Introduction
Prolonged procedure times associated with adverse patient outcomes have been widely explored in the surgical literature. Reference Cheng, Clymer and Chen1,Reference Jackson, Wannares and Lancaster2 Adverse outcomes have been attributed to time under anaesthesia, time exposed to possible infection, the operator’s technical abilities, or procedure complexity. However, there is very little literature on procedure times in congenital cardiac catheterization, Reference Bergersen, Gauvreau and Jenkins3–Reference Yeh, Lydon and Gauvreau5 despite multiple registries devoted to risk factors and patient outcomes for this population. Reference Nykanen, Forbes and Du6–Reference Vincent, Moore and Beekman8 Particularly with the growing number of transcatheter interventions, a more sophisticated understanding of typical case lengths for different case types can be beneficial for comparative reporting and scheduling purposes. In addition, limited data available on case length and adverse events in congenital cardiac catheterization show that longer case lengths are associated with higher adverse event rates. Reference Bergersen, Gauvreau and Jenkins3,Reference Yeh, Lydon and Gauvreau5
Using data from a large multicentre registry, the Congenital Cardiac Catheterization Project on Outcomes, this study reports case lengths for congenital cardiac catheterization case types and defines Expected Case Length groups as a comparison tool. The primary aim of this study is to investigate patient and procedure characteristics associated with longer than anticipated case length and explore whether longer than anticipated case length is associated with adverse events.
Materials and methods
Patient population and study design
This is a retrospective analysis of data captured prospectively for all diagnostic and interventional congenital cardiac catheterizations at participating Congenital Cardiac Catheterization Project on Outcomes institutions from 1 January 2014 to 31 December 2017. Cases with procedure duration <5 min or >420 min were excluded. Institutional Review Board approval for this study was obtained at Boston Children’s Hospital and participating institutions in accordance with local requirements. Data were independently audited using methods previously described. Reference Quinn, Yeh and Gauvreau9
Patient and procedure characteristics
Characteristics collected included known risk factors for adverse events in congenital cardiac catheterization. Patient characteristics include age at procedure, sex, single- or bi-ventricle functional circulation, presence of any genetic syndrome, and presence of any non-cardiac problem. Patient haemodynamics were reported as normal or abnormal based on established thresholds and assigned a weighted haemodynamic vulnerability score Reference Quinn, Yeh and Gauvreau9 (Supplemental Table S1). Cases were classified as diagnostic or interventional. Interventional case types were determined by procedures performed. Reference Quinn, Yeh and Gauvreau9
Case length
Procedure duration was defined as minutes from sheath-in to sheath-out. The time needed to manage an adverse event during the time from sheath-in to sheath-out was determined by the operator and entered into the database in minutes. Case length was defined as procedure duration minus time needed to manage an adverse event. As a measure of efficient use of in-lab time, total fluoroscopy time in minutes was collected and used to calculate the ratio of fluoroscopy time to procedure duration.
Adverse events
If an adverse event occurred during or as a result of the catheterization procedure, the adverse event type, severity (Level 3–5) as defined by the International Paediatric and Congenital Cardiac Code, and description of the event were recorded. Reference Bergersen, Giroud and Jacobs10 The primary outcome was the occurrence of any life-threatening event (Level 4/5) (Supplemental Table S2), with a secondary outcome of any clinically significant adverse event (Level 3bc/4/5). Reference Quinn, Gunnelson and Kotin11
Analyses
Case length was summarized for individual case types using the 50th, 75th, and 90th percentiles. For interventional procedures, case types were placed into four Expected Case Length groups based on the median length of each interventional procedure type (Table 1). Case lengths were then summarized for diagnostic versus interventional procedures and for each Expected Case Length group.
Table 1. Expected Case Length groups and median case length by PREDIC3T case type

Case type could not be assigned for 12 cases. Case length is defined as procedure duration minus time spent managing adverse events. PDA = patent ductus arteriosus; ASD = atrial septal defect; PFO = patent foramen ovale; RVOT = right ventricular outflow tract; VSD = ventricular septal defect; TPV = transcatheter pulmonary valve.
Patient and procedure characteristics were summarized for the cohort as a whole and stratified by procedures with case length ≤75th percentile for a given case type versus those with longer than anticipated case length, defined as >75th percentile. To investigate which characteristics were associated with longer than anticipated case length, categorical variables were summarized with frequencies and percentages and compared for cases with lengths ≤75th versus >75th percentile using the chi-square test. Continuous variables were summarized using medians and interquartile ranges and compared using the Wilcoxon rank sum test. Adverse event rates were compared between groups using Fisher’s exact test.
To determine whether case length was associated with the occurrence of adverse events, case length was added to a published risk adjustment model, CHARM II. Reference Quinn, Gunnelson and Kotin11 The multivariable model accounts for known patient and procedural risk factors for adverse events, including case type risk category (PREDIC3T), Reference Quinn, Yeh and Gauvreau9 haemodynamic vulnerability score, and patient age <30 days. Cases were categorized as ≤50th percentile of length for their specified case type, >50th and ≤75th percentile, >75th and ≤90th percentile, or >90th percentile. Cases with duration ≤50th percentile were used as the reference group. Separate models were fitted for the outcomes Level 3bc/4/5 adverse event and Level 4/5 adverse event. Odds ratios were estimated with 95% confidence intervals. The model was also run with the addition of cases ≤75th percentile and >75th percentile as a dichotomous variable. To determine the presence of an adverse relationship between very short case times and patient outcomes, cases <20th percentile were assessed and compared to cases from the 20th to 50th percentile.
Results
A total of 14,704 diagnostic and interventional congenital cardiac catheterization cases from 10 sites were recorded in the database from 1 January 2014 to 31 December 2017.
Case length groups
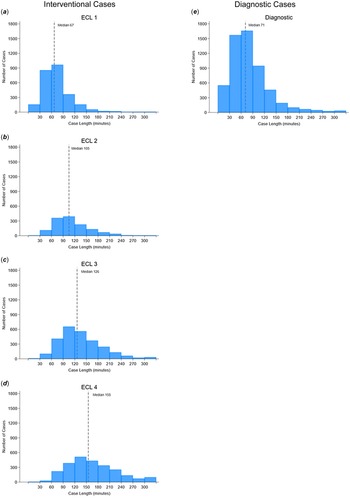
Median and 75th percentile case lengths by case type are reported in Table 1. Upon review, four groupings of case length emerged: <90 min, 90–119 min, 119–139 min, and ≥140 min (Table 1). Histograms of case length for diagnostic cases and each Expected Case Length group are included in Figure 1. The median case lengths were 67 minutes in Expected Case Length 1, 105 min in Expected Case Length 2, 126 min in Expected Case Length 3, and 155 min in Expected Case Length 4 (Fig. 2). Expected Case Length group 1Rev accounted for 89% of cases lasting 5–29 min, while Expected Case Length group 4 accounted for 57% of cases lasting at least 180 min (Fig. 2).
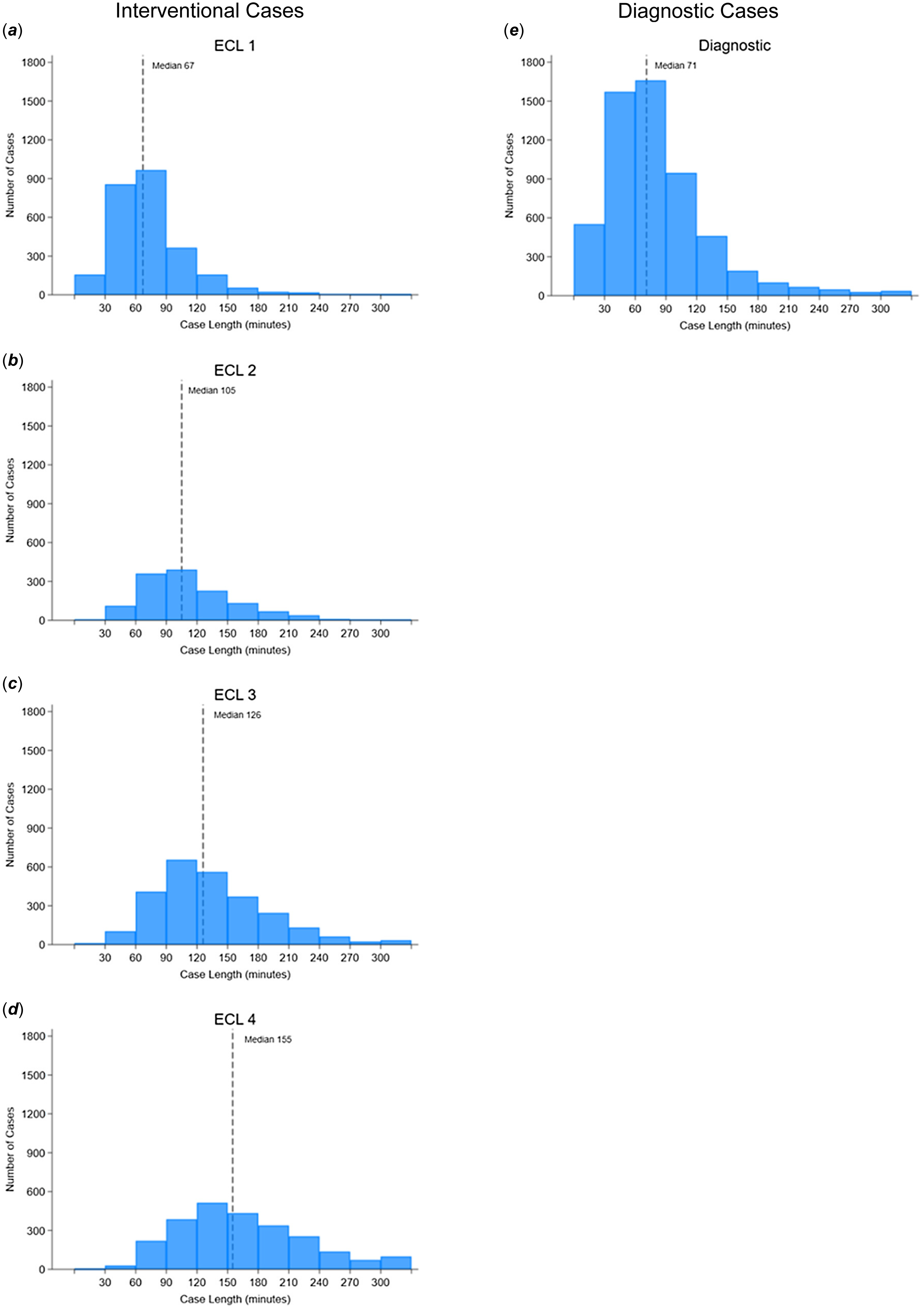
Figure 1. Case lengths for diagnostic cases and interventional cases by Expected Case Length (ECL) group.

Figure 2. Stacked histogram of percent of cases in each Expected Case Length group by case length with median, 25th and 75th percentile, and maximum case length for diagnostic and interventional cases and for each Expected Case Length group.
Patient and procedure characteristics
The median patient age for the cohort was 3 years, with a genetic syndrome reported in 10% of patients and a non-cardiac comorbidity present in 16% of patients (Table 2). Patients had single ventricle physiology in 26% of cases. Most patients (47%) had a haemodynamic vulnerability score of 0, and 65% were under general anaesthesia (n = 9596) (Table 2). The median procedure duration for the entire cohort was 93 min [IQR 62, 140]. Cases associated with Level 3 adverse events were a median of 10 min [5, 30] longer than cases without these events. Diagnostic and interventional cases associated with Level 4/5 adverse events were 30 min [10, 90] and 20 min [5, 60] longer, respectively, than procedures without these events.
Table 2. Patient and procedure characteristics
*Cut points at 75th percentiles of case length for each individual case type. AE = adverse event.
Diagnostic cases accounted for 5,660 cases and had a median case length of 71 min. There was no statistically significant difference in patient age, non-cardiac comorbidity, genetic syndrome, or recent cardiac procedure in cases shorter or longer than the 75th percentile for case length (Table 2). Patients with single ventricle physiology comprised 24% of shorter diagnostic procedures and 29% of longer cases. In addition, general anaesthesia was used in 57% (n = 2437) of the shorter cases compared to 71% (n = 983) of the longer cases. Patients had a haemodynamic vulnerability score of zero in 46% of shorter cases compared to 43% of longer cases, while a haemodynamic vulnerability score of ≥3 was present in 16% of shorter cases and 22% of longer cases (p < 0.001). The ratio of fluoroscopy time to procedure duration was 0.20 [0.13, 0.29] in shorter cases and 0.25 [0.14, 0.37] in longer cases (p < 0.001).
Interventions were performed in 9,044 cases, with a median patient age of 3 years and a median case length of 111 min. Cases with case length ≤75th percentile had a lower median age than cases >75th percentile (2 vs. 3 years, p < 0.001) (Table 2). Patients with non-cardiac comorbidities and/or genetic syndromes accounted for a larger percentage of the population in longer cases (Table 2). General anaesthesia was used in 67% of shorter cases compared to 73% of longer cases (p < 0.001). Additionally, 52% of shorter cases had a haemodynamic vulnerability score of 0 compared to 40% of longer cases (p < 0.001) (Table 2). Alternatively, 38% of longer cases had a haemodynamic vulnerability score of ≥2 compared to 26% of shorter cases (p ≤ 0.001). The ratio of fluoroscopy time to procedure duration was 0.25 [0.18, 0.36] in shorter cases and 0.30 [0.21, 0.42] in longer cases (p < 0.001).
Adverse event rates
The overall Level 3bc/4/5 adverse event rate for the cohort was 5.0%, with a 4/5 adverse event rate of 1.5% (Table 2). When comparing diagnostic cases shorter and longer than the 75th percentile, shorter cases had a 3bc/4/5 adverse event rate of 2.4% compared to 5.0% (p < 0.001). The Level 4/5 adverse event rate for diagnostic cases was 0.9% for shorter cases and 2.2% for longer cases (p < 0.001). Interventional cases >75th percentile also reported a higher 3bc/4/5 and 4/5 adverse event rate than shorter cases (5.4% vs. 8.4% and 1.4% vs. 2.7%, respectively, p < 0.001).
Multivariable model
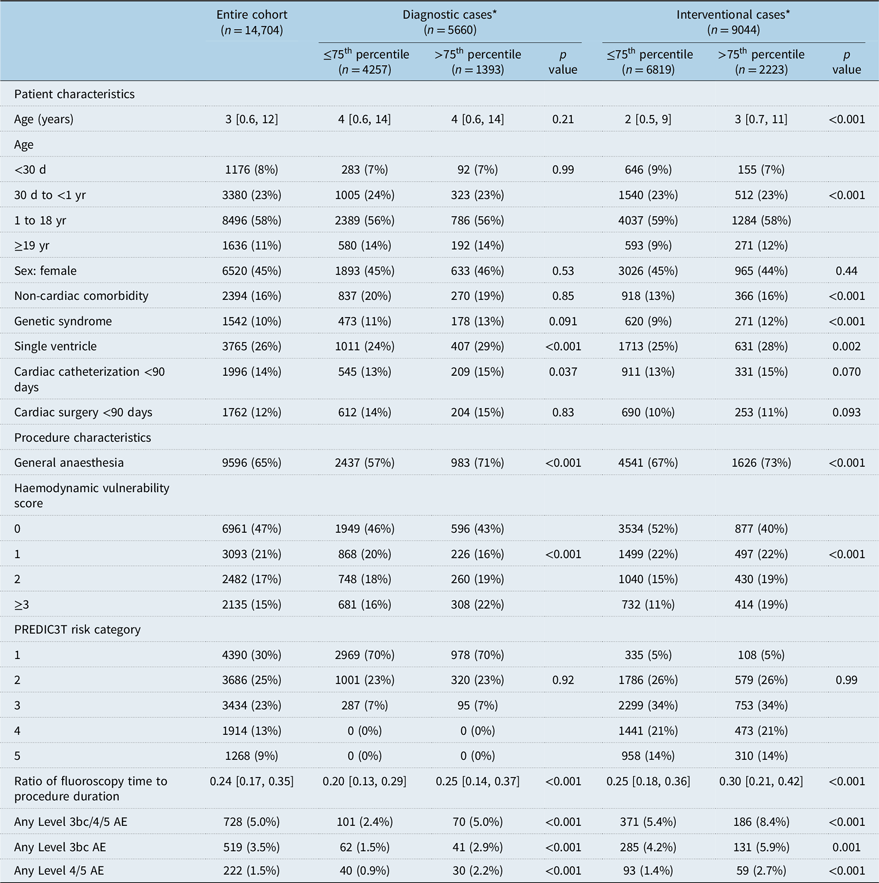
When the dichotomous variable of case length >75th percentile was added to the CHARM II multivariable model for adverse events (PREDIC3T risk category, haemodynamic vulnerability score, and patient age), case length was statistically significant, with an odds ratio of 1.60 [1.37, 1.88] for Level 3bc/4/5 adverse events and 1.97 [1.50, 2.60] for Level 4/5 adverse events (all p < 0.001). The CHARM II multivariable model for Level 3bc/4/5 adverse events, with the addition of cases categorized as 50th–−75th percentile, 75th–90th percentile, and >90th percentile, had odds ratios of 1.40 [1.16, 1.69], 1.56 [1.25, 1.94], and 2.24 [1.78, 2.81] with cases <50th percentile as the reference group (all p ≤ 0.001) (Table 3). When the model was run for the outcome Level 4/5 adverse event, the odds ratios were 1.57 and 2.76 for cases from 75th to 90th and >90th percentile for case length, respectively (p = 0.02, <0.001). When cases <50th percentile were broken into cases <20th percentile and 20th to 50th percentile, with the latter as the reference range, there was no statistically significant relationship between very short case times and adverse events.
Table 3. CHARM II adverse event risk model + case length
The CHARM II multivariable model is a risk adjustment model accounting for PREDIC3T case type risk category, haemodynamic vulnerability score, and patient age <30 days. Odds ratios are the independent contributions of each category for the outcome (3bc/4/5 adverse event or 4/5 adverse event).
Discussion
In this retrospective study of 14,704 cases from 10 sites over 4 years, we observed an association between case length and adverse events in congenital cardiac catheterization. After categorizing case types into groups of similar case lengths, we were able to create comparison groups. We then established the 75th percentile as the value over which case duration was considered long. Using this cut-off value, our study consistently demonstrated that longer case duration was significantly associated with a higher frequency of adverse events.
One single-centre study from 2008 found procedure duration categorized as <1 h, 1–2 h, 2–3 h, or >3 h to be statistically significantly related to adverse event rates when added to a multivariable model (p < 0.001). Reference Bergersen, Gauvreau and Jenkins3 The same centre also evaluated the impact of anaesthesia on cardiac catheterizations for pulmonary arterial hypertension and found that longer procedure duration was associated with adverse events in multivariable analysis (OR 1.3 per 30 min, p = 0.001). Reference Stein, Staffa and O’Brien Charles4 In a separate study, they found that cases with an adverse event had a 36 min longer median case length after adjusting for time spent managing adverse events than cases without an adverse event and identified a linear relationship between case length and log odds of an adverse event, with an OR of 1.08 for each additional 10 min of case length. Reference Yeh, Lydon and Gauvreau5 Those findings highlight the importance of an efficient procedure.
Our study consistently demonstrated that longer case duration was associated with a higher frequency of adverse events. To explore if this relationship was confounded by known risk factors, we adjusted for patient and procedure characteristics associated with increased risk of adverse events in previous work including age, procedure type, and haemodynamic vulnerability, and longer case times remained an independent risk factor for adverse event occurrence. To understand whether shorter case times, potentially related to hurrying through procedures, had a negative impact on patient outcomes, we looked at the relationship between cases <20th percentile and cases in the 20th–50th percentile and found no statistically significant relationship.
Case length is the result of many factors and is neither purely a cause nor an effect. Factors may include differences in individual interventionalist pacing or unusual or complex patient anatomy.
Some case types, such as pulmonary artery stenting, can vary widely in technical complexity and thus have a wide range of case lengths. Future quality improvement opportunities may include identifying aspects influencing case time, such as cath lab efficiency, which can be modified.
The longer a case goes on, the greater the opportunity for the patient to deteriorate from their baseline haemodynamic vulnerability for which previous risk adjustment methodology has not accounted. Case length helps account for the increased exposure risk as patients are exposed to general anaesthesia longer and are dependent on fluids and medications to maintain homeostasis. In addition, interventional complexities such as complex anatomical states during haemodynamic acquisition, catheter exchanges, flushing, and idling with catheters and wires in the heart while waiting for equipment increase patient vulnerability. While we have already accounted for case type in this study, for any given case type, there are additional factors that expose the patient to additional risk. For example, even in a diagnostic case, there can be significant variation. In comparison to a quick and simple diagnostic case, a complex diagnostic case may include complex anatomy making fluoroscopy and haemodynamic acquisition more difficult, pauses for review of angiograms, and further catheter manipulations and exchanges, which create opportunities for arrhythmias and trauma. Interventional cases include these same challenges, requiring pauses to re-evaluate the case, determine the next steps, and navigate anatomic complexity. In addition, interventional cases introduce additional risk exposure due to the technical components of interventions. Even in a straightforward case in a healthy patient for atrial septal defect closure, if the right equipment is not prepared in the lab, sending someone to get the equipment exposes the patient to a longer time under the sedated and manipulated environment.
Decreasing case length provides an opportunity for future local quality improvement work and is currently part of a Congenital Cardiac Catheterizations Project on Outcomes quality improvement initiative, which has shown initial positive results. The Expected Case Length groups can be used to provide a meaningful comparison of a centre’s case length, even for case types with fewer cases performed, while accounting for expected variation by interventions performed. Knowing the median case length for a given procedure type can assist in quality improvement projects to decrease case length, as it provides a goal length. When the median case time and/or 150% of the median time is reached, a brief team huddle can be conducted to assess progress in the case, challenges, and potential remediation strategies to complete the case safely and effectively. Of course, the advantage of this prescribed pause in the case must be weighed against the risk of prolonging case time, particularly when the procedure is flowing well and as planned. Balancing measures for improvement work related to case length may include the adverse event rate for cases <20th and in the 20th–50th percentile range, as rates may go up if interventionalists feel rushed. Similarly, rates of reintervention and measures of procedural efficacy may serve as important balancing measures to ensure that shorter cases do not eliminate parts of procedures. In an attempt to shorten case length, the efficacy can suffer. It is important to understand how to measure efficacy in order to use this as a balancing measure, and the Congenital Cardiac Catheterizations Project on Outcomes has been working to measure efficacy for particular procedures. Reference Hasan, Barry and Ali12 The overall efficacy and success of catheterization must take into account all aspects of the procedure, such as safety, technical success, establishing the correct diagnoses, trainee education, and myriad other factors.
Limitations
The Expected Case Length groups were derived based on the distributions of procedure duration without regard for operator or institution, assuming that these are the distributions of procedure duration across a diverse population of cases from multiple paediatric institutions. While we account for many types of multiple interventions in the Expected Case Length groups, we do not account for them all. For instance, a procedure with angioplasty of two pulmonary artery branches is grouped with a procedure with angioplasty of six pulmonary artery branches. The latter procedure would likely have a longer case length and inherently more risk because of the procedure being performed and not necessarily because of the case length itself. Sheath-in and sheath-out times are collected in the database, but in-lab time is not. Therefore, as part of this study, we did not explore the relationship of in-lab time, which would be a better estimate of total anaesthesia time. Furthermore, there was no way to account for time spent waiting for equipment after sheaths were inserted, extending patient time under anaesthesia. To account for this, we included the ratio of fluoroscopy time to procedure duration. Longer diagnostic-only cases had a lower ratio of fluoroscopy time to procedure duration than shorter diagnostic cases, potentially suggesting that longer diagnostic cases may have had a less efficient use of in-lab time. However, longer interventional cases had a higher ratio of fluoroscopy time to procedure duration. While this ratio did not appear to be a useful surrogate for lab efficiency, further investigation is required to identify metrics of efficiency related to case length. Lastly, we did not measure procedural efficacy or reintervention rates in these cases. Those are important outcome measures that will need to be studied in the future.
Conclusion
Case length >75th percentile is independently associated with a higher risk for serious adverse events, even when adjusted for other risk factors in a multivariable model. Quality improvement projects targeting improvement in case duration may reduce the overall adverse events and help improve patient outcomes, but a decrease in case length must be carefully balanced with procedural efficacy so that overall success does not suffer.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1047951124036606.
Acknowledgements
The authors would like to thank the Congenital Cardiac Catheterization Project on Outcomes Research and Publications Committee for their support and guidance for this project.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Competing interests
The authors declare none.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the US Federal Policy for the Protection of Human Subjects (“Common Rule”) and with the Helsinki Declaration of 1975, as revised in 2008, and has been approved by the Boston Children’s Hospital Institutional Review Board.