With older adults being the fastest-growing demographic segment of the Canadian population, and with life expectancy rates in the 80s (Statistics Canada, 2019), it is important that Canadian researchers, clinicians, and policy makers understand ways in which to improve the quality of years from middle to older adulthood. The extant body of research focusing on the beneficial impact of social participation is clear and well developed, highlighting enhanced quality of life, satisfaction with life, and health-related benefits (Desrosiers et al., Reference Desrosiers, Robichaud, Demers, Gélinas, Noreau and Durand2009; Gilmour, Reference Gilmour2012; Levasseur et al., Reference Levasseur, Cohen, Dubois, Généreux, Richard and Therrien2015). Social connectedness and social engagement are protective factors for older adults’ physical and mental health (Giles, Glonek, Luszcz, & Andrews, Reference Giles, Glonek, Luszcz and Andrews2005; Herzog, Ofstedal, & Wheeler, Reference Herzog, Ofstedal and Wheeler2002). As a related construct to social participation, greater social connection (sense of belonging in one’s social environment) is associated with reduced mortality rates, enhanced cognitive functioning, and decreased rates of dementia and depression (Wang, Karp, Winblad, & Fratiglioni, Reference Wang, Karp, Winblad and Fratiglioni2002; Ybarra et al., Reference Ybarra, Burnstein, Winkielman, Keller, Manis and Chan2008).
These findings are in line with several successful aging theories, including activity theory (Havighurst, Reference Havighurst1961; Lemon, Bengston, & Peterson, Reference Lemon, Bengston and Peterson1972; Longino & Kart, Reference Longino and Kart1982) and continuity theory (Atchley, Reference Atchley1989). Activity Theory specifies that to preserve well-being later in life, older adults should maintain participation in activities from middle age onwards for as long as possible. When participation in these activities is no longer possible for a variety of reasons including retirement, illness, mobility issues, and caregiving, well-being can be promoted by finding and participating in replacement activities. Consistent with activity theory, continuity theory also stresses the importance of consistency in roles and activities throughout the lifespan and making adaptive decisions and taking actions to preserve these aspects of people’s lives. Research by Cohen-Mansfield and Frank (Reference Cohen-Mansfield and Frank2008) highlights the importance of community programs, one component of social participation, to serve the unmet medical, psychological, social, and functional needs of community-dwelling older adults. This statement is echoed in a review study by Koutsogeorgou et al. (Reference Koutsogeorgou, Davies, Aranda, Zissi, Chatzikou and Cerniauskaite2014), which identifies social participation as a vital contributor to the health promotion of older adults.
A large and growing body of Canadian research has examined social participation and the impact of social participation on older adults (e.g., Gilmour, Reference Gilmour2012; Levasseur et al., Reference Levasseur, Gauvin, Richard, Kestens, Daniel and Payette2011; Levasseur et al., Reference Levasseur, Cohen, Dubois, Généreux, Richard and Therrien2015; Naud et al., Reference Naud, Généreux, Alauzet, Bruneay, Cohen and Levasseur2021; Naud, Généreux, Bruneau, Alauzet, & Levasseur, Reference Naud, Généreux, Bruneau, Alauzet and Levasseur2019; Perruccio et al., Reference Perruccio, Yip, Power, Canizares, Gignac and Badley2021; Sibalija, Savundranayagam, Orange, & Kloseck, Reference Sibalija, Savundranayagam, Orange and Kloseck2020). These studies have used nationally representative data from the Canadian Community Health Survey (CCHS)-Healthy Aging, collected between 2008 and 2009, as well as population-based data from the Canadian Longitudinal Study on Aging (CLSA), collected between 2011 and 2015. Using data from the CCHS, a report on the social participation, health, and well-being of Canadian adults 65 years of age and older highlights that 80 per cent of this group participated in at least one social activity. Further, as the number of activities increased, the likelihood of reporting positive self-perceived health increased, and loneliness and life dissatisfaction decreased. Building on this report, findings from research by Naud and colleagues (Reference Naud, Généreux, Alauzet, Bruneay, Cohen and Levasseur2021) using CCHS data highlighted a similar frequency in social participation overall for women and men per month, with small statistical differences between specific age categories (45–64 and 65–74). Age-related differences emerged when examining social participation whereby adults ages 65–74 had higher participation when compared with other age groups assessed (45–64, 75–84, ≥ 85).
Using data from the CLSA, research by Naud and colleagues (Reference Naud, Généreux, Bruneau, Alauzet and Levasseur2019) examined differences in community activities according to Canadian region among adults 65 years of age and older, with findings highlighting no statistical differences in total social participation among regions. With the aim of understanding the association between osteoarthritis and social participation using CLSA data with adults 45–85 years of age, Perruccio and colleagues (Reference Perruccio, Yip, Power, Canizares, Gignac and Badley2021) found that in the absence of activity limitations, osteoarthritis was associated with greater social participation. This finding lends particular insight into the importance of interventions to enhance access to continued social participation among populations of older adults who face barriers to participation, such as activity limitations. Finally, when examining social support, social participation, and depression among caregivers and non-caregivers using data from the CLSA, Sibalija and colleagues (Reference Sibalija, Savundranayagam, Orange and Kloseck2020) highlight the beneficial role of social participation in promoting caregiver mental health, with social participation as a mediator of the relationship between caregiver status and depression.
Although the Canadian literature base concerning aging and social participation is growing, there are several important gaps in this field, which the current research seeks to address. The main objective of this study was to document a nuanced profile of older adults’ engagement with community activities across Canada. Within this objective, our first aim was to explore who participates in community activities; in particular, we sought to describe their socio-demographic, psychosocial, cognitive, and health-related characteristics, and how often they participated. This is additive to the current literature in this area, as other studies have focused primarily on the socio-demographic, regional, and frequency-related characteristics of social participation. Our second aim was to examine the correlates of the frequency of community activity participation. This second objective also serves to augment the current literature base by including a more diverse array of correlates than has been previously studied, with a focus on variables concerning psychosocial characteristics, cognitive health, mental health, and physical health. The first objective was exploratory, and for the second objective, we hypothesized, in line with successful aging theories, that more frequent engagement with community activities would be associated with improved psychosocial and health-related characteristics.
Methods
Sample
We analyzed baseline data of the CLSA (n = 51,338), a population-based survey, administered to a population-based sample of Canadian adults 45–85 years of age (at baseline). Participants were invited to participate in a tracking (n = 21,241) or comprehensive (n = 30,097) cohort. Both cohorts completed the core computer-assisted interviews (e.g., assessing socio-demographic characteristics, lifestyle and social factors, health, service use), while the comprehensive cohort also participated in more in-depth assessment, including a face-to-face interview and a visit to a local data collection site to receive a physical and clinical examination and to provide samples of biological specimens (e.g., blood, urine; see Raina et al., Reference Raina, Wolfson, Kirkland, Griffith, Oremus and Patterson2009 for additional details). Stratified random sampling based on Statistics Canada’s Canadian Community Health Survey on Healthy Aging, health care registration databases and random digit dialing were used to recruit the tracking cohort, and random sampling of health care registration databases and random digit dialing were used for recruitment of the comprehensive cohort. Exclusion criteria eliminated full-time armed forces members, institutionalized individuals at baseline, those with significant cognitive impairment at baseline, residents of Canadian territories or federal First Nations reserves and other Frist Nations settlements, and those who were unable to respond in English or French. Data were collected between 2011 and 2015 using computer-assisted interviews, conducted by trained personnel, and measures included were selected based on having acceptable psychometric properties, their feasibility of administration, and their appropriateness and relevance to adults 45–85 years of age (Raina et al., Reference Raina, Wolfson, Kirkland, Griffith, Oremus and Patterson2009). All participants provided informed consent. Research ethics boards across the Canadian provinces provided ethical approval for CLSA and the University of Manitoba Research Ethics Board provided approval for the use of data for the current study. The CLSA Methodology Working Group derived sampling weights to apply to the data to ensure that the sample adequately represented the Canadian population. These weights were designed based on participant inclusion probability, and they adjust for non-response, unequal probabilities of being sampled, and other limitations of the sampling strategy (Raina et al., Reference Raina, Wolfson, Kirkland, Griffith, Oremus and Patterson2009). Additional details on the CLSA methodology and sampling weights can be found elsewhere (Kirkland et al., Reference Kirkland, Griffith, Menec, Wister, Payette and Wolfson2015; Raina et al., Reference Raina, Wolfson, Kirkland, Griffith, Oremus and Patterson2009, 2019).
Measures
Social participation
Participants self-reported their frequency of participation (i.e., never, at least once a year, at least once a week, at least once a day) for each of eight different types of community activities during the past year: (1) family or friendship-based activities outside the household, (2) church or religious activities (e.g., services, committees, choirs), (3) sports or physical activities engaged in with other people, (4) educational and cultural activities involving other people (e.g., courses, concerts, plays), (5) service club or fraternal organization activities, (6) neighbourhood, community, or professional association activities, (7) volunteer or charity work, and (8) other recreational activities involving other people (e.g., hobbies, gardening, poker, bridge, cards, other games). Based on these responses, CLSA derived a summary variable of participants’ past-year frequency of social participation (engagement with community activities); participants who responded “at least once a day” to any of the eight activities were categorized in the summary variable as “at least once a day”. Of the remaining participants, those who responded “at least once a week” to any of the eight activities were categorized in the summary variable as “at least once a week”, and so on. In order to ensure adequate cell sizes for analyses, we collapsed categories to create a three-level frequency of past-year social participation variable: (1) infrequent/no participation (i.e., never, at least once/year, or at least once/month), (2) moderate participation (i.e., at least once/week), and (3) frequent participation (i.e., at least once/day).
Socio-demographics
We assessed age continuously and categorized sex (male, female), race/ethnicity (white, black, Asian, Indigenous, other), marital status (single/never married, married/common law, widowed, separated/divorced), education (less than high school, completed high school, some college/university, college/university degree), and income (< $20,000, $20,000–49,999, $50,000–99,999, ≥ $100,000) in accordance with prior research (e.g., Stinchcombe, Wilson, Kortes-Miller, Chambers, & Weaver, Reference Stinchcombe, Wilson, Kortes-Miller, Chambers and Weaver2018; Toohey, Hewson, Adams, & Rock, Reference Toohey, Hewson, Adams and Rock2018).
Social support
The Medical Outcomes Study (MOS) Social Support scale assessed social support (Sherbourne & Stweart, Reference Sherbourne and Stweart1991). The MOS scale is composed of 19 items, each rated on a five-point scale ranging from 1 (none of the time) to 5 (all of the time). The scale derives four subscales, including: affection, emotional and informational support, positive social interaction, and tangible social support. We also included a continuous total score.
Cognitive abilities
As part of the CLSA, participants completed the Rey Auditory Verbal Learning Test (Rey, Reference Rey1964), Animal Fluency Test (Crossley, D’Arcy, & Rawson, Reference Crossley, D’Arcy and Rawson1997), and Mental Alternation Test (Teng, Reference Teng1994). Cognitive assessment was completed by telephone for the tracking cohort, and in person for the comprehensive cohort. In accordance with previous research (Oremus et al., Reference Oremus, Konnert, Law, Maxwell, O’Connell and Tyas2019), we created a global cognitive score by standardizing each individual cognitive assessment score and summing the standardized scores to create a composite variable.
Mental health
The Satisfaction with Life Scale (SWLS) assessed participants’ life satisfaction (Diener, Emmons, Larsen, & Griffin, Reference Diener, Emmons, Larsen and Griffin1985). The scale consists of five items, rated on a seven-point scale ranging from 1 (strongly disagree) to 7 (strongly agree). Summing of each of the individual items derives a total score. The 10-item Centre for Epidemiological Studies Depression Scale (CES-D-10) assessed current symptoms of depression (i.e., symptoms in the past week; Kohut, Berkman, Evans, & Cornoni-Huntley, Reference Kohut, Berkman, Evans and Cornoni-Huntley1993), and was assessed continuously. The Primary Care PTSD Screen for the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) assessed lifetime symptoms of post-traumatic stress disorder (PTSD) (Prins et al., Reference Prins, Ouimette, Kimerling, Cameron, Hugelshofer and Shaw-Hegwer2003), and was also assessed continuously. In addition, in line with previous studies (Sekhon, Allali, & Beauchet, Reference Sekhon, Allali and Beauchet2019; Stinchcombe et al., Reference Stinchcombe, Wilson, Kortes-Miller, Chambers and Weaver2018), participants also self-reported whether they had ever been told by a physician that they had a mood disorder (e.g., depression, bipolar disorder, mania, dysthymia) or an anxiety disorder (e.g., phobia, obsessive-compulsive disorder, panic disorder).
Physical conditions
Participants self-reported whether they had ever been told by a physician that they had a physical condition. We categorized them according to physiological systems, clinical recommendation (World Health Organization, 1992), and prior research (e.g., Sommer, Mota, & El-Gabalawy, Reference Sommer, Mota and El-Gabalawy2019): cardiovascular (i.e., heart disease, peripheral vascular disease, hypertension, angina, myocardial infarction), neurologic (i.e., multiple sclerosis, epilepsy, migraine, stroke, transient ischemic attack, Parkinson’s disease), gastrointestinal (i.e., intestinal/stomach ulcer, irritable bowel syndrome/inflammatory bowel disease, bowel incontinence), cancer (i.e., breast cancer, skin cancer, bladder cancer, kidney cancer, lung cancer, thyroid cancer, prostate cancer, ovarian cancer, leukemia, pancreatic cancer, non-Hodgkin lymphoma, other cancer), musculoskeletal/rheumatic (i.e., back problems, hand osteoarthritis, hip osteoarthritis, knee osteoarthritis, rheumatoid arthritis, other arthritis, osteoporosis), endocrine/metabolic (i.e., hypothyroid, hyperthyroid, diabetes), urogenital (i.e., urinary incontinence, kidney disease), respiratory (i.e., asthma, chronic obstructive pulmonary disease), and ophthalmologic (i.e., macular degeneration, cataracts, glaucoma). We also computed a continuous variable to assess the number of physical conditions.
Analytic Strategy
Inflation weights were applied for descriptive analyses (e.g., calculating proportions, means) and analytic weights were applied for analyses examining relationships between variables (e.g., regression). We assessed the weighted frequency of social participation (i.e., infrequent/no, moderate, frequent). Next, weighted cross-tabulations with χ 2 analyses and descriptive statistics with analyses of variance (ANOVAs) examined whether differences existed in sample characteristics (i.e., socio-demographics and psychosocial, cognitive, mental health, and physical health correlates) according to frequency of social participation. For ANOVAs for which the omnibus test was significant, Tukey’s Honest Significant Difference (HSD) post-hoc test assessed group differences for continuous variables, and Cohen’s d values were calculated as an indicator of effect size. Finally, multivariable regressions examined associations between frequency of social participation (i.e., infrequent/no [reference], moderate, frequent) and psychosocial (i.e., social support), cognitive (i.e., Rey Auditory Verbal Learning Score, Animal Fluency Score, Mental Alternation Score, global cognitive score), mental health (i.e., satisfaction with life, depressive symptoms, post-traumatic stress symptoms, mood disorder, anxiety disorder), and physical health (i.e., number of physical conditions) correlates; dependent variables were assessed continuously (examined with linear regressions), with the exception of the dichotomous mood and anxiety disorders (examined with logistic regressions). We ran three regression models, including: (1) an unadjusted model, (2) a model adjusting for socio-demographic characteristics (i.e., age, sex, race/ethnicity, education, marital status, income), and (3) a model additionally adjusting for other correlates of social participation (e.g., when examining social support as the dependent variable, we adjusted for global cognitive score, depressive symptoms, and number of physical conditions). Analyses were conducted using SPSS and STATA statistical software in order to employ the proper weighting (using sample weights provided by the CLSA) and variance estimation techniques.
Results
Sample Characteristics According to Frequency of Social Participation
As shown in Table 1, significant differences emerged across all sample characteristics according to frequency of community activity participation. Among those reporting infrequent/no participation (≤ once/month), participants were on average 60 years old, primarily male (55.6%), white (91.9%), married/common law (70.5%), with a college/university degree (63.5%), and an income of $50,000 or higher (64.1%). Those who reported moderate participation (once/week) were also 60 years old on average, and primarily female (52.7%), white (92.6%), married/common law (75.0%), with a college/university degree (74.2%), and an income of $50,000 or higher (72.7%). Participants who reported frequent participation (once/day) were 61 years old, on average, and primarily female (54.1%), white (92.2%), married/common law (78.3%), with a college/university degree (75.0%), and an income of $50,000 or higher (74.3%). Post-hoc analyses clarified that those who frequently engaged in activity participation reported having the greatest social support (mean = 65.81) and satisfaction with life (mean = 29.43); those who engaged in moderate and frequent participation had the highest global cognitive scores (mean = 0.36–0.40) and the fewest number of physical conditions, on average (mean = 2.66–2.68); those who reported infrequent/no participation had the highest number of current depressive symptoms (mean = 6.64) and lifetime post-traumatic stress symptoms (mean = 0.57), on average, and the highest prevalence of self-reported lifetime mood (21.0%) and anxiety (11.1%) disorders. The effect sizes of differences in key variables between those participating infrequently and those participating frequently ranged from small to medium: number of physical conditions (d = 0.11), lifetime post-traumatic stress symptoms (d = 0.14), global cognitive abilities (d = 0.22), depressive symptoms (d = 0.37), social support (d = 0.48), and satisfaction with life (d = 0.52).
Table 1. Sample characteristics according to frequency of social participation
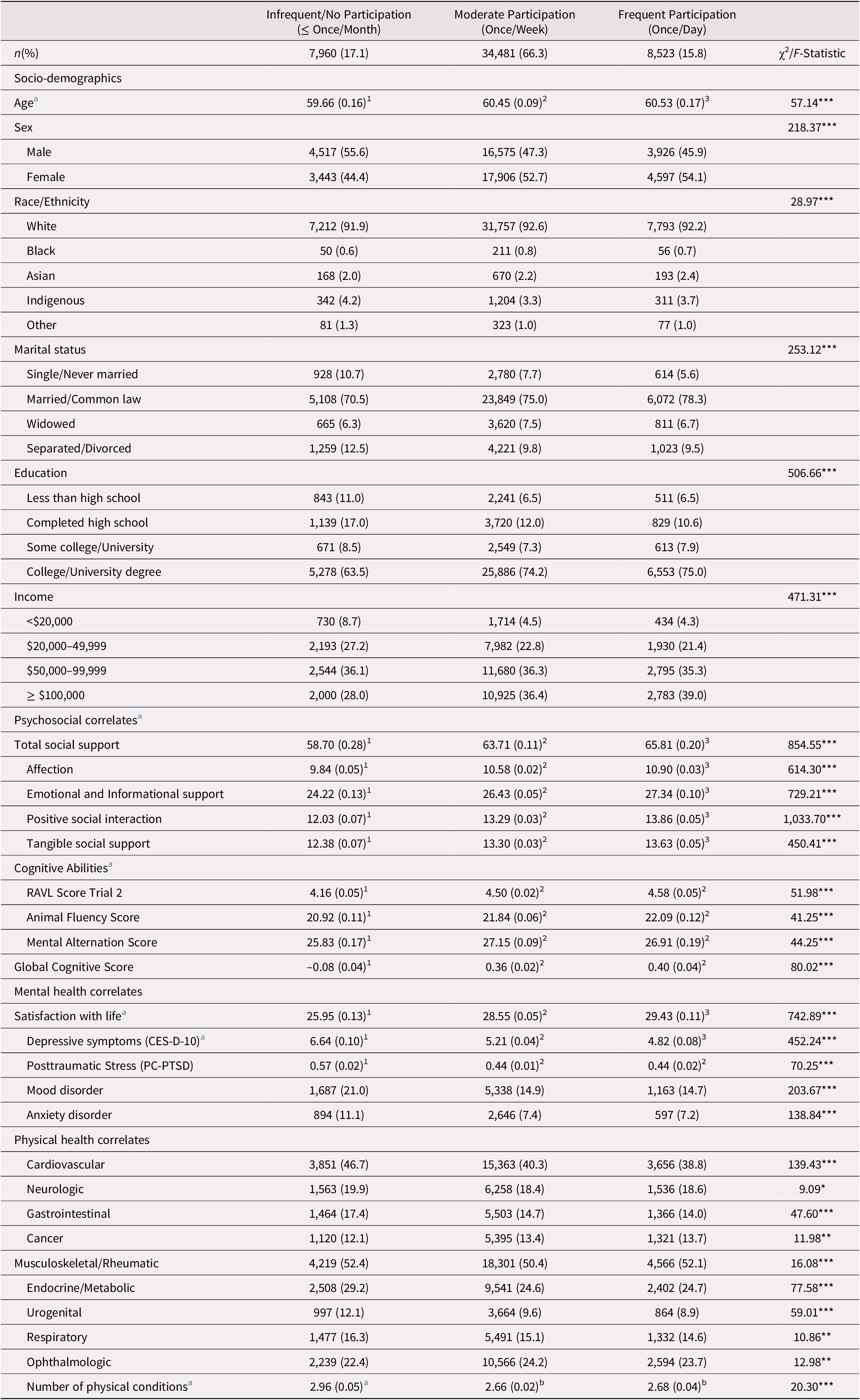
Note. Values represent n(%) of each characteristic/condition, according to frequency of participation in social activities. Superscript numbers indicate post-hoc Tukey’s HSD test group differences. Values that share the same superscript do not significantly differ
a Values represent M(SE) and F-value.
*p < 0.05, **p < 0.01, ***p < 0.001
RAVL = Rey Auditory Verbal Learning Score.
Correlates of Frequency of Social Participation
As specified in Table 2, after adjusting for socio-demographics and other correlates of participation (i.e., total social support, global cognitive score, depressive symptoms, and number of physical conditions, minus the dependent variable of interest), compared infrequent/no participation, moderate participation was associated with greater social support (unstandardized regression coefficient [b] = 3.33, 95% confidence interval [CI] [2.93-3.73], p < 0.001), a higher score on all cognitive tests including the global cognitive score (b range: 0.11–0.49, p < 0.01), increased satisfaction with life (b = 1.18, 95% CI [0.98–1.39], p < 0.001), fewer depressive symptoms (b = –0.58, 95% CI [−0.73 – −0.43], p < 0.001), reduced odds of both mood (adjusted odds ratio [AOR] = 0.82, 95% CI [0.75–0.90], p < 0.001) and anxiety disorders (AOR = 0.86, 95% CI [0.77–0.96], p < 0.01), and fewer physical conditions (b = −0.16, 95% CI [−0.23 – −0.10], p < 0.001). In addition, compared with infrequent/no participation, frequent participation was associated with greater social support (b = 5.19, 95% CI [4.72–5.65], p < 0.001), a higher animal fluency (b = 0.52, 95% CI [0.28–0.75], p < 0.001) and global cognitive score (b = 0.13, 95% CI [0.05–0.20], p < 0.01), increased satisfaction with life (b = 1.63, 95% CI [1.40–1.87], p < 0.001), fewer depressive symptoms (b = –0.82, 95% CI [−1.00 – −0.65], p < 0.001), reduced odds of both mood (AOR = 0.74, 95% CI [0.66–0.83], p < 0.001) and anxiety disorders (AOR = 0.81, 95% CI [0.70–0.94], p < 0.01), and fewer physical conditions (b = −0.13, 95% CI [−0.21 – −0.05], p < 0.01). Frequency of participation was not associated with post-traumatic stress symptoms in the most stringent model.
Table 2. Associations between frequency of social participation and psychosocial, cognitive, and health-related correlates
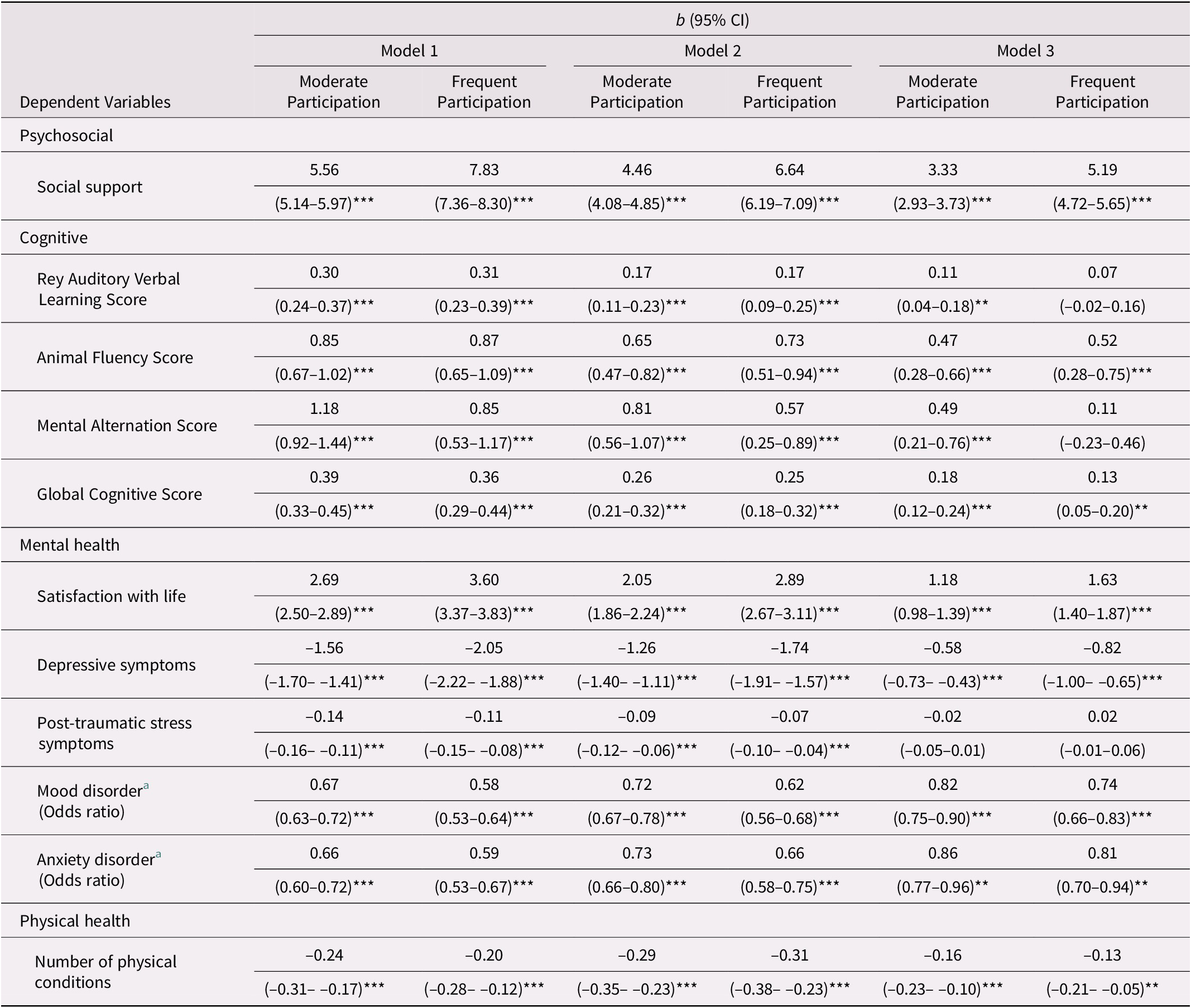
Note. Reference = infrequent/no participation; b = unstandardized regression coefficients; Model 1 = unadjusted; Model 2 = adjusted for socio-demographics (age, sex, race/ethnicity, education, marital status, income); Model 3 = adjusted for socio-demographics, and total social support, global cognitive score, depressive symptoms, and number of physical conditions (minus the dependent variable of interest).
a Values represent odds ratios (i.e., for dichotomous dependent variables).
**p < 0.01, ***p < 0.001.
Discussion
This study provides novel and important insights into the characteristics of Canadian older adults who participate in community activities, and the psychosocial and health-related correlates of their participation. Key findings highlight that those who moderately (i.e., at least once/week) or frequently (i.e., at least once/day) engage in community activities report greater social support, higher cognitive abilities, increased satisfaction with life, fewer depressive symptoms, reduced odds of mood and anxiety disorders, and fewer physical conditions than those who report infrequent/no participation. Findings from this representative Canadian data set demonstrate that moderate or frequent participation is associated with more positive psychosocial and health-related correlates.
It is possible that our findings are reflective of long-standing successful aging theories, activity theory (Havighurst, Reference Havighurst1961; Lemon et al., Reference Lemon, Bengston and Peterson1972; Longino & Kart, Reference Longino and Kart1982) and continuity theory (Atchley, Reference Atchley1989). There is something unique about how often people participate in community activities that has important, meaningful association with social support and health-related characteristics. As previously outlined, activity theory purports that well-being is enhanced when activity participation is maintained from middle age into older age, and that when participation in such an activity is not possible or made more challenging, those who can adapt to find replacement activities tend to experience continued well-being. Continuity theory also stresses the importance of a continuation of previous activities and frequency of participation and roles held within activities from middle age to older age. These findings, and their theoretical bases, are particularly timely in the current context of the COVID-19 pandemic, when it is becoming increasingly challenging for older adults to adapt preferred activities to telephone, virtual, or physically distanced platforms. It is important for researchers, clinicians, community organizations, and older adults, to work together to create opportunities for continued participation in community activities, given the strong associations with physical and mental well-being.
We found significant differences in the demographic characteristics of adults dependent on their frequency of participation. Adults participating moderately or frequently in community activities tended to be older in age, identifying as female, white, in a married/common law relationship, highly educated (college/university), with greater income levels (≥ $100,000). Taken together, the benefits of moderate to frequent social participation, paired with reduced participation among certain demographic groups, render important implications for community social program design and access. Further to this, important findings indicated that those who reported moderate or frequent engagement with community activities also reported higher cognitive abilities, fewer depressive symptoms, reduced odds of mood and anxiety disorders, and fewer physical conditions than those who reported infrequent/no participation. It is possible that adults who are experiencing challenges related to cognition, mental health, and physical health are excluded or do not feel as though there is a place for them in community activities, and therefore are not able to experience the beneficial impact that others experience in these areas from this participation.
Future research is needed to extend findings of the current research, by examining the socio-demographic and health-related (i.e., cognitive, mental health, and physical health) barriers to engagement with community activities among a representative sample of Canadian older adults. Participatory program development approaches which include those who will be engaged in programs that will be developed are necessary in allowing the unique voices of older adults to influence the development of community-based social activities and programs. It is recommended that community organizations work to ensure that programs being developed are of interest and accessible to older adults with diverse gender and relationship identifications and racial/ethnic backgrounds, and those reporting varying levels of socio-economic status. Although this was not assessed in our study, programs should also be made accessible to older adults with a range of cognitive, mental, and physical health problems, engaging these populations to investigate their interests and their barriers to participation. Future needs assessment research is needed to determine older adults’ perceptions regarding social participation, with a focus on under-represented groups.
Limitations
Because of the cross-sectional nature of these data, we are not able to make claims regarding the causality of trends, and longitudinal analyses, including those completed with now-available CLSA follow-up data, are warranted in future research. Although this study’s sample is considered nationally representative, certain subgroups may still be under-represented and therefore results may not generalize to these groups (Raina et al., Reference Raina, Wolfson, Kirkland, Griffith, Balion and Cossette2019). The application of sampling weights does help correct for some under-representation, although not all. For example, because of exclusion criteria, institutionalized individuals (e.g., hospital inpatients) are not included in the baseline sample, and therefore, our sample may not include a subgroup of individuals who may have limited access to social participation. In the current study, we used the entire sample of adults ranging in age from 45 to 85 years. Regarding engagement with community activities, it is important to note that younger participants (ages 45–65) are at a greater likelihood to be in the workforce, and some may be taking care of dependent children. Future research could consider stratifying the sample by age, to examine those ≥ 65 years of age. In the current study, we examined all social participation activities as having equal value or weighting. Although beyond the scope of the current study, prior research has shown that different activities may be associated with differential impact (e.g., Perruccio et al., Reference Perruccio, Yip, Power, Canizares, Gignac and Badley2021). Future research should consider the impacts of activity type and frequency of participation, particularly among samples of adults experiencing challenges related to cognition, mental health, or physical health. An additional limitation of the data used in this study is the reliance on retrospective self-report data, rather than on clinically assessed mental health and physical conditions. Further to this, social participation was assessed as retrospective self-report, rather than as real-time reporting or more observational methods of community-based data collection.
Conclusions
Our research lends support to findings outlined in prior work (i.e., Cohen-Mansfield & Frank, Reference Cohen-Mansfield and Frank2008; Koutsogeorgou et al., Reference Koutsogeorgou, Davies, Aranda, Zissi, Chatzikou and Cerniauskaite2014) highlighting that the community is a place where health should be promoted among older adults. Findings are situated within a growing body of Canadian research exploring the impact of social participation among older adults, demonstrating the importance of this participation for health and wellness, and we echo the need for increased access to social participation for all Canadians. Multi-systemic and public-engagement strategies are needed to increase access to participation in social activities among older adults who are a steadily growing segment of our population.
Acknowledgment
This research was made possible using the data/biospecimens collected by the CLSA. Authors extend thanks to CLSA researchers, staff, and participants, and also acknowledge Scott Nowicki for his contributions to this work. Finally, the authors acknowledge funding from the University of Manitoba (K. Reynolds, PI).
Disclaimer
The opinions expressed in this manuscript are the authors’ own and do not reflect the views of the CLSA.
Funding
The authors acknowledge funding from the University of Manitoba (K. Reynolds, P.I.). Funding for the CLSA is provided by the government of Canada through the Canadian Institutes of Health Research (CIHR) under grant reference: LSA 94473, and the Canada Foundation for Innovation. This research has been conducted using the CLSA, Baseline Tracking data set v3.2, Baseline Comprehensive data set v3.0, under Application Number 161019. The CLSA is led by Drs. Parminder Raina, Christina Wolfson and Susan Kirkland.





