The majority of adult CHD consultants surveyed (16, 84%) expressed that introduction of some form of adult CHD certification would be helpful.
Table 6. Adult CHD consultant demographics, ACHD training, current certification, and potential adoption of certification.
Discussion
Training to become a paediatric cardiologist in Europe varies markedly from one country to another, and although there is excellent training in many countries, there is potential for improvement in consistency of training and certification in several countries. A single common examination set to a certain recognised level across Europe would help towards improving this consistency. Europe is a unique continent from a cultural, geographical, and geopolitical standpoint. There is a broad mixture of large (>20 million population, n = 8), medium (8–20 million, n = 11) and small countries (<8 million, n = 11) represented in this study. These countries possess unique languages, cultures, and not infrequently significant disparities in resources and gross domestic product. Perhaps it is not surprising therefore that these disparities are reflected in the wide variation in training patterns of paediatric cardiologists across Europe reported in our study, not dissimilar to adult CHD reports from other continents. Reference Gurvitz, Chang, Ramos, Allada, Child and Klitzner17 The study demonstrated a wide variation from highly structured formalised training (often with exit examination), informal but substantial training (more often than not without exit examination), to no formal training (invariably but not always in smaller countries or countries with limited resources, for example even resource-rich countries like Norway have limited training structures).
A surprising finding from this study was the realisation that paediatric cardiology, as a distinct speciality, is not recognised in several countries (Spain, Italy, Norway, Denmark, Belgium, Slovenia, and Greece), thereby undermining the potential to develop a training framework where no speciality recognition exists. Some delegates reported that their Ministry of Health was tentative to provide recognition when requested which may reflect funding implications were they to recognise the speciality. This was a particularly stark finding when one considers that the speciality was recognised back in 1957 by the American Academy of Pediatrics and that Board examination for certification and training programmes were established in 1961 in the United States. Reference Engle18 Despite this wide variation in training practice between individual European countries, this paper does not seek to delegitimise such training but instead ask how efforts to harmonise and standardise training can be developed and implemented. Moreover, formal recognition of their level of training could potentially aid such “accredited paediatric cardiologists” with greater flexibility in working across different European countries.
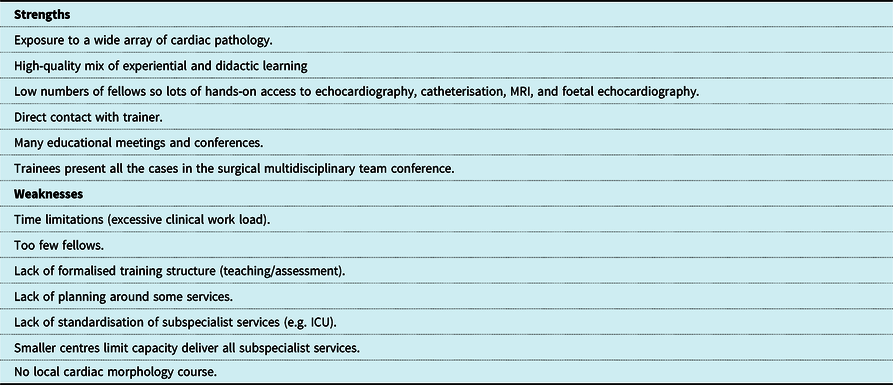
Our goal in training paediatric cardiologists should be to provide them with the critical competencies/capabilities to be safe to work as independent cardiologists providing high-quality care to patients in their defined work environment. Such training can prove stressful for trainees even in well-structured programmes; hence, it is critically important that the training provided be of high-quality and relatively standardised across different borders. Reference Brown, Binney, Gauthier and Blume19,Reference Horst, Michel, Kubicki, Lang, Zschirnt and Moosmann22 Creative solutions in reducing stress may include novel instructional techniques (e.g. echocardiography bootcamp or simulation) which can be easily incorporated into training at an early stage to allay some of these pressures on trainees. Reference Ceresnak, Axelrod and Sacks20 Interestingly, some authors in the United States have argued that too much structure may be deleterious to training given that many paediatric cardiologists function in an outpatient or office setting in that jurisdiction. Reference Abdulla21 Matching training to the eventual everyday roles of the cardiologist is fundamentally important, in addition to ensuring cardiologists maintain their level of competence and capability in line with evolving practice and innovation. In this study, several delegates reported reassuring strengths of training (Table 7). Having smaller training programmes may counterintuitively prove a strength given the potential for close hands-on teaching, supervision of trainees, and easy access to trainers. There is most likely a sweet spot between training programmes that are too big and those that are too small.
Table 7. Paediatric cardiology trainers perceptions of strengths/weaknesses of training programmes.
Countries with no training facilities
Iceland and Cyprus are limited in population which makes it difficult for them to develop or sustain a training programme. Many cardiologists in smaller countries face challenges in achieving recognition of their speciality, providing comprehensive care and all the subspecialist components (electrophysiology, heart failure/transplantation/pulmonary hypertension, advanced imaging) in addition to achieving cardiac surgical outcomes comparable to large international centres.
Furthermore, limited access to a critical volume of patients, with significant disease severity, lack of a formal curriculum, high-quality instructional design, and most importantly time to train fellows may all prove barriers to effective training practices. Even once a training programme has been established, a need for regular standardised assessments, exit examination, and certification may prove a problem for smaller countries. It takes a significant amount of time and effort to construct an exit examination, which makes it unrealistic for small or even larger countries to individually develop this especially when one considers the small number of graduates in each country each year, for example the United Kingdom may only have 15–20 trainees graduating each year. Limited financial resources (gross domestic product) may also play a significant factor in limiting development of paediatric cardiology training (Table 2 and Fig 5).
Common problems in training
Several delegates reported many positive aspects of training in European centres (Table 7). Trainees themselves have previously reported high satisfaction with overall training from countries with well-established programmes. Reference Horst, Michel, Kubicki, Lang, Zschirnt and Moosmann22 However, it is clear that there is also room for improvement. One of the most cited problems in training was limited trainer time availability (Table 7). Many cardiologists are extremely busy providing clinical services, even with a median number of 4.2 cardiologists per million population. There is also a very wide disparity of resources in terms of the European paediatric cardiology workforce with a range of 0.9–11.8 cardiologists per million population. In the United States, there are 2860 paediatric cardiologists which represents 8.8 per million population. Reference Mehta, Fisher and Rzeszut23 It is not surprising that teaching and training may be at the bottom of the priority list in such under-resourced and challenging settings. Furthermore, one can surmise that limited investment in fragile public health services over the last few decades, Reference Mackenbach, Stirbu and Roskam24,25 highlighted in many countries by the current COVID-19 pandemic, may have compromised our European wide capacity for future training and evolution of paediatric cardiology and indeed wider medical services. Differences between privately and state-funded healthcare provision may also significantly impact upon the availability of training, location of training, and indeed career outcomes of trainees.
Other weaknesses reported included too few fellows in the programme, lack of formalised training structure (teaching/assessment), Reference Horst, Michel, Kubicki, Lang, Zschirnt and Moosmann22 lack of standardisation of subspecialist services, smaller centres with limited capacity to deliver all subspecialist services, and lack of local access to a cardiac morphology course. The latter is more recently becoming more readily achievable remotely as well as via the excellent “in person” courses run in the United Kingdom (Great Ormond Street Hospital, Royal Brompton & Harefield hospitals (rbt.nhs.uk) and via the online Heart Academy (cardiacmorphology.com)). The lack of access to all subspecialist services is a challenge for smaller countries (e.g. electrophysiology training is a much bigger challenge on both small and large countries alike). Some have also questioned how subspecialised training should be, given that many paediatric cardiologists will spend much of their time in an outpatient setting, and not more subspecialised settings. Reference Moodie26 This does however beg the question that the outpatient setting in some ways requires the highest level of specialisation; the need to acquire and maintain the most current and ongoing knowledge of all treatment modalities available for patients, for conditions where optimisation of timing for optimal intervention or reintervention is crucial. Balancing these needs is difficult.
Comparison with North American training
Training in North America is generally well organised to a high standard with a standardised curriculum accepted by most programmes. There are 60 paediatric cardiology fellowship programmes in the United States (https://www.nrmp.org/fellowship-match-data/). Core training is 3 years with the option of completing a fourth year in advanced training. Most cardiac programmes have a dedicated fellowship director who meets regularly with trainees and monitors their progress in reaching the six competencies promoted by the Accreditation Council for Graduate Medical Education. Europe could adopt a similar curriculum and structured core programme of 3 years with the option of a fourth subspecialisation year.
The European Working Time Directive has also impacted the need for a longer duration of training in European countries to meet the competencies required for satisfactory completion of training compared to a what was previously a more intensive shorter period of training in the United States. However, between 2004 and 2015 the number of United States paediatric cardiology fellow positions increased from 61 to 141, primarily to take account of the implementation of work hour restrictions there also. Reference Ross, Srivastava and Cabrera27
One of the challenges for European programmes is significant resource limitation especially in terms of “teaching faculty”. Medium-sized North American programmes often have 20–30 members on their faculty while larger programmes (Houston, Boston) may have in excess of 60–70 faculty members, with a dedicated fellowship director who has often received formal educationalist training. This enables faculty members to spend greater time training and also undertaking fellow assessments. Increased resources, often a challenge for smaller European centres, in terms of faculty and educationalist training are critical to implementing an effective training framework. Medical systems in Europe often differ radically to those in the United States where institutions and departments may be remunerated for patient care, whereas a public healthcare system is employed in most European centres. These stark differences in training infrastructure may pose practical dilemmas for trainees embarking upon their careers. Where there is a real or even perceived lack of “parity of esteem” between European and North American centres, trainees may feel their chance of securing a consultant position is greater if they spend 3–4 years training in a North American centre compared to a comparable European centre, where the training may be as long as 5 years of duration. We must ask ourselves the question is it fair to ask our trainees to train for longer in a programme with less resources to be less competitive than a comparable trainee who spends less time training in a better-resourced international centre?
Another notable difference between North American and European programmes is the dedicated time apportioned to research. The Accreditation Council for Graduate Medical Education mandates that 12 months of the 3-year United States programme be devoted to research (typically towards the latter part of the programme) while the majority of European programmes had no dedicated time or relatively limited time specifically for research without taking time out of training (Table 4). This may be partly accounted for by the larger numbers of fellows in North American programmes (some exceeding 20 fellows per programme) and the fact that highly reputable programmes often attract international research fellows, some of whom provide their own funding. There are very few European programmes with such high numbers of fellows so service provision and patient care may be the primary focus in those less well-resourced centres.
Realistically, every trainee cannot go to North America to train as not only are there limited training positions and challenges in meeting entry criteria (United States Medical Licensing Examinations) but also because they would be returning to a very different healthcare system. More recently, completion of a paediatric residency in the United States is also required prior to starting fellowship training, potentially requiring experienced trainees having to repeat general paediatric training. Furthermore, not every European country may recognise United States Board certification qualifications for entry onto the specialist register (e.g. United Kingdom) even when they are secured.
To address some of these challenges in training, the educational committee of the Association for European Paediatric and Congenital Cardiology was established. The committee is composed of several members from multiple different European countries with broad levels of experience and expertise, includes a junior representative, and has adopted a very active role in developing guidelines for general paediatric cardiology and individual subspeciality training (published by working groups) in addition to the development of a logbook. Reference Kriebel, Rosenthal and Gebauer10–Reference Moons, Bratt and De Backer16 It is currently in the process of establishing a European exit examination which could be recognised across all countries (AEPC certificate). The European Association of Cardiovascular Imaging echocardiogram examination has been a very successful benchmark model examination. A comparable knowledge-based examination although a challenge to develop could prove a useful development.
Should all training be in surgical centres?
Across Europe, there are some major teaching hospitals that have some specialised paediatric cardiology inpatient services but without surgery or interventional cardiology on site. The overall complexity and intensity of CHD case exposure at surgical centres generally exceeds that at the non-surgical cardiology centres. Consequently, we would advocate for trainees to be able to spend the majority of their time in surgical centres so as to receive exposure to complex cardiac physiology and be involved in the post-operative management of patients but fully acknowledge that there can be significant benefit from rotations that include time in non-surgical centres as well, for example, in the Irish training scheme trainees rotate through the Dublin surgical centre for the majority of their training but also rotate through Belfast where there is benefit from the well-established cardiology service and strong research aspects of training as well. Even though many countries surgical centres function as their main training centres (Table 1), there is also likely benefit from rotations even between major surgical centres as learning can be gained from “more than one master”. In countries with none or very limited surgical programmes, the potential for trainees to rotate through other surgical centres in other countries would be important.
Adult CHD training
To date, there is no uniformity of provision of adult CHD training across Europe. Many of the problems are similar to those for paediatric cardiology. On the one hand, many paediatric cardiologists have grown older together with their patients and have continued to care for them. These paediatric cardiologists have usually been trained in adult CHD because of their ongoing clinical practice. On the other hand, adult cardiologists have also begun to focus on the care of adolescents and adults with CHD. With their internist background, they lean more towards adult care and have more training and experience in both acquired heart disease and the wider diseases of ageing. For more than 20–30 years, they have been proficient in the care of adult CHD patients through a more practice-based approach. Both type of specialists can be considered as “made by the job.”
Meanwhile, the number of patients with CHDs reaching adulthood has steadily increased, so that more adult CHD healthcare providers are gradually required. Reference Baumgartner28 Expert centres worldwide which had already developed a well-structured adult CHD programme opened the doors for training paediatric cardiologists and adult cardiologists to become fully fledged adult CHD specialists. Many adult CHD specialists undertook clinical training in the United Kingdom or outside Europe. In the meantime, several expert centres have emerged on European soil which can offer full-fledged training to adult CHD specialists. Reference Baumgartner, Budts and Chessa29 It goes without saying that as the need to align training courses grew, thought was given to the minimum content of clinical training to become an adult CHD specialist. Few recommendation papers for general and more specific training in the adult CHD subspeciality were published over last decade. Reference Baumgartner, Budts and Chessa29–Reference Chessa, Baumgartner and Michel-Behnke32
As a result, a European certification for adult CHD specialists is also currently being considered. Certification would likely entail passing a theoretical exam and would also require a minimum of clinical exposure. It is unclear how best this should be considered at present, but the best candidates to undertake this may be European scientific societies already responsible for training and research. How this European certificate could be introduced in the different countries is included as reflection. Few countries currently require an examination or certification to practice adult CHD (Table 6). Although the majority of adult CHD consultants surveyed believed European certification would help to standardise training, the marked heterogeneity (gross domestic product, healthcare organisation, health insurance, organisation of teaching, and education) across European countries may well pose a challenge for regulation and standardisation of training.
Proposed solutions
The findings from this study highlight the continuing question of how we can improve training support for countries with limited resources. We propose the following initiatives:
-
To support colleague countries in applying to their Ministry of Health for formal recognition of subspeciality status of paediatric cardiology and adult CHD as independent specialities. This recognition is fundamental to providing a framework for training. In some countries limited gross domestic product may dramatically impact development of medical services including paediatric and adult congenital cardiology and funding streams may need to be developed to enable greater training and service development for such disadvantaged countries.
-
To standardise the curriculum across different European countries, respecting there may be some specific competencies required in individual population groups.
-
To increase awareness of competency and “capability” based medical education (much of the Shape of Training, United Kingdom Reference McMahon, Tretter and Redington1 ). This provides a useful model framework which is important to ensure trainees are capable in each of the competencies they require. Reference McMahon, Tretter and Redington1,Reference Narang, Velagapudi and Rajagopalan33
-
To establish and standardise formal fellowship training with recommendations for standard fellowship duration (3–5 years), rotations, and expected levels of entrustment and capability. We should ensure there is a focus on high-quality training and not simply counting the numbers of echocardiograms, catheters, electrophysiology studies, outpatient clinics which should be completed during training. The logbook could record the quality as well as the number of studies performed by the trainee. Recognising levels of entrustment to undertake “only under supervision,” “with limited supervision,” or “unsupervised” provides an excellent model.
-
Most countries can offer basic level fellowship training (years 1–3). It is a credit to the speciality that much progress has been made in training subspecialists (e.g. electrophysiology, foetal cardiology and cardiac catheterisation). However, the vast majority of European cardiologists will spend most of their time looking after undifferentiated patients outside their area of special interest, either in the outpatient clinic, while on service or on call. It is critical that trainees are thoroughly grounded in “basic” or general paediatric cardiology so they can safely treat common paediatric cardiology problems. Reference Shkolnikova, Osokina and Abdulatipova34
-
Encourage streamlining of advanced training (fourth or fifth year training) to larger centres for advanced imaging, catheterisation, electrophysiology, heart failure/transplantation/pulmonary hypertension. By concentrating resources on advanced training to high-volume/high complexity European cities/centres this may obviate the need to train in United States/Canadian centres, although that remains within the prerogative of the trainee. Many current trainees already travel to North America or a major European centre.
-
Develop partnerships between countries with limited training support and larger better resourced countries with a track record in training congenital cardiologists. Although there may be language and logistical barriers to overcome this would appear to be a viable solution to such a heterogenous collection of countries. Potential collaborations/hubs of training, some already partially established, could be established between different countries, for example Norway, Sweden, Finland, Denmark and Iceland each with populations between 0.3–10 million could form a Nordic block (cumulative population >27 million) for training in both basic paediatric cardiology but also subspecialist training. Alternatively trainees from smaller countries with limited resources may benefit from an exchange programme undertaking elective periods (comparable to the Erasmus scholarship) at larger better resourced centres to supplement their training.
-
The Association for European Paediatric and Congenital Cardiology as a governing structure is in a unique position to foster the birth, growth and development of such partnerships. Traditionally many trainees move to a handful of European centres (London, Paris, Rome, Milan, Berlin, Prague) or to United States/Canadian/Australian centres (Houston, Boston, Cincinnati, Philadelphia, Toronto, Edmonton, Melbourne) for advanced subspecialist training but it may be feasible that there is an equitable distribution of trainees around different European centres.
-
Provide a common exit knowledge-based assessment, currently under preparation, which would lead to European Board Certification qualification. This could be standardised which would facilitate transfer of professional qualifications across different European countries. In addition, certification should focus on quality and competencies rather than purely on numbers of procedures performed/attended. Entrustable professional activities are also an effective means of bridging the gap between competency frameworks and clinical practice and will likely increasingly become incorporated into trainee assessment and certification. Reference Ten Cate35
-
Develop and expand formal adult CHD fellowships across a greater number of countries given the current critical need to train adult congenital cardiologists to care for these patients. There is clear support among a majority of surveyed practitioners for introduction of a certification process for adult CHD training.
-
The Association for European Paediatric and Congenital Cardiology education group can offer educational courses to educate trainers in instructional design and novel learning techniques (e.g. problem-based learning and simulation). The European Society Cardiology also advocates for training by hosting the CHD echocardiography certification examination (European Association of Cardiovascular Imaging).
-
Encourage utilisation of novel pedagogical strategies including online learning, for example webinars (“Heart University,” “Congenital Heart Academy,” and “World University for Paediatric and Congenital Heart Surgery”). COVID-19 has shown us that there are many new ways to deliver very high-quality training; virtual delivery of some parts of the fellowship training series online and greater subspeciality virtual meetings can be leveraged to benefit European but also a wider global trainee audience, while remaining cognisant of the webinar fatigue which can arise from overexposure to these technologies. Reference McMahon, Tretter and Redington1,Reference Tretter, Windram and Faulkner36–Reference McMahon, Tretter, Faulkner, Krishna Kumar, Redington and Windram38
-
The Association for European Paediatric and Congenital Cardiology can also advocate for educational sessions at research meetings including the annual meeting. There are already some exceptional educational courses (London morphology courses, Association for European Paediatric and Congenital Cardiology working group courses) which could be replicated and extended to different subspecialities. Morphology is the bedrock of paediatric cardiology: many national delegates emphasised that attending a recognised course should be mandatory for all trainees.
-
Support ongoing research into the medical education of congenital cardiologists will assist in improving education and training for all our trainees. Funding sources (national and European wide) should be sought to invest in the education and training of congenital heart specialists.
These proposals outlined to provide greater consistency in training are purely that, proposals, and will require ongoing dialogue and planning among several countries under the Association for European Paediatric and Congenital Cardiology framework. This paper is only as useful as the tangible measurable real-life benefits accrued to our trainees and by extrapolation to our patients. Change is frequently difficult and often slow. The real work begins now and over the coming years to bring these proposals to fruition: we hope this opportunity is not squandered. While standardisation tends to improve overall standards of training, we recognise within individual countries there may be conditions that require specific training to care for the local population. Reference McMahon, Tretter and Redington1 We welcome input from Association for European Paediatric and Congenital Cardiology affiliated countries who could not avail of the opportunity, at this time, to participate in this study. We look forward to collaborating with countries to improve training and education for congenital cardiologists.
Limitations
Despite persistent efforts to enrol all countries in this study, some countries’ national delegates could not be reached. Of the national delegates who responded, not every delegate was able to furnish a complete data set for all the variables we studied, due in part to the high variation of training delivery in some countries. We relied on each national delegate providing accurate data related to their country. To ensure data accuracy, we requested the national delegate from each country to review the finalised paper very carefully for potential inaccuracies. Although countries with a formal accredited fellowship are easy to identify, the differentiation between informal but substantive training can prove a challenge and there are nuances in training in specific countries. Characterisation of training did not always fall into a “neat box.” Where this existed, we quoted the national delegates to maintain accuracy and clarity in reporting. The assignment of “formal” or “informal” training is not meant to denigrate training in certain countries but to accurately reflect whether training is nationally recognised, with established exit examination and certification. We apologise if the use of such terms appears pejorative but that was not the intention. The ratio of paediatric cardiologist per million population may have slightly over or underestimated this ratio as the definition of one whole time equivalent paediatric cardiologist may vary from country to country. Small private practice institutions were not included in this study. Furthermore, the exact definition of a “paediatric cardiologist” may vary subtly between countries: we aimed to include only those who had completed paediatric cardiology training and practised actively as a paediatric cardiology specialist. Development of research competency is a critical part of training fellows (representing up to 12 months of the 36 month North American fellowship), and complete data from all European countries were not available. Further detailed work on adult CHD training will provide further insights into the needs of these trainees.
Conclusion
In conclusion, education and training of paediatric and adult congenital cardiologists varies markedly across the continent of Europe. This paper maps the current training landscape and proposes initiatives towards a more standardised and organised approach, which will hopefully facilitate better trained paediatric and adult congenital cardiologists into the future. The goodwill of national delegates and multiple trainers witnessed through their active engagement in this study bodes well for future progress in this important area. Further dialogue between all stakeholders and listening to trainers and trainees experiences will help expedite such progress and hopefully build bridges of collaboration between our colleagues across Europe. Only by working together to find common pan European solutions which can be successfully implemented and sustained can this vision for excellence in paediatric cardiology and adult CHD training and care be fully realised across the continent.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S104795112100528X
Acknowledgements
We are grateful to the Association for European Paediatric and Congenital Cardiology council and educational committee for their support in undertaking this project.
Ms. Linda Bosschers provided enormous assistance in finalising questionnaires and coordinating the project. Drs. Igor Kovalev, Angelina Yakshina and Gulnara Okhramenko assisted in completing the questionnaire from the Russian delegation. Dr Adam James reviewed the questionnaire. Mr. Andrew Pendred generated the maps.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of interest
None.
Ethical standards
Approval of the above study was obtained from the Ethics Department at CHI Children’s Health Ireland, Crumlin, Dublin Ireland.















