Introduction
Global population aging has resulted in a prioritization of healthy aging policy, programming, and service provision for older adults. It is projected that by the year 2050, one in four people will be over the age of 60 years (World Health Organization, 2018). Parallel to this demographic shift is a health care system shift that is emphasizing aging-in-place – a strategy aimed at keeping individuals in their homes and communities longer. In order to best support these community-dwelling older adults, however, there is a need to fully comprehend how they understand and define health.
Self-reported health, also described as self-rated health or self-assessed health, is an individual appraisal of health status based upon individual perspectives (Banerjee, Perry, Tran, & Arafat, Reference Banerjee, Perry, Tran and Arafat2010; Jylhä, Reference Jylhä2009; Knaüper & Turner, Reference Knaüper and Turner2003). Self-reported health, a widely used measure in both health and epidemiological research, has been found to be a highly predictive measure of both morbidity and mortality and is typically inexpensive to administer (Banerjee et al., Reference Banerjee, Perry, Tran and Arafat2010; Idler & Benyamini, Reference Idler and Benyamini1997; Jylhä, Reference Jylhä2009). Within older adult populations, various factors – including economic status, sex, participation in physical activities, and the presence of certain chronic conditions – have been found to be associated with self-reported health (Dowd & Zajacova, Reference Dowd and Zajacova2007; Vuorisalmi, Lintonen, & Jylhä, Reference Vuorisalmi, Lintonen and Jylhä2005). Nonetheless, despite this broad evidence base, there has not been a review that has synthesized these wide-ranging factors among community-dwelling older adults. As self-reported health is a widely used measure to assess health status, there is a need to understand the current state of the literature and the opportunities for future study on this topic – especially as it concerns a growing population that is aging in place.
Purpose
By addressing these gaps in the literature, the scoping review serves as a form of knowledge synthesis that maps key concepts, evidence types, and knowledge gaps in research related to a specific and defined area (Colquhoun et al., Reference Colquhoun, Levac, O’Brien, Straus, Tricco, Perrier and Moher2014; Levac, Colquhoun, & O’Brien, Reference Levac, Colquhoun and O’Brien2010). The scoping review provides a broad overview of the literature through systematic searching and synthesis of existing evidence (Colquhoun et al., Reference Colquhoun, Levac, O’Brien, Straus, Tricco, Perrier and Moher2014). We selected the scoping review methodology for this study as it will provide an opportunity to summarize the evidence, identify research gaps, and make recommendations for future research related to factors associated with self-reported health among community-dwelling older adult populations and how these factors influence it. The aims of our review were (a) to systematically scope the literature related to factors that are associated with self-reported health among community-dwelling older adults; and (b) to identify key areas for future research.
Methodology
This scoping review followed the stage-wise framework developed by Arksey and O’Malley (Reference Arksey and O’Malley2005). This included (a) identifying the research question; (b) identifying relevant studies; (c) selecting studies for review; (d) charting the data; and (e) collating, summarizing, and reporting the results. The findings of this review are reported in accordance with the PRISMA-ScR guidelines (Tricco et al., Reference Tricco, Lillie, Zarin, O’Brien, Colquhoun, Levac and Straus2018).
Identifying the Research Question
To meet the objectives of this review, we developed two exploratory research questions: (a) What factors are associated with self-reported health among community-dwelling older adults? and (b) What opportunities for future research exist, including other methodologies or designs?
For this review, community-dwelling older adults are those older adults, aged 60 and older, who reside in any setting, exclusive of institutional (e.g., long-term care home) or hospital settings. These settings may include retirement living or transitional care facilities.
Identifying Relevant Studies
Information Sources.
Relevant peer-reviewed studies were identified through a comprehensive search of the literature. This search included the following electronic databases: MEDLINE, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Web of Science, and AgeLine. Reference lists of all included articles were hand searched for relevant articles not identified through database searching.
Search Strategy.
We developed the search strategy and search terms in consultation with a health sciences librarian. Search terms included “older adult*” OR “senior” OR “elder*” and “self-report*” OR “self-rate*” OR “subjective health”. The search we conducted used combinations and synonyms of the core concept keywords, including “older adult” and “self-reported health”. We restricted the search to include only those articles published in the English language and publications between the years of 1975 and 2019.
Study Selection.
Titles and abstracts of all articles retrieved were screened for relevance by two independent reviewers. Research articles were selected for review if the study pertained to (a) a sample of community-dwelling adults aged 60 years and older, and (b) self-reported health as an exposure or a measure. We excluded articles from the review if the study (a) did not study self-reported health as an exposure or a measure, (b) did not pertain to a community-dwelling population of older adults, (c) was unclear regarding the population studied, and (d) was not written in the English language. For example, we excluded a study if it did not analyze self-reported health for association with other factor(s), or if the study included a population of adults aged 18 and older with no separate analysis of an older adult sub-group. Despite the literature commonly defining older adults as those aged 65 years and older, our review included a less restrictive age range (i.e., adults 60 and older) so as to include some key longitudinal studies on the topic. Full-text copies of relevant articles were retrieved according to study selection criteria.
Charting the Data.
Data from articles that met the inclusion criteria were extracted using a standardized data abstraction form created in Microsoft Excel. Data abstracted included author, year published, country, study aims, age range of the study participants, design and methods, definition of self-reported health, and key findings. Key findings included those factors (variables) associated with self-reported health, the nature of the association observed (e.g., whether the factor was associated with an increase or decrease in self-reported health), and any factors that were assessed but found not to have a statistically significant association with self-reported health. We identified key findings and themes from the extracted articles through numeric summary and qualitative thematic analysis.
Collating, Summarizing, and Reporting the Results.
From the database searches, we identified 431 articles. We used two stages of independent screening to identify articles that met study inclusion criteria (see Figure 1 for PRISMA-style study search procedure). An additional 22 articles were identified through hand-searching reference lists of full-text articles. After removing duplicates, we read 339 titles and abstracts and screened them for relevance, resulting in 88 papers eligible for full-text review. These articles were read in full and examined for their eligibility for inclusion. Following full-text review of the 88 articles, we deemed 30 articles eligible and included those in this scoping review.

Figure 1: Study search procedure
Geographic Locations.
This review included14 studies completed with North American populations (4 in Canada, 10 in the United States). The remaining studies were completed with populations from Europe, including Germany (n = 5), Albania (n = 1), Finland (n = 1), the Netherlands (n = 1), Poland (n = 1), Turkey (n = 1), and Slovenia, Lithuania, and the United Kingdom (n = 1); South America, including Brazil (n = 2), Colombia (n = 1); and Asia, including Japan (n = 3), China (n = 1), and Taiwan (n = 1). See Table 1 for study characteristics including the design, objective, and population.
Table 1: Study characteristics

Types of Evidence.
This scoping review included cross-sectional surveys (n = 24) and longitudinal designs (n = 6). There was no difference between the studies that used a cross-sectional design and those that used a longitudinal design with respect to the factors associated with self-reported health.
Description of Population.
Included studies were diverse in the populations studied (see Table 1). Characteristics of the study population included the presence of multiple chronic conditions (n = 3); living alone (n = 2); being married (n = 2). Several of the studies also had specific parameters for age ranges within the older adult population. These parameters of included studies were (a) individuals older than aged 60 years (n = 4); (b) those older than 65 years (n = 14); (c) those 75 years or older (n = 2); as well as (d) a handful of studies that further segmented the population (e.g., those aged 65–74 years or 60–84 years). One of the included studies included only a population of women while the other studies included both men and women.
Measuring Self-reported Health.
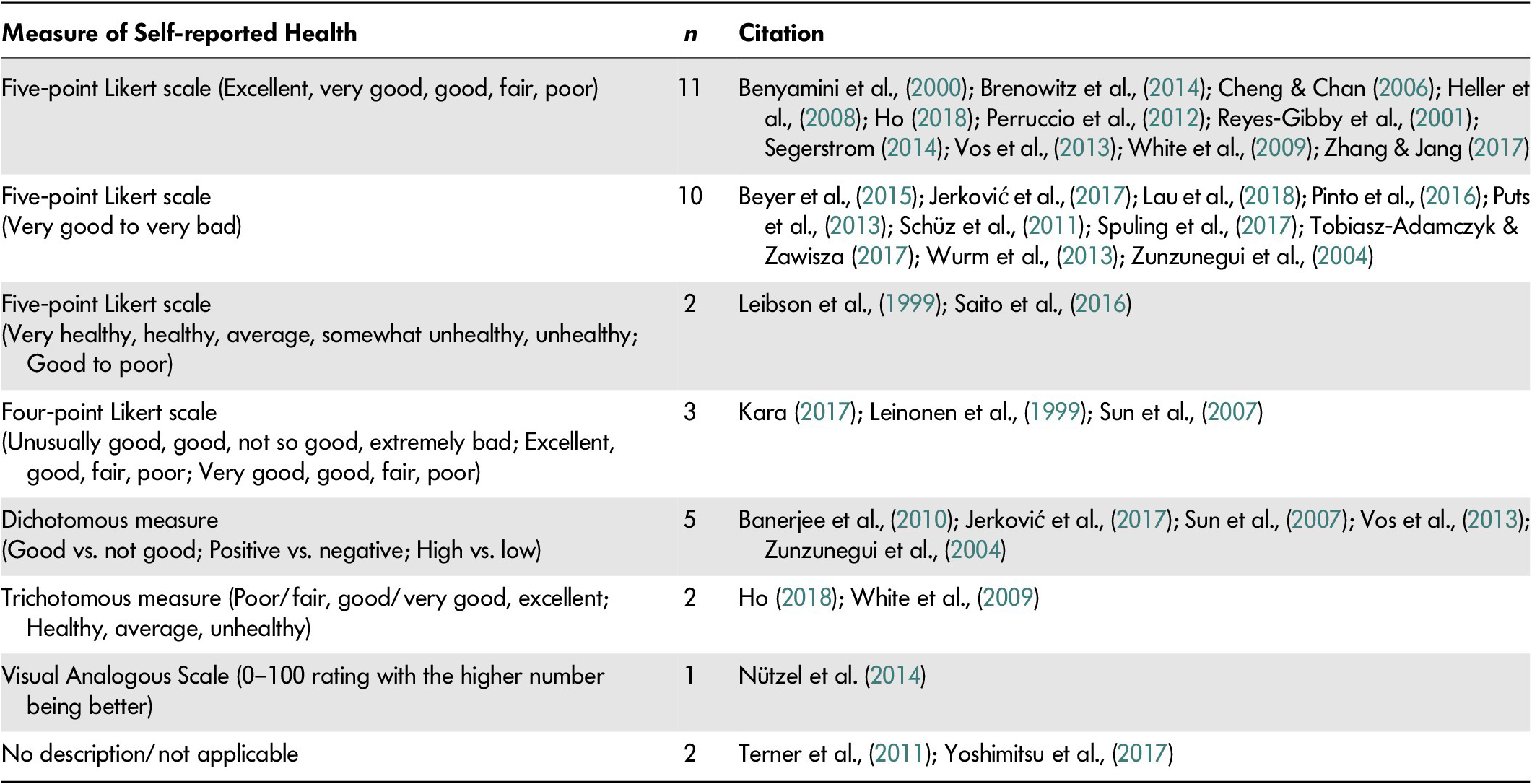
Among included studies, self-reported health, also described as self-rated health or subjective health, was measured in different ways (see Table 2 for measures of self-reported health). This included measurement on a 5-point Likert scale (n = 22) with most studies including anchors of “excellent” to “poor” (n = 11), “very good” to “very bad” (n = 10), or “very healthy” to “unhealthy” (n = 2), while others used 4-point scales (n = 3). Two of the studies included did not describe the way that self-reported health was measured. Further, some of the included studies, for analytical purposes, used a collapsed self-reported health measure that converted the original 5- or 4-point scales to dichotomous measures (n = 5) or trichotomous measures (n = 2). This meant that in some studies, “positive” or “good” self-reported health included original anchors of excellent, very good, and good, while “negative” or “low” health included anchors such as fair or poor health.
Table 2: Measures of self-reported health
Factors Associated with Self-reported Health
A total of 42 factors were identified as associated with self-reported health among community-dwelling older adults. The majority of these factors were measured using self-report (e.g., report on nutritional intake). These broad factors are grouped under the following four categories: sociodemographic variables; physical and psychiatric health; health-related behaviour; and emotional status (see Table 3 for a full description of the factors).
Table 3: Factors associated with self-reported health

+ associated with a higher self-reported health rating
– associated with a lower self-reported health rating
x no statistical significance with self-reported health rating
* longitudinal study design
Sociodemographic Factors.
Six sociodemographic factors were identified as associated with self-reported health among this population. With consistency, a higher level of education (n = 8); a higher economic status (n = 6); and White race (n = 2) were associated with higher self-reported health. There were also several sociodemographic factors that were reported in some studies to be associated with higher ratings of self-reported health (+) whereas in other studies were found to be associated with lower ratings of self-reported health (–). These factors included older age (+ n = 1; – n = 6); younger age (+ n = 1); identifying with the female sex (+ n = 2; – n = 5); and living alone because of divorce (– n = 1), being widowed (– n = 1), or being single (+ n = 2).
Physical and Psychiatric Health Factors.
Many of the included studies focused on the association between single chronic conditions or a combination of chronic conditions with self-reported health. A higher number of chronic conditions (n = 18) and declining functional status (n = 8) were consistently associated with lower levels of self-reported health. In addition, it was found that not just the number of chronic conditions, but also the presence of specific conditions that consistently were associated with lower self-reported health. These conditions included a higher number of depressive symptoms (n = 10), diabetes (n = 3), arthritis (n = 3), hypertension (n = 2), and stroke (n = 2). Other physical or psychiatric health factors, consistently found to be associated with lower levels of self-reported health, included an inability to perform activities of daily living (n = 4), the presence of a serious health event (n = 2), higher number of hospital or primary care visits (n = 2), weight loss (n = 2), and the presence of pain (n = 2).
Health-Related Behaviour Factors.
This third category of factors associated with self-rated health refers to those that describe health-related behaviours. These factors include those that relate to routines and habits (e.g., lifestyle, social determinants of health) (Riediger, Bombak, & Mudryj, Reference Riediger, Bombak and Mudryj2019). Seven health-related behaviour factors were identified. Engaging in regular exercise (n = 4), reporting social integration or participation (n = 7), and engaging with social networks (n = 5) were consistently associated with higher levels of self-reported health.
Emotional Factors.
This fourth and final category encompasses those factors related to emotional processes, personality, and context. Nine emotional factors were identified and were all consistently associated with higher levels of self-reported health: positive affect (n = 4), the presence of emotional support (n = 3), the presence of health-related control beliefs (n = 2), a high internal health locus of control (n = 2), absence of loneliness (n = 2), and increased positive perceptions of aging (n = 2).
Factors Not Associated with Self-reported Health.
In addition to synthesizing those factors that were found to be associated with self-reported health, factors that were reported to not have a statistically significant association were also identified from those studies that reported these findings. These factors, found to have no relationship with self-reported health, included HbA1c level (n = 1), nutrition (n = 2), waist circumference (n = 1), faith affiliation (n = 1), and smoking status (n = 2).
Summary of Findings
This review identified 42 individual factors encompassing sociodemographic, physical and psychiatric health, health-related behaviour, and emotional factors that were associated with self-reported health among community-dwelling older adults.
The factors associated with self-reported health that were most frequently cited (i.e., in the greatest number of included studies) across the included studies were as follows: age, level of education, the number of chronic conditions present, the presence of depressive symptoms, functional status, and the presence of social participation. This descriptive review contributes new understanding related to the state of the knowledge on the factors associated with self-reported health.
Discussion
The purpose of this scoping review was to summarize the factors associated with self-reported health among community-dwelling older adults, identify gaps in this literature base, and make recommendations for future research. We will further discuss each of these three points.
Key Factors Associated with Self-reported Health
In this scoping review, we identified 30 publications and summarized 42 individual factors associated with self-reported health among community-dwelling older adults. Although the review has highlighted a broad range of factors associated with self-reported health, it has also highlighted inconsistencies across studies. It is because of these inconsistencies that further research is required.
Of these broad factors, the number of chronic conditions reported (n = 18) and the presence of depressive symptoms (n = 10) were the two factors that we found most commonly identified as being associated with self-reported health in the included studies. However, although the direction of the association of these factors with self-reported health is known, causality cannot be claimed. This is because of the study design (e.g., observational, cross-sectional), and because few studies have explored the mechanism that links these factors with self-reported health.
Multimorbidity, Self-reported Health, and Community-dwelling Older Adults.
Multimorbidity, defined as the presence of two or more chronic conditions, is increasingly prevalent among older adults (Boyd & Fortin, Reference Boyd and Fortin2010; Markle-Reid et al., Reference Markle-Reid, Ploeg, Valaitis, Duggleby, Fisher, Fraser and Williams2018). As the population continues to age and life expectancy subsequently rises, health service use demand has also increased as a result of increasing multimorbidity (Canadian Institute for Health Information, 2011; World Health Organization, 2018). Until recently, single conditions were often studied in isolation. Following the recognition that older adults frequently experience a combination of chronic conditions, research on chronic conditions has refocused on multimorbidity to better understand the combined and cumulative effects of these multiple chronic conditions (Wister et al., Reference Wister, Coatta, Shcuurman, Lear, Rosin and MacKey2016). However, despite upwards of 30 per cent of older adults reporting the presence of multimorbidity (Canadian Institute for Health Information, 2011), and the presence of chronic conditions appearing as a factor associated with self-rated health in over half of the studies included in this review, there remains a need to understand how chronic conditions – and more specifically, how the presence of multimorbidity – influence self-reported health among older adults.
For example, multimorbidity was analyzed for its influence on self-reported health among older women in a study by Vos, Bor, van Rangelrooij-Minkels, Schellevis, and Lagro-Janssen (Reference Vos, Bor, van Rangelrooij-Minkels, Schellevis and Lagro-Janssen2013). In that research, combinations of the most common chronic conditions including arthritis, hypertension, diabetes, depression, and chronic pain were studied for their impact on self-reported health. Consistent with other studies in our review, the Vos et al. work found that ratings of low self-reported health were associated with older women with a greater number of chronic conditions (Vos et al., Reference Vos, Bor, van Rangelrooij-Minkels, Schellevis and Lagro-Janssen2013). In addition, these researchers highlighted that all combinations of chronic conditions that were significantly associated with lower levels of self-reported health involved the presence of either chronic back pain or chronic headache (Vos et al., Reference Vos, Bor, van Rangelrooij-Minkels, Schellevis and Lagro-Janssen2013). This finding highlights that, in addition to the presence of multimorbidity, underlying symptoms such as pain may be particularly important in understanding the connection between multimorbidity and self-reported health.
Our scoping review has highlighted the need to understand how multimorbidity as well as other factors such as advanced age, functional status, and social connectivity shape self-reported health among community-dwelling older adults.
Depressive Symptoms, Multimorbidity, and Self-reported Health.
One of the most frequently identified factors associated with self-reported health in our review was the presence of depressive symptoms among older adults. Although we found both depressive symptoms and multimorbidity to be independently associated with self-reported health, it is also understood that the risk for depressive symptoms is increased by the presence of multimorbidity (Harpole et al., Reference Harpole, Williams, Olsen, Stechuchak, Oddone, Callahan and Unützer2005; Wilson-Genderson, Heid, & Pruchno, Reference Wilson-Genderson, Heid and Pruchno2017). Moreover, the presence of both depressive symptoms and multimorbidity may have a synergistic impact (i.e., an effect that is greater than the sum of the individual effects) on self-reported health.
When considering the wide-reaching impact of depressive symptoms on somatization, social functioning, and activities of daily living (Bruce et al., Reference Bruce, McAvay, Raue, Brown, Meyers, Keohane and Weber2002), for example, it becomes difficult to disentangle what factors are potentially impacting health, physical or psychiatric conditions, or both. Knowing that upwards of 40 per cent of older adults report the presence of depressive symptoms (Bruce et al., Reference Bruce, McAvay, Raue, Brown, Meyers, Keohane and Weber2002; Gallegos-Carrillo et al., Reference Gallegos-Carrillo, Garcia-Pena, Mudgal, Romero, Duran-Arenas and Salmeron2009), and that depression is a frequently underdiagnosed and undertreated condition among this population (Bruce et al., Reference Bruce, McAvay, Raue, Brown, Meyers, Keohane and Weber2002; Markle-Reid et al., Reference Markle-Reid, McAiney, Forbes, Thabane, Gibson, Browne and Busing2014), future research is warranted to explore the ways in which depressive symptoms shape self-reported health among older adults and/or interact with multimorbidity in shaping self-reported health.
For example, in one study by Reyes-Gibby, Aday, and Cleeland (Reference Reyes-Gibby, Aday and Cleeland2001), older adults with depression were found to be twice as likely to report fair or poor self-reported health (73%) in comparison to those who did not report depression (31%). The association of depression and depressive symptoms to subjective health status, as highlighted in a meta-synthesis by Pinquart (Reference Pinquart2001), is likely related to (a) an increased risk for depression because of increasing physical illness in older age; (b) the physical symptoms that depression may exacerbate or produce, such as lack of energy, which can worsen health status and, likely, health ratings; and (c) the presence of negative affect and negative evaluation of the self which is a cognitive symptom of depression.
Identified Gaps in Literature.
Findings from our scoping review have highlighted that, to date, the literature related to self-reported health has mostly been exploratory. This exploratory nature of the literature has resulted in a fragmentary understanding of how, or the process by which, the identified factors shape self-reported health.
Identified by Lau, Guerra, de Souza Barbosa, and Phillips (Reference Lau, Guerra, de Souza Barbosa and Phillips2018), high resiliency – as measured using the Wagnild Resilience Scale (Wagnild & Young, Reference Wagnild and Young1993) – was associated with high levels of self-reported health. Resiliency, defined as a process of positive adaptation toward adversity, trauma, or stress (American Psychological Association, 2015) that draws upon dynamic personal characteristics (Masten, Reference Masten2007), has been linked to successful aging (Stewart, Auais, Bélanger, & Phillips, Reference Stewart, Auais, Bélanger and Phillips2018). Although there has been much study on resilience as an outcome measure, this study is one of the first of its kind to study resilience and its association with self-reported health among community-dwelling older adults (Lau et al., Reference Lau, Guerra, de Souza Barbosa and Phillips2018). This unique finding led Lau et al. (Reference Lau, Guerra, de Souza Barbosa and Phillips2018) to propose that resiliency may serve to increase the level of self-reported health (i.e., more positive self-reported health), and, in addition, may shape or be shaped by other factors that are fundamental to personal definitions of health.
Drawing upon the literature on resilience, a resilience index was developed by Wister et al. (Reference Wister, Lear, Schuurman, MacKey, Mitchell, Cosco and Fyffe2018). This resilience index maps functional (e.g., activities of daily living), psychological (e.g., depressive symptoms), and social variables (e.g., social support) to resiliency among older adults. The level of resilience, calculated using this index, as well as the individual variables that comprise this index may serve to shape self-reported health among community-dwelling older adults as it was found that total resilience is associated with perceived health status (Wister et al., Reference Wister, Lear, Schuurman, MacKey, Mitchell, Cosco and Fyffe2018).
There are further opportunities to explore the relationship between those factors the studies associated with both resilience as well as self-reported health. Although only one study in our review identified resilience as an associated factor, several of the factors identified in other studies, from each of the four categories, are factors commonly associated with resilience. For example, these commonalities include (a) sociodemographic factors such as age (Gooding, Hurst, Johnson, & Tarrier, Reference Gooding, Hurst, Johnson and Tarrier2011; Laird et al., Reference Laird, Lavretsky, Paholpak, Vlasova, Roman, St. Cyr and Siddarth2019), economic status (Wells, Reference Wells2009), education (Pietrzak & Cook, Reference Pietrzak R and Cook2013), ethnicity (Laird et al., Reference Laird, Lavretsky, Paholpak, Vlasova, Roman, St. Cyr and Siddarth2019), and sex (Hardy, Concato, & Gill, Reference Hardy, Concato and Gill2004); (b) physical and psychiatric health factors such as an ability to perform instrumental activities of daily living (Hardy et al., Reference Hardy, Concato and Gill2004), number of chronic conditions (Gooding et al., Reference Gooding, Hurst, Johnson and Tarrier2011; Laird et al., Reference Laird, Lavretsky, Paholpak, Vlasova, Roman, St. Cyr and Siddarth2019; Wells, Reference Wells2009), mental illness (Gooding et al., Reference Gooding, Hurst, Johnson and Tarrier2011; Pietrzak & Cook, Reference Pietrzak R and Cook2013; Wells, Reference Wells2009) including depressive symptoms (Hardy et al., Reference Hardy, Concato and Gill2004; Laird et al., Reference Laird, Lavretsky, Paholpak, Vlasova, Roman, St. Cyr and Siddarth2019), cognitive capacity (Laird et al., Reference Laird, Lavretsky, Paholpak, Vlasova, Roman, St. Cyr and Siddarth2019; Lamond et al., Reference Lamond, Depp, Allison, Langer, Reichstadt, Moore and Jeste2008), and physical health (Pietrzak & Cook, Reference Pietrzak R and Cook2013; Wells, Reference Wells2009); (c) behavioural factors such as social integration (Lamond et al., Reference Lamond, Depp, Allison, Langer, Reichstadt, Moore and Jeste2008; Pietrzak & Cook, Reference Pietrzak R and Cook2013) and social networks (Fuller-Iglesias, Sellars, & Antonucci, Reference Fuller-Iglesias, Sellars and Antonucci2008; Wells, Reference Wells2009); and (d) emotional factors like coping (Laird et al., Reference Laird, Lavretsky, Paholpak, Vlasova, Roman, St. Cyr and Siddarth2019; Lamond et al., Reference Lamond, Depp, Allison, Langer, Reichstadt, Moore and Jeste2008), locus of control (Lamond et al., Reference Lamond, Depp, Allison, Langer, Reichstadt, Moore and Jeste2008), and self-perceptions of aging (Lamond et al., Reference Lamond, Depp, Allison, Langer, Reichstadt, Moore and Jeste2008).
Beyond the identified associations, and considering the substantial development of the resilience literature and the alignment between factors associated with both resilience and self-reported health, there remains a gap in understanding related to how these factors may shape self-reported health and how this knowledge may in turn shape public policy or health and social interventions. With this knowledge there is the potential to improve health outcomes for this population.
Of the 42 factors we identified in this scoping review, 20 of them can be categorized as physical and psychiatric health condition factors. Considering this emphasis, and knowing that despite the challenges associated with multimorbidity and depressive symptoms among community-dwelling older adults, self-reported health is not always aligned with objective health status (Canadian Longitudinal Study on Aging, 2018; Wister et al., Reference Wister, Lear, Schuurman, MacKey, Mitchell, Cosco and Fyffe2018), there is a need to understand what is considered when community-dwelling older adults define and describe their health and how resilience may shape this process.
Future Opportunities
Identified in this scoping review literature were a number of opportunities for future inquiry and research. These opportunities include the need to understand self-reported health within the context of (a) resiliency; (b) multimorbidity, including factors that mediate and modify the relationship between multimorbidity and self-reported health; and (c) more specifically, how depressive symptoms interact with multimorbidity and other factors to shape self-reported health among community-dwelling older adults. Although there has been exploratory, statistical work over the past few decades, there remains a need to study the process and mechanism that drives how self-reported health is shaped by these factors using longitudinal data. This understanding, addressing current gaps in the literature, and framed by theory related to these concepts, could be used to develop effective interventions aimed at building resilience and maintaining higher levels of self-reported health into older adulthood.
Limitations
As our review focused upon self-reported health as a health measure or exposure, it is possible that we may have missed studies that referred to self-reported health simply as the health status of the individual. We consulted a health sciences librarian on the search strategy and the search terms remained iterative; nonetheless, it is possible that studies that described subjective health status may have been missed due to the keywords used. In addition, because this review defined older adults as those 60 years or older in age, studies with a younger, older adult population (e.g., those aged 55 years or older) were excluded. It is possible that this definition meant the exclusion of studies that included a younger population of older adults.
Warranting further study, this review is limited by the current state of the literature itself as it relates to the concept of resilience among an older adult population. Although only one study included in this review highlighted the fact that resilience was associated with self-reported health, several of the factors identified – for example, an ability to perform activities of daily living; functional status; or social participation – are those which have been described as being related to and comprising measures of resilience (Wister et al., Reference Wister, Lear, Schuurman, MacKey, Mitchell, Cosco and Fyffe2018). There is a need to further explore this conceptual literature related to resilience and the ways in which it overlaps with self-reported health among community-dwelling older adults. In addition, there is a need for future research on this topic to study the relationships between additional factors absent in this evidence, such as immigration status or substance use.
Conclusion
In this scoping review, we identified a body of research that focused on factors associated with self-reported health among community-dwelling older adults. The available literature provided a broad overview of sociodemographic, physical and psychiatric, health-related behaviour; as well as the emotional factors that are associated with self-reported health. Additionally, this review highlighted the need to further understand these factors in terms of how they shape self-reported health and the mechanism underlying the associations identified. As the population of older adults continues to increase, multimorbidity is becoming an important focus in health research. The results of this review emphasize a need to explain how multimorbidity shapes self-reported health, as well as to identify the potential synergistic impacts of co-existing depressive symptoms. A better understanding of these issues will inform how best to support healthy aging and the factors that may contribute to health and wellness.







