We read Kulik et al’s article on “Pressure injury prevention for paediatric cardiac surgical patients using a standardized clinical tool” with interest.Reference Kulik, Connor, Graham and Hickey 1 They have highlighted the significant variation in pressure injury susceptibility that exists between hospital units, thereby emphasising the importance of integrating a dedicated evidence-based guideline into a nurse-driven pressure injury prevention programme in children with CHD. Our pressure injury management strategy aligns with this principle and has been recently implemented in our mixed tertiary paediatric ICU.
Critically ill children admitted to the paediatric ICU are at high risk for developing pressure injuries. Of the three pressure injury risk assessment scales validated in the paediatric intensive care setting,Reference Gray 2 , Reference Kottner, Hauss, Schlüer and Dassen 3 the Glamorgan Pressure Ulcer Risk Assessment Scale is the only tool developed specifically for the paediatric population.Reference Willock, Baharestani and Anthony 4 However, pressure injury risk assessment scales are used universally in hospitals and do not adjust for acuity of illness.
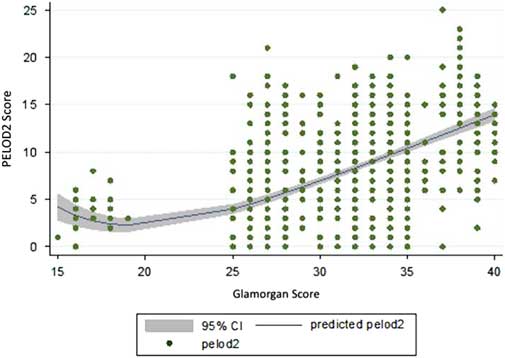
Our paediatric ICU has recorded higher internal numbers of pressure injuries than other areas of our hospital. The significant financial penalty attracted by each pressure injury, together with a clear need for review of our clinical practice, prompted this study. As part of a quality improvement initiative, we studied predictors for identifying patients at high risk of pressure injury and implemented measures to prevent the occurrence of pressure injuries. Pressure injury incidence data were obtained from the Queensland Children's Hospital Paediatric ICU pressure injury audit for the period between 1 July, 2017 and 31 December, 2017. This database includes both general and cardiac patients. Glamorgan and Paediatric Logistic Organ Dysfunction-2 scoresReference Leteurtre, Martinot and Duhamel 5 correlation values were obtained from Metavision, the electronic medical record system used in our paediatric ICU. The statistical program “R” was used to analyse these data. A nonlinear regression line was used to best display the correlation between Glamorgan and Paediatric Logistic Organ Dysfunction-2 scores. For the 98 pressure injuries recorded, we demonstrated a positive correlation between the two scores (Fig 1).
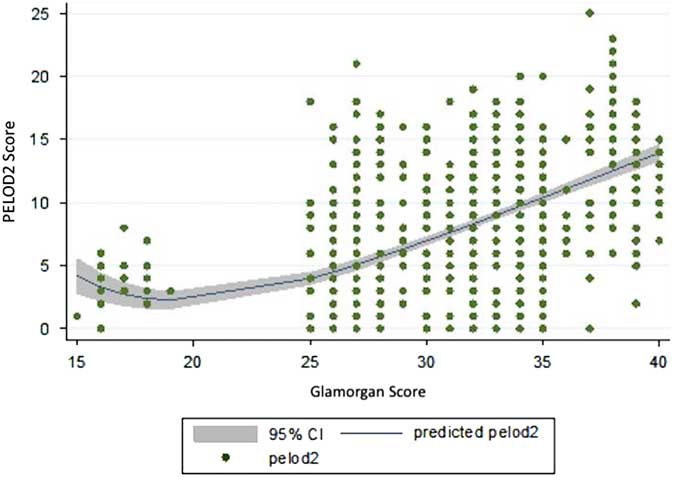
Figure 1 Correlation of daily Glamorgan and Paediatric Logistic Organ Dysfunction-2 (PELOD-2) scores for 98 pressure injuries recorded in 48 paediatric ICU patients between July and December 2017. The blue line shows the predicted PELOD-2, whereas the grey area represents the 95% confidence interval.
As pressure injury risk assessment scales are not suitable for universal use across all hospital departments, we propose that a modification of the Glamorgan risk assessment scale could provide a more representative comparison across hospital departments. Furthermore, incorporation of the Paediatric Logistic Organ Dysfunction-2 score may improve the predictive value of a modified Glamorgan scoring system. Whilst we develop such a scale, our new institutional pressure injury prevention bundle focusses on children with higher Paediatric Logistic Organ Dysfunction-2 scores, addressing both preventative strategies and emphasising early detection. We envisage that, in time, a paediatric ICU dedicated pressure injury scoring system will enable better patient care and objective data-driven policy decisions.
Acknowledgements
Andrew Barlow, Senior Data Manager.
Financial Support
This research received no specific grant from any funding agency, or from commercial or not-for-profit sectors.
Conflicts of Interest
None.