Ebstein anomaly and tricuspid valve dysplasia are rare forms of CHD, occurring in 1 per 10,000 live births and accounting for 3–7% of all CHDs. Reference Hoffman and Kaplan1 Although Ebstein anomaly and tricuspid valve dysplasia are embryologically and anatomically different, they share similar pathophysiology and fetal presentation and encompass a broad spectrum of severity; ranging from mild, asymptomatic tricuspid regurgitation to severe tricuspid valve dysfunction with massive enlargement of the right heart chambers. Reference Freud, Escobar-Diaz and Kalish2 Because of their striking ultrasound findings, severe forms of Ebstein anomaly and tricuspid valve dysplasia are usually recognised on prenatal ultrasound screening.
Survival in patients with severe Ebstein anomaly and tricuspid valve dysplasia has improved over recent years and is attributed to advances in perinatal clinical management. Reference Freud, Escobar-Diaz and Kalish2–Reference Torigoe, Mawad and Seed4 While early studies reported perinatal mortality rates of up to 80%, mortality has dropped to around 45% in the last decade. Reference Wertaschnigg, Manlhiot and Jaeggi3,Reference Celermajer, Cullen, Sullivan, Spiegelhalter, Wyse and Deanfield5 Importantly, the use of prenatal non-steroidal anti-inflammatory drugs to induce ductal restriction and limit circular shunting, and the adoption of a single ventricle palliative strategy during the neonatal period in the most severely affected patients have been associated with survival in even the most severe forms of Ebstein anomaly and tricuspid valve dysplasia. Reference Freud, Escobar-Diaz and Kalish2,Reference Torigoe, Mawad and Seed4
Patients surviving surgery for severe forms of CHD are at risk of life-long neurodevelopmental impairment. Reference Marelli, Miller, Marino, Jefferson and Newburger6 Among CHD subtypes, patients with Ebstein anomaly and tricuspid valve dysplasia probably exhibit the most profoundly abnormal perinatal haemodynamics. Reference Marelli, Miller, Marino, Jefferson and Newburger6 However, data concerning long-term neurodevelopmental outcome in fetuses with Ebstein anomaly and tricuspid valve dysplasia are lacking. These data are needed for prenatal counselling. Therefore, the first aim of this study was to characterise the neurodevelopmental outcome of this population.
Currently, prenatal ultrasound is used to diagnose and evaluate the severity of fetal Ebstein anomaly and tricuspid valve dysplasia, while Doppler also provides information about the impact of these cardiac malformations on the peripheral and cerebral circulations. However, ultrasound is not routinely used to obtain quantitative vessel blood flow measurements and does not provide a direct assessment of fetal oxygenation. Therefore, the secondary aim of this study was to examine cardiovascular haemodynamics in fetuses with Ebstein anomaly and tricuspid valve dysplasia using fetal cardiovascular magnetic resonance and to determine their impact on surgical outcome, cerebral growth, and neurodevelopmental outcomes.
Methods
This is a retrospective single-centre case–control study including all fetuses diagnosed with Ebstein anomaly or tricuspid valve dysplasia between May, 2013 and December, 2019 at the Hospital for Sick Children, Toronto. Fetuses with Ebstein anomaly and tricuspid valve dysplasia associated with other forms of CHD such as congenitally corrected transposition of the great arteries, and those having had a postnatal diagnosis were excluded. The study was approved by our Research Ethics Board.
Fetal echocardiography
Prenatal ultrasound findings of Ebstein anomaly and tricuspid valve dysplasia were classified according to the criteria reported by Wertaschnigg et al. Reference Wertaschnigg, Manlhiot and Jaeggi3 This included calculating the “SickKids score” at each visit, which assigns a score of 0, 1, or 2 for each of 5 echocardiographic findings based on the severity of the abnormality to predict the risk of mortality. Scores >8/10 were obtained in patients with the most severe forms of Ebstein anomaly/tricuspid valve dysplasia who had typically developed pulmonary regurgitation and were generally treated with maternal indomethacin in an attempt to limit the circular shunting by inducing restriction at the ductus arteriosus. Reference Torigoe, Mawad and Seed4
Table 1. Maternal and fetal characteristics
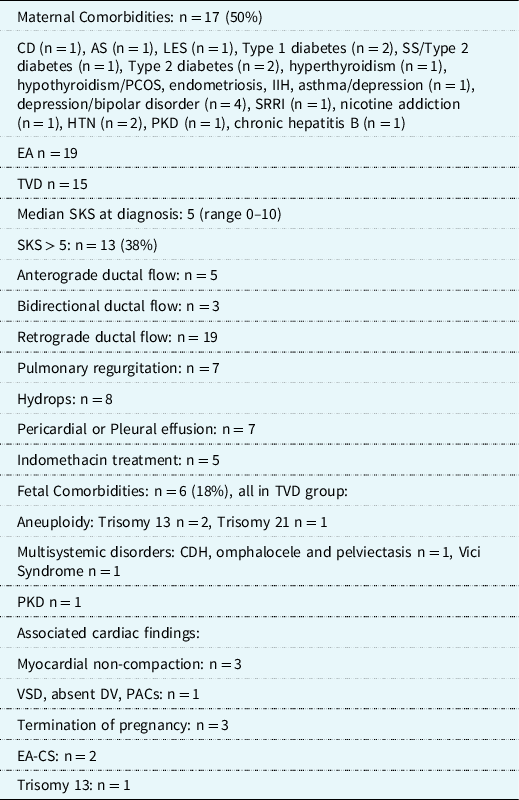
AS: ankylosing spondylitis, CD: Crohn’s disease, CDH: congenital diaphragmatic hernia, CS: circular shunt; EA: Ebstein anomaly, HTN: hypertension, IIH: idiopathic intracerebral hypertension, PACs: premature atrial contractions, PCOS: polycystic ovary syndrome, PKD: polycystic kidney disease, SLE: systemic lupus erythematosus, SSRI: selective serotonin reuptake inhibitor, SS: Sjogren’s syndrome, TVD: tricuspid valve dysplasia; VSD: ventricular septal defect.
Fetal cardiovascular magnetic resonance
Fetal cardiovascular magnetic resonance was performed using a 1.5-Tesla clinical MRI system (Siemens Avanto, Erlangen, Germany) as previously described. Reference Seed, van Amerom and Yoo7,Reference Sun, Macgowan and Sled8 Our protocol includes a 3D steady-state free-precession volume of the entire fetus, cine phase-contrast MRI and T2 mapping of the major fetal vessels. Reference Sun, Macgowan and Sled8,Reference Prsa, Sun and van Amerom9 Segmentation of the 3D-steady-state free-precession volume was performed using a commercially available post-processing software (Mimics, Materialize, Leuven, Belgium) and used to calculate the estimated weight using previously reported conversion factors. Reference Roelfsema, Hop, Boito and Wladimiroff10 The combined ventricular output was calculated as the sum of the ascending aorta and the main pulmonary artery flows plus an additional 3% estimated for coronary blood flow. In the setting of functional pulmonary atresia, the combined ventricular output was calculated as ascending aorta flow plus 3% estimated for coronary blood flow, while pulmonary blood flow and thus ductus arteriosus flow were calculated as the difference between combined ventricular output and the total systemic perfusion, which is given by the sum of superior caval vein flow and descending aorta flow. Peripheral perfusion was defined as the sum of superior caval vein and descending aorta flows. Flows were indexed to fetal weight. As previously described, we employed quantitative measurements of the T2 relaxation of blood in the major vessels to achieve magnetic resonance oximetry, which combined with the cine phase-contrast analysis of the vessel flow, allowed us to calculate fetal and cerebral oxygen delivery (DO2) and consumption (VO2) according to the Fick principle. Reference Sun, Macgowan and Sled8,Reference Saini, Darby and Portnoy11 The haemodynamic findings in fetuses with Ebstein anomaly and tricuspid valve dysplasia were compared with those obtained in a control group of 30 healthy fetal control subjects recruited from a low-risk obstetric outpatient clinic and examined using the techniques described above.
Surgical and neurodevelopmental outcomes
For patients with circular shunt, perinatal management recommendations included delivery by caesarean section and early neonatal surgery to eliminate the circular shunt and stabilise the circulation. This was either achieved with ductal ligation if the RV performance was considered adequate to achieve a biventricular repair or by ligating the main pulmonary artery and over-sewing of the tricuspid valve to exclude the RV and establish stable single ventricle physiology (modified Starnes operation). Surviving newborns and infants underwent clinical brain MRI before discharge, including 3D T1-weighted gradient-echo, axial diffusion-weighted imaging, axial and coronal T2-weighted fast spin-echo, axial susceptibility-weighted imaging and magnetic resonance spectroscopy targeting the left basal ganglia. Reference Lim, Porayette and Marini12 Total brain volume was obtained by segmenting the 3D T1-weighted volume, and total brain weight and total brain weight z-score were calculated according to our previously published method. Reference Lim, Kingdom and Saini13 In 2014, we initiated a cardiac neurodevelopmental follow-up programme at our centre, whereby all patients undergoing cardiopulmonary bypass in the first 6 weeks of life are referred for clinical neurodevelopmental follow-up. This includes clinical assessments at ages 8, 12, 18, and 36 months. Standardised assessments using the Bayley Scales of Infant Development–3rd edition are completed at the 18- and 36-month visits. In addition to fetal cardiovascular magnetic resonance and brain MRI data, we collected a range of information about the spectrum and progression of the cardiac disease as assessed by fetal echocardiography, as well as details regarding surgical management and neurodevelopmental follow-up.
Statistical analysis
Continuous data are expressed as mean± SD. Normal distribution of the data was confirmed using a Kolmogorov Smirnov test and an unpaired Student’s t-test was used to compare different parameters between the control and Ebstein anomaly and tricuspid valve dysplasia groups. A non-parametric Kruskal–Wallis test was used to examine differences in Ebstein anomaly and tricuspid valve dysplasia patients with circular shunt, versus those with no circular shunt and controls. The correlation between fetal superior caval vien, descending aorta (superior caval vien + descending aorta) flows and cDO2 with fetal brain weight Z-score, and postnatal brain weight Z-score were assessed by using simple linear regression. P < 0.05 were considered statistically significant. All statistical analyses were performed using GraphPad Prism 6.0 (GraphPad Software Inc., La Jolla, CA).
Results
Fetal population and overall survival, clinical management, and surgical outcomes are summarised in Figure 1 and Table 1. Spontaneous in utero demise occurred in 5 patients (15%) (Table 2). Four in utero deaths occurred after 33 weeks' gestation while one fetus died before 30 weeks' gestation. The fetal demise occurring closest to term (37 weeks) was in a patient in whom the family had decided on a palliative approach to perinatal management following a late diagnosis of Ebstein anomaly at 35 weeks. There were 26 live-born patients (76%).
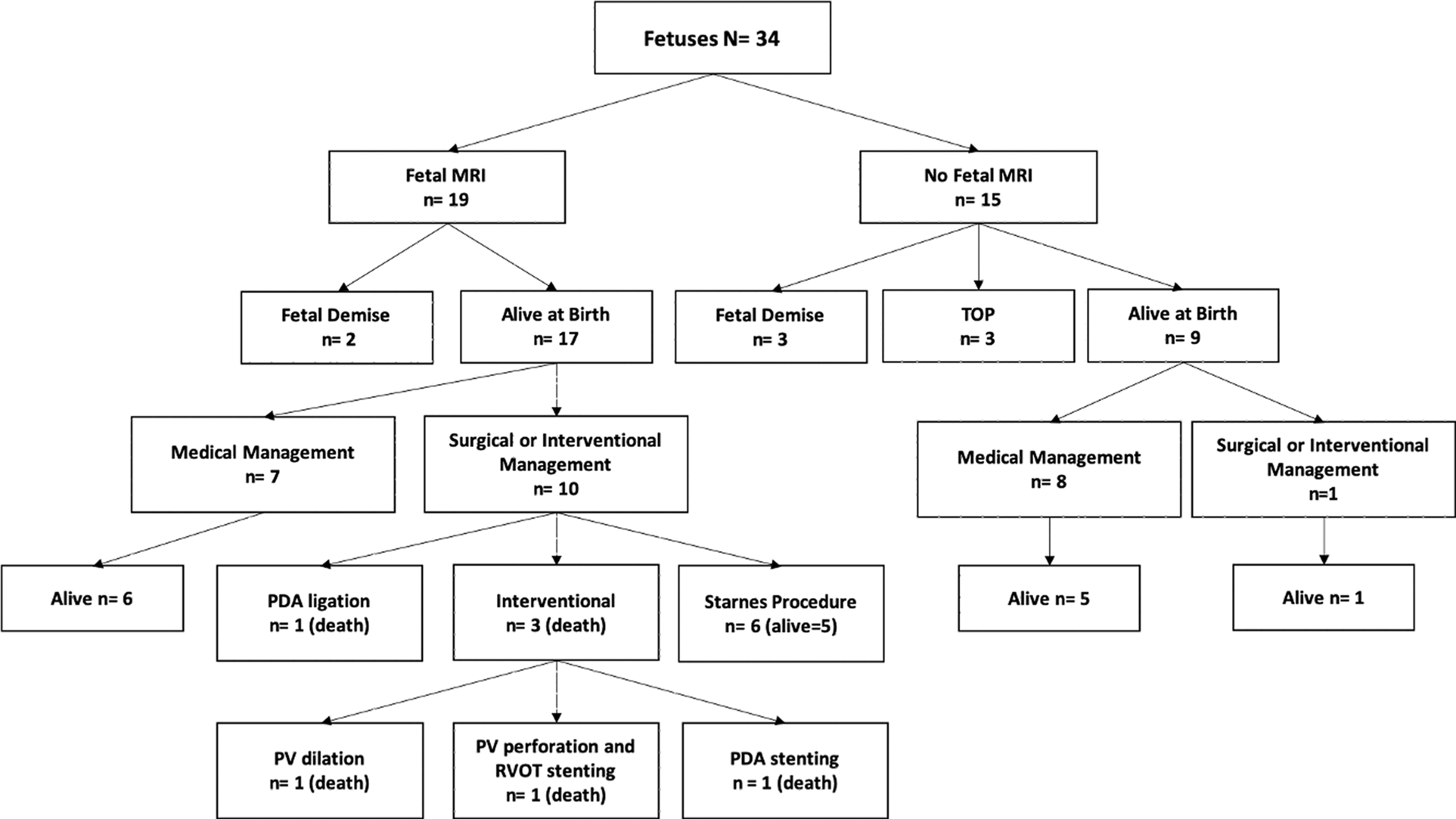
Figure 1. Overall population of fetuses with Ebstein anomaly and tricuspid valve dysplasia referred in the interval 2013–2019 with clinical management and surgical outcomes. Legend: EA: Ebstein anomaly; PDA: patent arterial duct; TOP: termination of pregnancy, TVD: tricuspid valve dysplasia.
Table 2. Characteristics of fetuses with Ebstein anomaly and tricuspid valve dysplasia with spontaneous in-utero demise

CDH: congenital diaphragmatic hernia; EA: Ebstein anomaly; GA: gestational age; w: weeks; SKS: SickKids score; TVD: tricuspid valve dysplasia.
Fetal haemodynamics by cardiovascular magnetic resonance
Nineteen fetuses underwent fetal cardiovascular magnetic resonance. A comprehensive haemodynamic assessment was obtained in 17/19 cases with Ebstein anomaly/tricuspid valve dysplasia and 30/30 controls. Fetal cardiovascular magnetic resonance could not be completed in two cases of Ebstein anomaly/tricuspid valve dysplasia performed at 32 weeks because of excessive fetal movement. A comparison of the haemodynamic findings in Ebstein anomaly/tricuspid valve dysplasia versus controls is summarised in Table 3. Within the Ebstein anomaly/tricuspid valve dysplasia group, five fetuses had circular shunt. Mean fetal total brain weight z-score was significantly lower than normal controls for patients with and without circular shunt (p < 0.0001 and p = 0.0007 respectively), while fetuses with circular shunt had the lowest mean total brain weight z-score (−2.2) (Fig 2). Following a similar trend, mean superior caval vien flow in the Ebstein anomaly/tricuspid valve dysplasia groups with and without circular shunt were significantly lower than in normal controls (p = 0.003 and p = 0.02, respectively). Fetuses with circular shunt had the lowest mean superior caval vien flow. Mean superior caval vien/combined ventricular output ratio was significantly different between Ebstein anomaly/tricuspid valve dysplasia patients with and without circular shunt. Although not reaching statistical significance, mean ascending aorta and combined ventricular output flows in Ebstein anomaly/tricuspid valve dysplasia patients with circular shunt trended higher than in those without circular shunt. We observed a progressive reduction in mean fetal total brain weight z-score, combined ventricular output, superior caval vien, descending aorta, and umbilical vien flows between normal control fetuses, fetuses with Ebstein anomaly/tricuspid valve dysplasia that were subsequently managed medically versus those that underwent surgical management (Fig 3). A similar progressive reduction in total brain weight z-score, combined ventricular output, superior caval vien, descending aorta, and umbilical vien flows were documented when fetuses managed with single ventricle palliation were compared to those undergoing interventional catheterisations and/or surgeries aimed at achieving a biventricular repair (Fig 4). Simple linear regression applied to a combined group of normal controls and Ebstein anomaly/tricuspid valve dysplasia fetuses revealed correlations between fetal brain weight z-score and peripheral perfusion (superior caval vien + descending aorta) (r2 = 0.54, p < 0.001), superior caval vien flow (r2 = 0.41, p < 0.001), descending aorta flow (r2 = 0.45, p < 0.001) and cDO2 (r2 = 0.47, p < 0.001) (Fig 5). Similarly, postnatal brain weight z-score correlated with fetal peripheral perfusion (superior caval vien + descending aorta) (r2 = 0.53, p < 0.001) and fetal superior caval vien flow (r2 = 0.46, p < 0.001); and fetal brain weight z-score (r2 = 0.65, p < 0.001) (Fig 6).
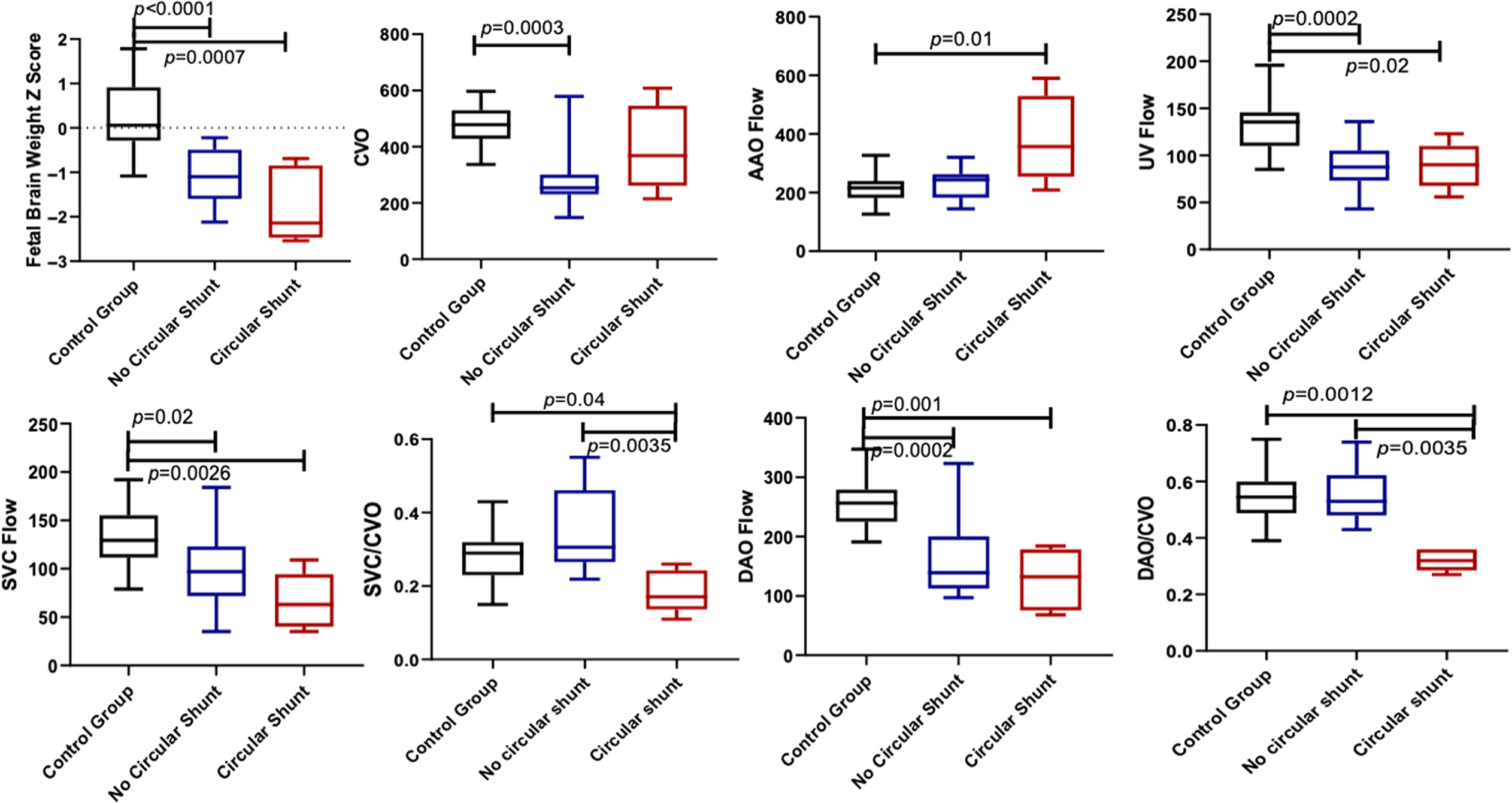
Figure 2. Comparison of haemodynamics measures between fetuses in control group, and fetuses with and without circular shunt. AAO: ascending aorta; CVO: combined ventricular output; DAO: descending aorta; SVC: superior caval vein; UV: umbilical vein.

Figure 3. Comparison of haemodynamics between fetuses in control group, fetuses not requiring and requiring surgery at birth. AAO: ascending aorta; CVO: combined ventricular output; DAO: descending aorta; SVC: superior caval vein; UV: umbilical vein.

Figure 4. Comparison of haemodynamics measures between fetuses in control group, those non-requiring surgery at birth, those undergoing Starnes procedure and other interventional and/or surgical procedures. AAO: ascending aorta; CVO: combined ventricular output; DAO: descending aorta; SVC: superior caval vein; UV: umbilical vein.

Figure 5. Correlations between prenatal brain weight z-score with superior vena cava flow, descending aorta flow, cerebral oxygen delivery and peripheral perfusion. DAO: cDO2: cerebral oxygen delivery; descending aorta; SVC: superior caval vien; (SVC + DAO): peripheral perfusion.

Figure 6. Correlation between postnatal brain weight z-score and prenatal brain weight z-score with superior vena cava flow and peripheral perfusion. SVC: superior caval vien; DAO: descending aorta; cDO2: cerebral oxygen delivery.
Table 3. Comparison of clinical and cardiovascular magnetic resonance findings between fetuses with Ebstein anomaly and tricuspid valve dysplasia and normal controls

AAO: ascending aorta; CVO: combined ventricular outflow; DAO: descending aorta; DO2: oxygen delivery; EA: Ebstein anomaly; GA: gestational age; SVC: superior caval vien; TVD: tricuspid valve dysplasia; UV: umbilical vein; VO2: oxygen consumption.
Clinical management and outcomes
Median gestational age at birth was 37 weeks (range 31–41 weeks). The prenatal diagnosis was confirmed in all live-born newborns. Among these, 11 underwent surgery and/or interventional catheterisations (surgical and interventional group) (Table 4), 15 newborns were managed medically (medical group). Overall mortality in newborns was 35% (9/26), while overall mortality of the original cohort of fetuses with an intention to treat was 43% (13/30). Two patients in the surgical and interventional group having severe forms of Ebstein anomaly with severe tricuspid regurgitation (SickKids Score 7 and 8) died following efforts to promote antegrade flow across the pulmonary valve in an attempt to achieve a biventricular circulation. Three patients died because of complications unrelated to their initial surgery or intervention (respiratory syncytial virus and parainfluenza bronchiolitis) or occurring once discharged at home (ductal stent thrombosis) or > 30 days after surgery when the patient was recovering and growing (Blalock Taussig shunt thrombosis). Including the patient that had thrombosis of the Blalock Taussig shunt, six newborns with severe forms of Ebstein anomaly/tricuspid valve dysplasia (median final SickKids Score 8, range 7–9) underwent a Starnes procedure. At a mean follow-up interval of 4 years (SD 0.8 years), all five survivors have undergone bidirectional cavopulmonary connection, three of whom have undergone completion of a total cavopulmonary connection. Within this group, two patients were born preterm and were prenatally treated with indomethacin because of severe circular shunt. Fifteen patients received only medical management (Table 5). Two neonates born preterm with severe comorbidities died on day 2 and day 14 before any palliative surgery or intervention could be attempted. Two patients died in infancy, one having Vici syndrome and the other trisomy 13. Of the remaining 11 patients, one underwent surgical correction at 3 years of age. Ten patients are doing well without any surgical intervention.
Table 4. Surgical and Interventional group: clinical outcome
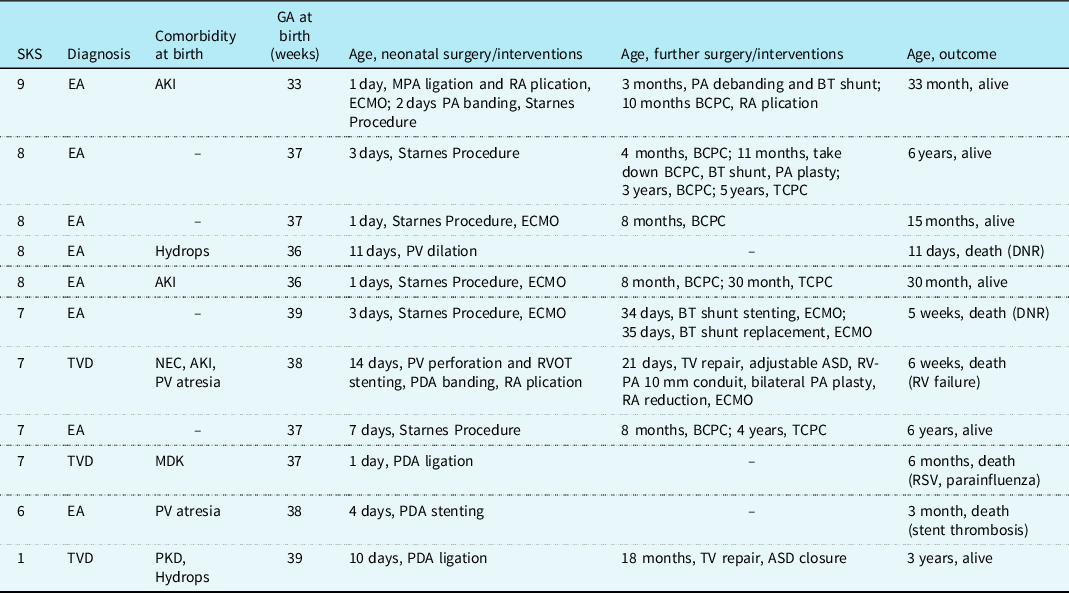
ASD: atrial septal defect; AKI: acute kidney inquiry; BCPC: bidirectional cavopulmonary pulmonary connection; BT: Blalock Taussig; DNR: do not resuscitate; GA: gestational age; MDK: multicystic dysplastic kidney; MPA: main pulmonary artery; PDA: patent ductus arteriosus; PKD: polycystic kidney disease; PA: pulmonary artery; PV: pulmonary valve; RA: right atrium; RSV: respiratory syncytial virus; RV: right ventricle; SKS: SickKids score; TCPC: total cavopulmonary connection; TV: tricuspid valve.
Table 5. Medical group: clinical outcomes
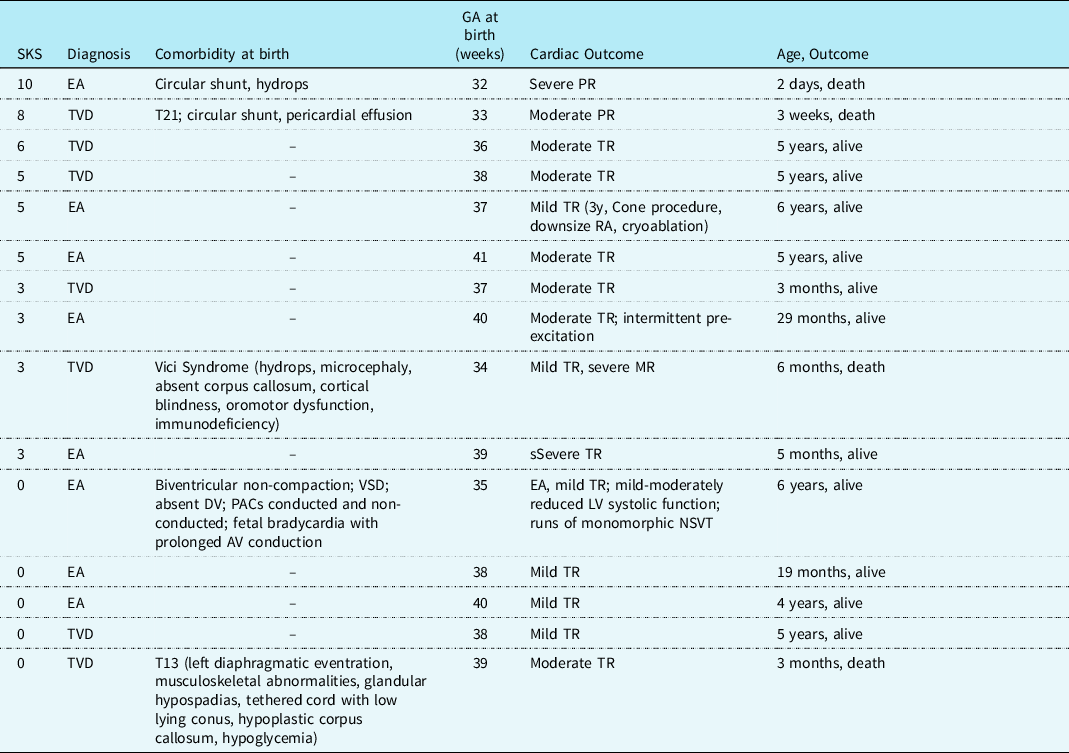
AV: Atrioventricular; DV: Ductus Venosus; MR: EA: Ebstein Anomaly; GA: Gestational Age; Mitral Regurgitation; NSVT: Non-Sustained Ventricular Tachycardia; PACs: Premature Atrial Contractions; RA: Right Atrium; SKS: SickKids Score; SVT: Supraventricular Tachycardia; T13: Trisomy 13; T21: Trisomy 21; TR: Tricuspid Regurgitation; TVD: Tricuspid Valve Dysplasia; VSD: Ventricular Septal Defect.
Postnatal Brain MRI findings
The brain MRI findings are summarised in Table 6. Infants in the medical group had a mean total brain weight z-score of −0.2 ± 0.2 at birth (n = 5, all SickKids Score 5 or 6), while those in the surgical group had a mean total brain weight z-score of −2.0 ± 1.0 (n = 5, SickKids Score range 7–10). Three of the patients in the surgical group had a brain MRI in the neonatal period revealing a mean total brain weight z-score of −1.2 ± 0.3. The other two infants born preterm with circular shunt had longer and more complicated postoperative courses, and their brain MRIs were performed at age 3 and 5 months, when their total brain weight z-scores were −3.6 and −2.8, respectively. The brain MRI was abnormal in all patients in which it was performed, even in those who did not require neonatal surgery: 7/10 had features of volume loss (enlarged CNS spaces and ventricular dilation), one had multiple foci of haemorrhagic stroke, one had mild white matter injury, one had moderate white matter injury and Grade 2 intraventricular haemorrhage, while two had diffuse excessive high-signal intensity on T2-weighted imaging (DEHSI). One newborn with a mild form of tricuspid valve dysplasia but with hydrops and polycystic kidney disease had severe white matter injury.
Table 6. Brain MRI in patients with fetal diagnosis of Ebstein anomaly and tricuspid valve dysplasia
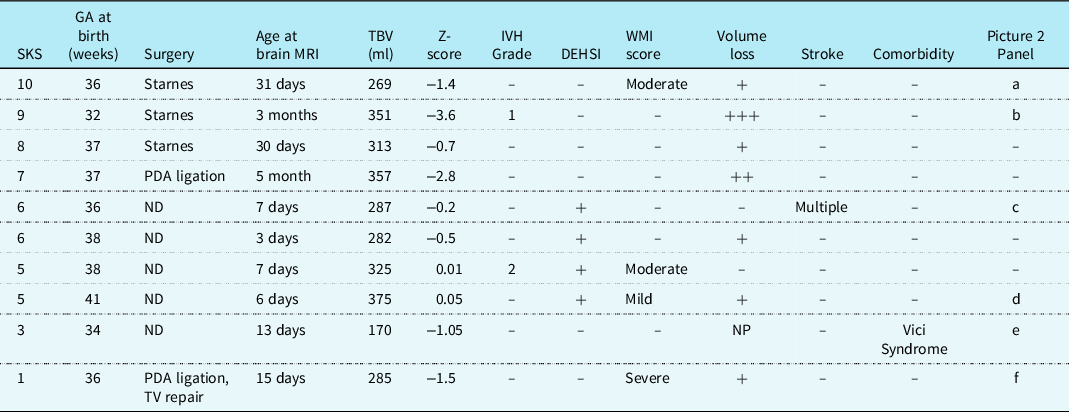
DEHSI: Diffuse Excessive High Signal Intensity; GA: Gestational Age; IVH: Intra Ventricular Hemorrhages; ND: Not Done; NP: Not Pertinent; PDA: Patent Ductus Arteriosus; SKS: SickKids Score; TBV: total brain volume; TV: Tricuspid Valve; WMI: white matter injury.
Mid-term neurodevelopmental outcomes
All surviving patients of the surgical group (6/6) underwent neurodevelopmental evaluation using the Bayley Scales of Infant Development-3rd edition at 18 months of age and scored lower than normal controls across all domains (Table 7). Mean percentiles for cognitive and language skills in Ebstein anomaly/tricuspid valve dysplasia patients were 11th (range 9th−16th) and 11th (range 4th−18th), respectively. Gross motor skills (mean percentile: 4th, range 1st−5th) were more affected than fine motor skills (mean percentile: 34th, range 16th−50th). At a mean follow-up of 4 years (SD 0.8, range 1−6), the five remaining patients surviving a Starnes operation have global neurodevelopmental delay, complementary nutrition by gastrostomy tube and are followed by a dietician, a speech language therapist, an occupational therapist, and a physiotherapist. Neurodevelopmental outcome data was available for 8 of the 17 surviving infants (47%) only because neurodevelopmental follow-up was not a routine component of care for patients in the medical group. However, two newborns were followed in our neurodevelopmental clinic because of their pre-discharge brain MRI findings. Despite the finding of multiple foci of haemorrhagic stroke at birth, one patient had a normal 12-month clinical examination and normal 36-month Bayley scores (Fig 7). The second patient had a Grade-2 intraventricular haemorrhage, diffuse excessive high signal on T2-weighted imaging, and moderate white matter injury on neonatal brain MRI (Fig 7). This patient obtained a very low score on the Bayley at 18 months and is now followed for an autism-related disorder and fine-motor skills delay.

Figure 7. Neonatal brain MRI. (a) T1-hypertense injury in the right frontal white matter (left picture) and scattered punctate foci of susceptibility in the left cerebellar lobe (right picture). (b) Severe loss of white matter with ventricular dilation (TBV z-score −3.6). (c) Multifocal ischaemic lesions with intraparenchymal haemorrhage suggestive of cortical venous infarcts. (d) Mild bifrontal-bitemporal volume loss with prominent extra-axial spaces and diffuse mild increase in T2-signal intensity of the deep white matter (DEHSI). A few bilateral posterior periventricular T2-hypointense punctate white matter foci and Grade-2 IVHD. (e) Extensive sulcation and gyration malformations with polymicrogyria in the bilateral peri-Sylvian regions. Complete agenesis of the corpus callosum, abnormal configuration of the brainstem with cerebellar and vermian hypoplasia. (f) Multiple bilateral and scattered areas of T1-hyperintensity in the periventricular white matter. (g) Small focus of T2-hyperintensity, enlarged ventricles and thinning of the corpus callosum in a 3-year-old patient before the total cavopulmonary connection.
Table 7. Mid-term neurodevelopmental outcome in survivors with Ebstein anomaly and tricuspid valve dysplasia

EA: Ebstein anomaly; SKS: SickKids Score; TVD: tricuspid valve dysplasia. * In this patient the tests were conducted in English, which was neither the primary languages spoken at home and the second language spoken at the day care.
Discussion
Our contemporary cohort of children with Ebstein anomaly and tricuspid valve dysplasia confirms prior reports Reference Freud, Escobar-Diaz and Kalish2–Reference Torigoe, Mawad and Seed4 of improved overall survival, reaching 57% (17/30) of prenatal diagnosed patients that were actively managed. Remarkably, even preterm fetuses born at 32 gestational week + 4 days and 36 gestational week affected by severe forms of Ebstein anomaly and tricuspid valve dysplasia involving circular shunt and hydrops survived into early childhood. This was probably achieved as a result of multiple interventions including transplacental therapy with indomethacin, optimised timing and mode of delivery in a setting predisposed and ready for immediate neonatal resuscitation and surgery, early Starnes procedure as the first surgical option and systematic use of ECMO. When fetuses with similarly severe forms were managed in-utero or when the Starnes procedure was delayed or when surgeries and/or interventions other than Starnes were preferred, survival was compromised. It is interesting to note that in severe forms of Ebstein anomaly and tricuspid valve dysplasia not complicated by other associated malformations, all in-utero deaths occurred after 33 gestational week. Although decision-making about the optimal timing of delivery in fetuses with critical Ebstein anomaly or tricuspid valve dysplasia will always be challenging and managed on a case-by-case basis, this observation raises the possibility that at around 33 gestational week it might be possible to achieve survival by delivering the fetus when there are signs of impending fetal demise such as the development of hydrops.
We note that interventional or hybrid strategies that aimed to encourage a biventricular circulation in two newborns with no antegrade flow across the pulmonary valve were unsuccessful. Conversely, even when the Starnes Procedure was performed in preterms, there was no peri-operative mortality. The remaining deaths were related to the patients’ fragility in the later follow-up period more than to the surgical decision-making and early post-operative period, occurring because of BT shunt or intra-stent thrombosis and bronchiolitis following discharge from the hospital. Although definitive conclusions are not possible with our sample size, it is worth noting that the SickKids Score correlated well with surgical management after birth. With the exception of the fetus whose hydrops likely had more to do with his polycystic kidney disease than his mild tricuspid valve dysplasia, the SickKids Score was >5 in all fetuses requiring surgery at birth. Newborns undergoing a Starnes procedure had prenatal SickKids Score of 7 or more. Among the five fetuses with a final SickKids Score of 7, those with Ebstein anomaly underwent a Starnes procedure, one with tricuspid valve dysplasia showing some anterograde pulmonary flow at birth tolerated closure of the patent ductus arteriosus well. Conversely, one patient with anatomic pulmonary valve atresia would have required a single ventricle pathway. Thus, a SickKids Score of 7 might represent a borderline value, associated with different postnatal outcomes when obtained in fetuses with Ebstein anomaly or tricuspid valve dysplasia, being highly dependent on the anatomy of the pulmonary valve and on the presence of spontaneous pulmonary anterograde flow after birth.
Brain MRI findings
Brain MRI at birth was abnormal in all surviving infants, even in those who did not require neonatal surgery. None of the infants had early clinical signs to suggest brain injury, except for one neonate with severe white matter injury who demonstrated axial hypotonia with limb hypertonia. The high incidence of brain injuries suggests that systematic brain MRI and neurodevelopmental follow-up are warranted in this population as clinical signs of brain injury are lacking in infancy and become apparent only over time. Reference Lim, Kingdom and Saini13 Early detection of brain injuries followed by timely remedial therapy are likely to improve their neurodevelopmental outcome. Reference McCusker, Doherty and Molloy14 In keeping with previous studies showing that stroke in neonates with CHD does not predict adverse outcome, a patient found to have multi-focal haemorrhagic strokes before discharge scored within the normal range at 36 months Bayley. Reference Peyvandi, Chau and Guo15
An additional newborn amongst those in the medically treated group had Grade 2 intraventricular haemorrhage and moderate WMI at birth and ultimately developed an autism-related disorder. Nevertheless, the causal relationship of these injuries with the clinical symptoms is difficult to prove.
Many studies have shown that newborns with CHD have smaller total brain volume than normal controls. Reference Lim, Porayette and Marini12,Reference Lim, Kingdom and Saini13 Our data would suggest that newborns with Ebstein anomaly and tricuspid valve dysplasia probably have smaller total brain volume than all other forms of CHD. Despite not reaching statistical significance, it is interesting to note that, excluding the only newborn with a congenital cerebral malformation, total brain weight z-score at birth was in keeping with the severity of the CHD assessed prenatally and with the surgical outcome. Reference Owen, Shevell and Donofrio16 Amongst the predictors of neurodevelopmental delay in patients with CHD, in-hospital length of stay is one of the strongest. In keeping with this observation, the two patients who had a late brain MRI because of a complex and long postoperative course, complicated by hypoxia, chylothorax, circular shunt and prematurity had the smallest brain sizes. Given the findings of previous studies linking brain size to neurodevelopmental outcome in adolescents after neonatal surgery for CHD, these patients are likely to require intensive rehabilitative interventions to maximise their individual potentials. Reference von Rhein, Buchmann and Hagmann17
Prenatal pathophysiology and the impact on neurodevelopmental outcomes
We used fetal cardiovascular magnetic resonance technology to investigate the haemodynamic patterns of fetuses with Ebstein anomaly and tricuspid valve dysplasia, quantifying flow and DO2 and VO2 and demonstrating reductions in umbilical vein, combined ventricular output, superior caval vein, and descending aorta flows and systemic arterial and venous oxygen saturations compared with normal controls. These measurements account for the reduced mean fetal DO2 and VO2 and for the reduced mean cerebral DO2 and VO2 in fetuses with these malformations. Meanwhile, ascending aorta flow is higher than in normal controls, serving to provide retrograde flow through the arterial duct in the case of functional or anatomic pulmonary atresia.
In addition, we noted a specific haemodynamic pattern in fetuses with circular shunts. Due to the retrograde loop, ascending aorta flow in Ebstein anomaly and tricuspid valve dysplasia with circular shunt tends to be higher than in fetuses without circular shunt, explaining the paradoxically higher combined ventricular output in these patients, despite their more severe clinical course. In patients with circular shunt, superior caval vien flow tends to be reduced and superior caval vien/combined ventricular output ratio is significantly lower than in Ebstein anomaly and tricuspid valve dysplasia fetuses without circular shunt. The increased cardiac output therefore fails to improve brain perfusion. In parallel, fetal brain size also tends to be smaller. We speculate that this might be the result of a retrograde carotid steal via the arterial duct and the regurgitant pulmonary valve, and proof of failure of cerebral autoregulation. Furthermore, the significantly lower descending aorta/combined ventricular output ratio confirms the deficit in systemic perfusion in Ebstein anomaly and tricuspid valve dysplasia fetuses with circular shunt.
Interestingly mean combined ventricular output, superior caval vien, descending aorta flow, and fetal total brain weight z-score correlate with surgical outcome. The lowest flows and z-score are measured in those fetuses undergoing the more extreme form of palliation at birth, the Starnes procedure. Fetal flows and total brain weight z-scores are higher in more moderate forms Ebstein anomaly and tricuspid valve dysplasia requiring interventions and other surgeries and are similar to normal controls in milder forms of disease that can be managed medically. In fetuses with circular shunt and in those requiring a Starnes procedure at birth, low descending aorta flow and thus low abdominal perfusion may be linked to an increased risk of necrotising enterocolitis and the severe failure to thrive associated with this pathophysiology. Reference Mukherjee, Zhang, Chang, Vricella, Brenner and Abdullah18 The direct relationship between systemic perfusion and brain size is confirmed by the significant correlation we observed between fetal superior caval vien and descending aorta flows and total brain weight z-score.
Our findings highlight how neurodevelopmental outcome is related to the severity of the haemodynamic impairment in patients with Ebstein anomaly and tricuspid valve dysplasia. Severe forms of these malformations have lower fetal superior caval vien flow and smaller fetal total brain volume, and smaller brain size at birth. Prolonged hospitalisation, hypoxia and low cardiac output in single ventricle patients may also play an additional role in the ongoing pathogenesis of global developmental delay. Not surprisingly, all of the patients surviving a Starnes procedure had low body weight and height gain despite being provided with additional nutritional intake via gastrostomy tubes and scored low on 18 month Bayley Scales. Gross motor skills seem to be the most impaired on the early assessments, as typically seen in other CHD patients at this age. Reference Martin, De Villiers Jonker and Joffe19 However, further follow-up will be necessary to verify if at least partial recovery will occur, as frequently seen after the total cavopulmonary connection completion. Unfortunately, we have limited data on neurodevelopmental follow-up in Ebstein anomaly and tricuspid valve dysplasia undergoing other strategies such as biventricular repair and 1.5 ventricle palliation. However, we have shown that even these mild or moderate forms of these malformations have a high incidence of brain injuries. In addition, these patients may also have chronically low cardiac output and persistent cyanosis because of their interatrial right-to-left shunts. In one newborn with multiple white matter injury and truncal hypertonia, early screening and therapy were effective in normalising neurodevelopment. Therefore, it is reasonable to speculate that all these less severe forms might benefit from systematic neurodevelopmental follow-up.
Limitations
A limitation of this study is the small sample size, which is the result of the relatively rare incidence of Ebstein anomaly and tricuspid valve dysplasia, and the relatively high rate of termination of pregnancy and fetal demise. Unfortunately, not all the fetuses included in our study underwent fetal cardiovascular magnetic resonance, and similarly not all surviving newborns had a brain MRI before discharge or a neurodevelopmental assessment.
Conclusions
In summary, in this study, we were able to link third trimester fetal brain volume and cardiovascular pathophysiology with postnatal brain size, surgical management, and with midterm neurodevelopmental outcome. As a result of innovations in perinatal and surgical management, patients with more severe forms of Ebstein anomaly and tricuspid valve dysplasia are more likely to survive. Brain MRI was abnormal even in moderate forms of these diseases. Close cardiac and neurodevelopmental follow-up is important in this fragile population, even in those newborns who do not require surgery or intervention at birth. We suggest these patients would benefit from systematic neurodevelopmental assessments, allowing early recognition of deficits and appropriate intervention that would optimise the chances of improving neurodevelopmental status and quality of life. Children surviving fetal circular shunt and neonatal Starnes procedure are all likely to require multiple rehabilitation services. Finally, fetal cardiovascular magnetic resonance demonstrated specific fetal haemodynamic patterns and linked fetal cardiac failure to impaired brain growth. Our data suggest the need for a larger multi-centre study to evaluate the utility of combined fetal cardiovascular and neonatal brain MRI to predict surgical and neurodevelopmental outcomes.
Acknowledgements
We thank Nathalie Dutil and Sonila Moustafa for the administration, Vanna Kazazian and Amandeep Saini for the coordinate with the neonatal brain MRI scan and neurodevelopmental follow-up.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national guidelines on human experimentation (Impact of cardiovascular haemodynamics on surgical and neurodevelopment outcomes in fetuses with Ebstein Anomaly and Tricuspid Valve Dysplasia, REB# 1000069782) and with the Helsinki Declaration of 1975, as revised in 2008, and has been approved by the institutional committees (The Hospital for Sick Children Research Ethics Board).

















