Background
Dementia is a terminal illness; however, the disease trajectory is highly unpredictable, making prognostication difficult (Smith & Ferguson, Reference Smith and Ferguson2017). Dementia is typically complicated by the presence of multiple chronic diseases, increasing the risk for frequent hospitalizations and emergency department visits (Mondor et al., Reference Mondor, Maxwell, Hogan, Bronskill, Gruneir and Lane2017). As cognitive abilities and decision-making capacity worsen, caregivers are expected to make care decisions on behalf of the persons living with dementia, which may exert increased caregiver burden (Gofton, Jog, & Schulz, Reference Gofton, Jog and Schulz2009) and care that may be discordant with wishes of the care recipients. As a result, in the last year of their life, people with advanced dementia may receive burdensome medical interventions such as enteral nutrition, and suboptimal management of pain (Cintra, de Rezende, de Moraes, Cunha, & da Gama Torres, Reference Cintra, de Rezende, de Moraes, Cunha and da Gama Torres2014).
A “palliative approach” has been suggested as a way to conceptualize care for people with non-cancer chronic illnesses – such as dementia – who may not require the formal palliative care services (Kristjanson, Toye, & Dawson, Reference Kristjanson, Toye and Dawson2003) that are usually delivered by palliative specialists. A palliative approach utilizes the principles of palliative care, which involve the physical, social, emotional, and spiritual aspects of holistic care (Gamondi, Larkin, & Payne, Reference Gamondi, Larkin and Payne2013), to meet the needs of the person and their caregivers at all stages of chronic diseases, not just at the end of life (Canadian Hospice Palliative Care Association, 2013a, 2015), and which can be delivered by health care practitioners regardless of their training, role, and work setting (Touzel & Shadd, Reference Touzel and Shadd2018). In this scoping review, the conceptualization of a palliative approach in the care of older adults with dementia was drawn from the work by Maciver and Ross (Reference Maciver and Ross2018), the Canadian Hospice Palliative Care Association (2013b), Touzel and Shadd (Reference Touzel and Shadd2018), and van der Steen et al. (Reference van der Steen, Radbruch, Hertogh, de Boer, Hughes and Larkin2014). The four consistent components within each of the above works include (1) advance care planning (ACP), (2) pain and symptom management, (3) psychosocial and spiritual support, and (4) the process of shared decision making. Advance care planning is defined as “a process that supports adults at any age or stage of health in understanding and sharing their values, life goals, and preferences regarding future medical care” (Sudore et al., Reference Sudore, Lum, You, Hanson, Meier and Pantilat2017). Pain and symptom management are interventions instituted to maximize comfort to optimize the quality of life (Canadian Hospice Palliative Care Association, 2015), whereas psychosocial and spiritual care provide emotional support, boost hope, address stress, and increase the quality of life of patients and caregivers coping with chronic medical conditions (Canadian Hospice Palliative Care Association, 2015; Reyes-Ortiz, Reference Reyes-Ortiz2015). The process of shared decision making is proactive and iterative (Maciver & Ross, Reference Maciver and Ross2018) and involves evidence-informed decision making among practitioners, patients and care partners (Elwyn et al., Reference Elwyn, Coulter, Laitner, Walker, Watson and Thomson2010; van der Steen et al., Reference van der Steen, Radbruch, Hertogh, de Boer, Hughes and Larkin2014).
The majority of people with dementia live in the community (Alzheimer’s Association, 2018; Dudgeon, Reference Dudgeon2010; Wertman, Brodsky, King, Bentur, & Chekhmir, Reference Wertman, Brodsky, King, Bentur and Chekhmir2007), and these numbers are projected to increase exponentially (Dudgeon, Reference Dudgeon2010). The supply of geriatric practitioners is insufficient to meet the demands of the rising number of older adults (Canadian Nurses Association, 2016; Warshaw & Bragg, Reference Warshaw and Bragg2014). Furthermore, only about 15 per cent of persons with dementia receive any specialist palliative care services in the community in the last year of their life, and less than 1.9 per cent of these receive physician home visits (Seow, O’Leary, Perez, & Tanuseputro, Reference Seow, O’Leary, Perez and Tanuseputro2018). As such, most people with dementia, including those approaching the end of life, are cared for by primary care providers in community settings (Shadd et al., Reference Shadd, Burge, Stajduhar, Cohen, Kelley and Pesut2013). Hence, primary care providers, both nurse practitioners (NP) and physicians, should be well situated to integrate a palliative approach when caring for older adults with dementia in their practice.
Authors in previous studies have examined how a palliative care approach was perceived and operationalized by nurses and physicians working in primary care settings, who cared for patients with life-limiting chronic illnesses (Reimer-Kirkham, Sawatzky, Roberts, Cochrane, & Stajduhar, Reference Reimer-Kirkham, Sawatzky, Roberts, Cochrane and Stajduhar2016; Rewegan et al., Reference Rewegan, Danho, White, Winemaker, Hansen and MacLennan2019). The authors found that in caring for these patients, these clinicians were employing strategies that are aligned with the principles of palliative care, yet, clinicians tended to meld a palliative approach with specialist palliative services that are mostly limited to the end-of-life period as opposed to having an upstream focus. There remains an important gap in understanding the perspectives and experiences of primary care providers (nurses and physicians) on an integrated palliative approach in dementia care, as well as the impact of existing programs and models of care in primary care using an integrated palliative approach in dementia.
Past reviews have specifically examined outcomes of a integrated palliative approach in caring for individuals with dementia with most studies involving institutional care settings (Hines et al., Reference Hines, McCrow, Abbey, Foottit, Wilson and Franklin2011; Sampson, Ritchie, Lai, Raven, & Blanchard, Reference Sampson, Ritchie, Lai, Raven and Blanchard2005). No review, to our knowledge, has specifically focused on health care providers (nurses and physicians) in primary care/community settings and the integration of a palliative approach throughout the dementia trajectory. To address this gap, we aim to examine the literature guided by the following questions:
1. What are the nurses’ and physicians’ perspectives and experiences regarding the integration of a palliative approach in the care of older adults with dementia in primary care settings?
2. What are the impacts of the integration of a palliative approach in the care of older adults with dementia in primary care settings on patients, caregivers, and health care utilization outcomes?
A scoping review was selected because it aligned with the goal of exploring the topic’s breadth and depth in the available literature (Colquhoun et al., Reference Colquhoun, Levac, O’Brien, Straus, Tricco and Perrier2014). Furthermore, it allowed us to examine the broad scope of different community-based programs aimed at integrating a palliative approach into the care of older adults with dementia. It also explores a wide variety of perspectives and experiences of practitioners in primary care settings, including nurses and physicians, pertaining to an integrated palliative approach. This examination of empirical literature has important implications for enhancing the practice of primary care practitioners in the delivery of quality dementia care in primary care settings. This review also highlights gaps in current knowledge and the need for more research in this area.
Methods
We developed the review protocol according to the framework outlined by Arksey and O’Malley (Reference Arksey and O’Malley2005), and advanced by Levac, Colquhoun, and O’Brien (Reference Levac, Colquhoun and O’Brien2010), and followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) statement (Tricco et al., Reference Tricco, Lillie, Zarin, O’Brien, Colquhoun and Levac2018) (Supplement A). MEDLINE®, Cumulative Index to Nursing and Allied Health Literature (CINAHL), PsycInfo, Embase, and Ageline databases were searched for studies between 1990 and February 2018, as significant seminal work was done in the early 1990s on palliative care (Mohanti, Reference Mohanti2011). The search strategy was updated in October 2019. Based on the descriptive aims of the review, three key concepts made up the search strategy, "older adults", "dementia", and "palliative approach", which was developed in consultation with an information specialist at the University of Toronto libraries. The search strategy was translated according to each database platform’s command language, controlled vocabulary, and appropriate search fields. For example, the search terms for the broad concept of palliative approach included palliative care, palliat*.tw,kf., palliat* adj3 (care or approach or utiliz* or method*)).tw,kf. Supplement B presents an example of the MEDLINE search strategy.
Criteria
The inclusion criteria were
-
• Original research studies using quantitative, qualitative, and mixed-methods research designs
-
• Studies published in English and addressing the integration of palliative care principles and practices (Sawatzky et al., Reference Sawatzky, Porterfield, Lee, Dixon, Lounsbury and Pesut2016) for people with dementia in primary care settings even though the term “palliative approach” may not have been explicitly used
-
• Studies in which the mean age of the study population was ≥ 65 years
-
• Studies that addressed the perspectives and experiences of nurses and physicians working in primary care settings on the integration of a palliative approach for older adults with dementia in their care; and/or that reported on the impact of an integrated palliative approach on older adults, caregivers, and/or health care utilization outcomes.
The exclusion criteria were
-
• Editorials, reviews, expert opinions, and materials that did not include original data
-
• Publications about medical assistance in dying (MAID), withdrawal of care, euthanasia, and assisted suicide
-
• Studies involving settings other than primary care; for example, acute care and/or long-term care
-
• Studies with the exclusive focus on end-of-life care
Data Analysis
We used the EndNote reference manager to collate 2,945 retrieved records. After systematic de-duplication, a final unique set of 2,153 records were imported into Covidence. This Web-based software program streamlines the screening, study selection, and data extraction for the literature reviews (www.covidence.org). Article screening, selection, data extraction, and quality assessment were completed independently by two reviewers (S.V. and C.D.) for each of the included studies, and consensus was reached through discussion. Cases of disagreement between reviewers were resolved by a third reviewer (K.M.). In the first stage of study selection, titles and abstracts of each article were screened, whereas in the second stage, full-text screening was completed for 70 articles that were deemed relevant. We also screened the reference lists of all the included studies. Where results of a study were reported in more than one publication, they were grouped.
The data were extracted by two authors (S.V. and C.D.) for each of the included studies and then compared and amalgamated, using a pre-piloted form on the details of the study type (quantitative, qualitative, report); physicians’ and nurses’ characteristics (specialty type, years of experience, additional educational preparation); patient and/or caregiver characteristics (age, gender, ethnicity, number of chronic conditions, dementia stage); features of a palliative approach; impact of integration of a palliative approach in dementia care; and categories/themes – if used; as well as nurses’ and physicians’ perspectives and experiences in integrating a palliative approach in the care of older adults with dementia in primary care settings, referring back to the research questions as a guide (Levac et al., Reference Levac, Colquhoun and O’Brien2010) (sample data abstraction form available from the corresponding author upon request). We used the Mixed Methods Appraisal Tool (MMAT) to critically appraise diverse designs in this review, with quality criteria specific to each design (Hong et al., Reference Hong, Pluye, Fàbregues, Bartlett, Boardman and Cargo2018). It allowed us to summarize the quality of the evidence, as well as to guide the design of high-quality studies in future. However, no study was excluded based on the MMAT scores, to be consistent with the goals of the scoping reviews (Joanna Briggs Institute, 2015).
We followed Arksey and Malley’s as well as Levac et al.’s suggestion to analyze the extracted data in the context of each objective using a descriptive numerical summary to describe the characteristics of the study, participants, and interventions (Colquhoun et al., Reference Colquhoun, Levac, O’Brien, Straus, Tricco and Perrier2014; Daudt, van Mossel, & Scott, Reference Daudt, van Mossel and Scott2013; Levac et al., Reference Levac, Colquhoun and O’Brien2010). We used a narrative synthesizing approach guided by the definition of a palliative approach in the care of older adults with dementia operationalized for this review (Popay et al., Reference Popay, Roberts, Sowden, Petticrew, Arai and Rodgers2006). This served as a common analytical framework for organizing and synthesizing standard information from each study to support mapping the data. As a result, it not only helped frame a nebulous concept that was useful in organizing the data synthesis but stands a higher likelihood of being useful in clinical practice.
Results
Characteristics of the Included Studies
Figure 1 describes our PRISMA flow diagram and the study selection process. Of 2,153 studies, 17 (21 articles) met inclusion criteria. Of the 17 studies, 8 addressed the perspectives of physicians and/or nurses, whereas, 9 studies reported on the impact of a palliative approach in the care of older adults with dementia in primary care settings (Carduff et al., Reference Carduff, Jarvis, Highet, Finucane, Kendall and Harrison2016; Clevenger, Cellar, Kovaleva, Medders, & Hepburn, Reference Clevenger, Cellar, Kovaleva, Medders and Hepburn2018; Daaleman et al., Reference Daaleman, Ernecoff, Kistler, Reid, Reed and Hanson2019; Holley, Gorawara-Bhat, Dale, Hemmerich, & Cox-Hayley, Reference Holley, Gorawara-Bhat, Dale, Hemmerich and Cox-Hayley2009; Hum et al., Reference Hum, Wu, Ali, Leong, Chin and Lee2018; London, McSkimming, Drew, Quinn, & Carney, Reference London, McSkimming, Drew, Quinn and Carney2005; Nakanishi, Hirooka, Morimoto, & Nishida, Reference Nakanishi, Hirooka, Morimoto and Nishida2017; Sternberg et al., Reference Sternberg, Sabar, Katz, Segal, Fux-Zach and Grofman2019; Treloar, Crugel, & Adamis, Reference Treloar, Crugel and Adamis2009). Eight of nine studies involved persons with late stage of dementia, whereas one study did not report the dementia stage (Daaleman et al., Reference Daaleman, Ernecoff, Kistler, Reid, Reed and Hanson2019). No study addressed both the research questions. Supplement C describes the summary of the included studies. The selected articles included 7 (41%) qualitative, 8 (47%) quantitative, and 2 (11.7%) mixed-method studies. No randomized control trial was identified. Ten studies were conducted in Europe, four in the United States, and three in Asia (Singapore, Israel, and Japan).
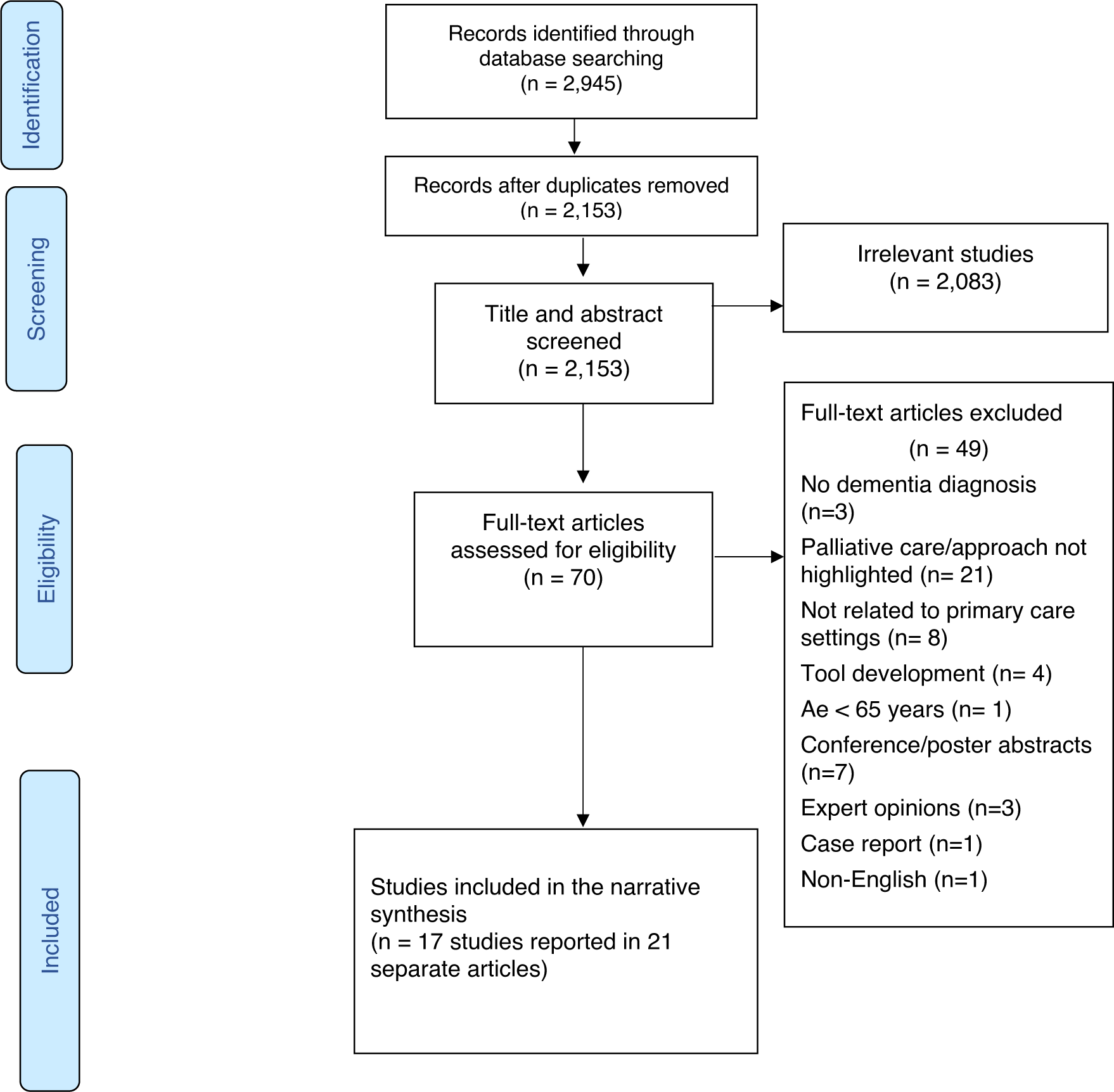
Figure 1: PRISMA flow diagram
The sample size in eight studies (Beernaert et al., Reference Beernaert, Deliens, Vleminck, Devroey, Pardon and Den Block2014; Brazil, Carter, Galway, Watson, & van der Steen, Reference Brazil, Carter, Galway, Watson and van der Steen2015; Carduff et al., Reference Carduff, Jarvis, Highet, Finucane, Kendall and Harrison2016; Davies et al., Reference Davies, Maio, van Riet Paap, Mariani, Jaspers and Sommerbakk2014; De Witt Jansen et al., Reference De Witt Jansen, Brazil, Passmore, Buchanan, Maxwell and McIlfatrick2017; Evans et al., Reference Evans, Pasman, Donker, Deliens, Van den Block and Onwuteaka-Philipsen2014; Ryan, Gardiner, Bellamy, Gott, & Ingleton, Reference Ryan, Gardiner, Bellamy, Gott and Ingleton2012; Vleminck et al., Reference Vleminck, Pardon, Beernaert, Deschepper, Houttekier and Audenhove2014) involving physicians and nurses, varied from 1 (Carduff et al., Reference Carduff, Jarvis, Highet, Finucane, Kendall and Harrison2016) to 188 (Brazil et al., Reference Brazil, Carter, Galway, Watson and van der Steen2015) with a total sample size of 459 primary care physicians and 195 nurses. Of six studies in which response rate was applicable (Brazil et al., Reference Brazil, Carter, Galway, Watson and van der Steen2015; Evans et al., Reference Evans, Pasman, Donker, Deliens, Van den Block and Onwuteaka-Philipsen2014; Holley et al., Reference Holley, Gorawara-Bhat, Dale, Hemmerich and Cox-Hayley2009; London et al., Reference London, McSkimming, Drew, Quinn and Carney2005; Nakanishi et al., Reference Nakanishi, Hirooka, Morimoto and Nishida2017; Treloar et al., Reference Treloar, Crugel and Adamis2009), five reported it. It ranged from 25.6 per cent (Nakanishi et al., Reference Nakanishi, Hirooka, Morimoto and Nishida2017) to 100 per cent (Treloar et al., Reference Treloar, Crugel and Adamis2009). Details on the characteristics of the health care practitioners are provided in Supplement D.
Table 1 summarizes the features of a palliative approach addressed in the included studies based on our operationalized definition. Ten of the 17 studies highlighted all four features; that is, ACP, pain and symptom management, psychosocial and spiritual support, and shared decision making (Brazil et al., Reference Brazil, Carter, Galway, Watson and van der Steen2015; Clevenger et al., Reference Clevenger, Cellar, Kovaleva, Medders and Hepburn2018; Daaleman et al., Reference Daaleman, Ernecoff, Kistler, Reid, Reed and Hanson2019; Davies et al., Reference Davies, Maio, van Riet Paap, Mariani, Jaspers and Sommerbakk2014; Evans et al., Reference Evans, Pasman, Donker, Deliens, Van den Block and Onwuteaka-Philipsen2014; Holley et al., Reference Holley, Gorawara-Bhat, Dale, Hemmerich and Cox-Hayley2009; Hum et al., Reference Hum, Wu, Ali, Leong, Chin and Lee2018; London et al., Reference London, McSkimming, Drew, Quinn and Carney2005; Ryan et al., Reference Ryan, Gardiner, Bellamy, Gott and Ingleton2012; Treloar et al., Reference Treloar, Crugel and Adamis2009), whereas the remaining studies, except one (Carduff et al., Reference Carduff, Jarvis, Highet, Finucane, Kendall and Harrison2016), addressed at least two. No study reported a feature that is not captured in our definition.
Table 1. Features of a palliative approach in dementia care addressed in the studies
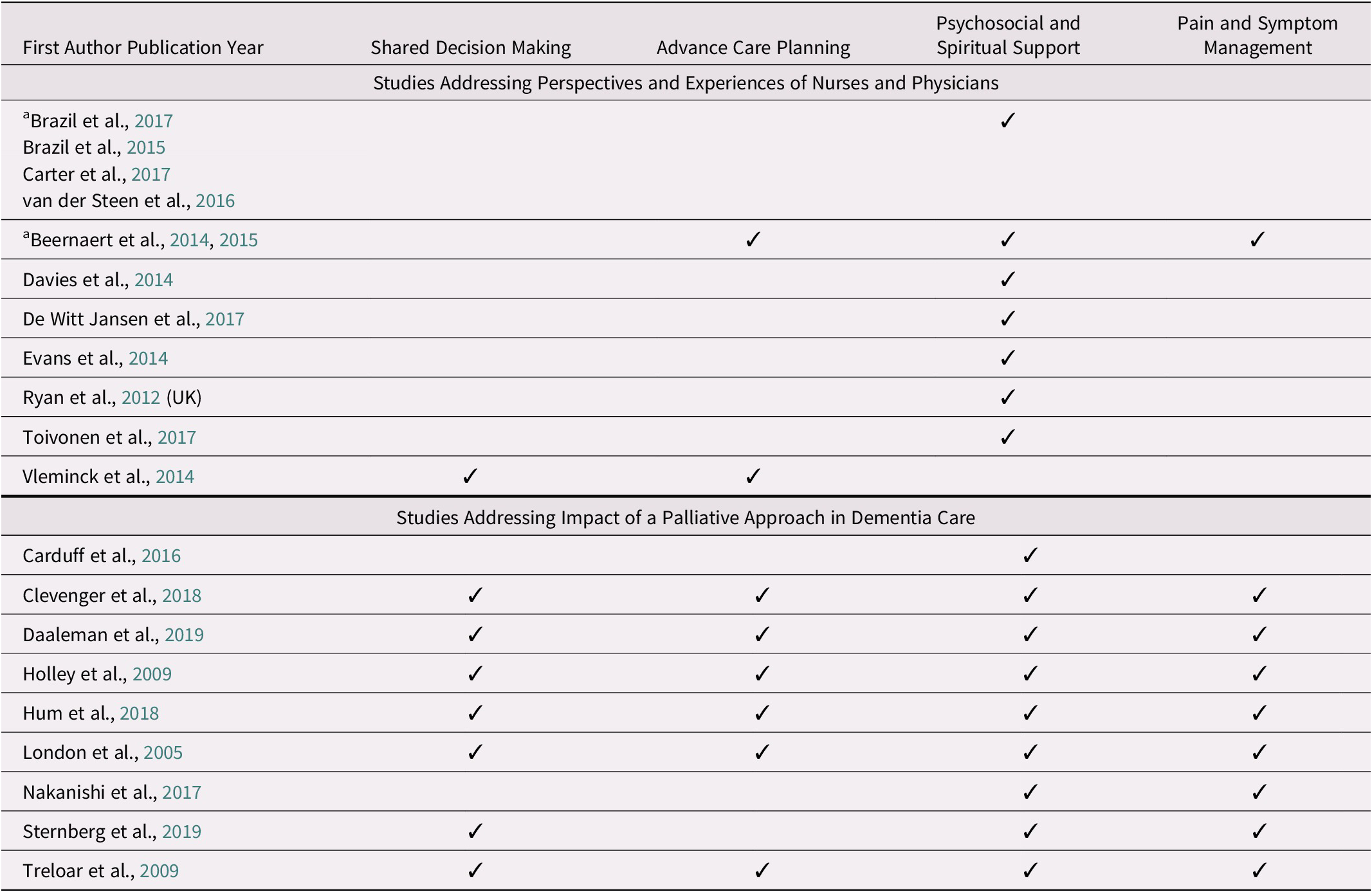
Note. aDenotes study presented in more than one article.
Quality Assessment
The quality assessment result is presented in Supplement E based on the MMAT. The authors of MMAT discourage calculating the overall score of the included studies (Hong et al., Reference Hong, Pluye, Fàbregues, Bartlett, Boardman and Cargo2018), however, the majority (n = 8) of the studies only met 40 per cent of the quality criteria. Quality assessment using MMAT enabled us to provide a comprehensive overview of the methodological quality of the available evidence (Pluye, Reference Pluye and Hong2014). Studies measuring the impact of a palliative approach had small sample sizes and sources of bias, leading to questions about the generalizability of the results. Nonetheless, it is crucial to conduct further research with rigorous methods to accumulate findings related to the effectiveness of this approach in dementia care.
Among the quantitative studies, in which response rates were indicated, only one was below 30 per cent (Nakanishi et al., Reference Nakanishi, Hirooka, Morimoto and Nishida2017). The primary author of this study clarified that the low response rate of 25.6 per cent is comparable to other surveys in Japan. For most of the qualitative studies, issues concerning reflexivity and positionality were not discussed; hence, they may influence the interpretation of data. The qualitative studies were mainly descriptive without theoretical or paradigmatic foundations.
Question 1: Perspectives and Experiences of Nurses and Physicians
Table 2 presents a summary of nurses’ and physicians’ perspectives on integration of a palliative approach in the care of older adults with dementia in community settings. The next section presents the details on each of the four components of the definition of a palliative approach as operationalized for this review.
Table 2. Perspectives and experiences of nurses and physicians regarding integration of palliative approach
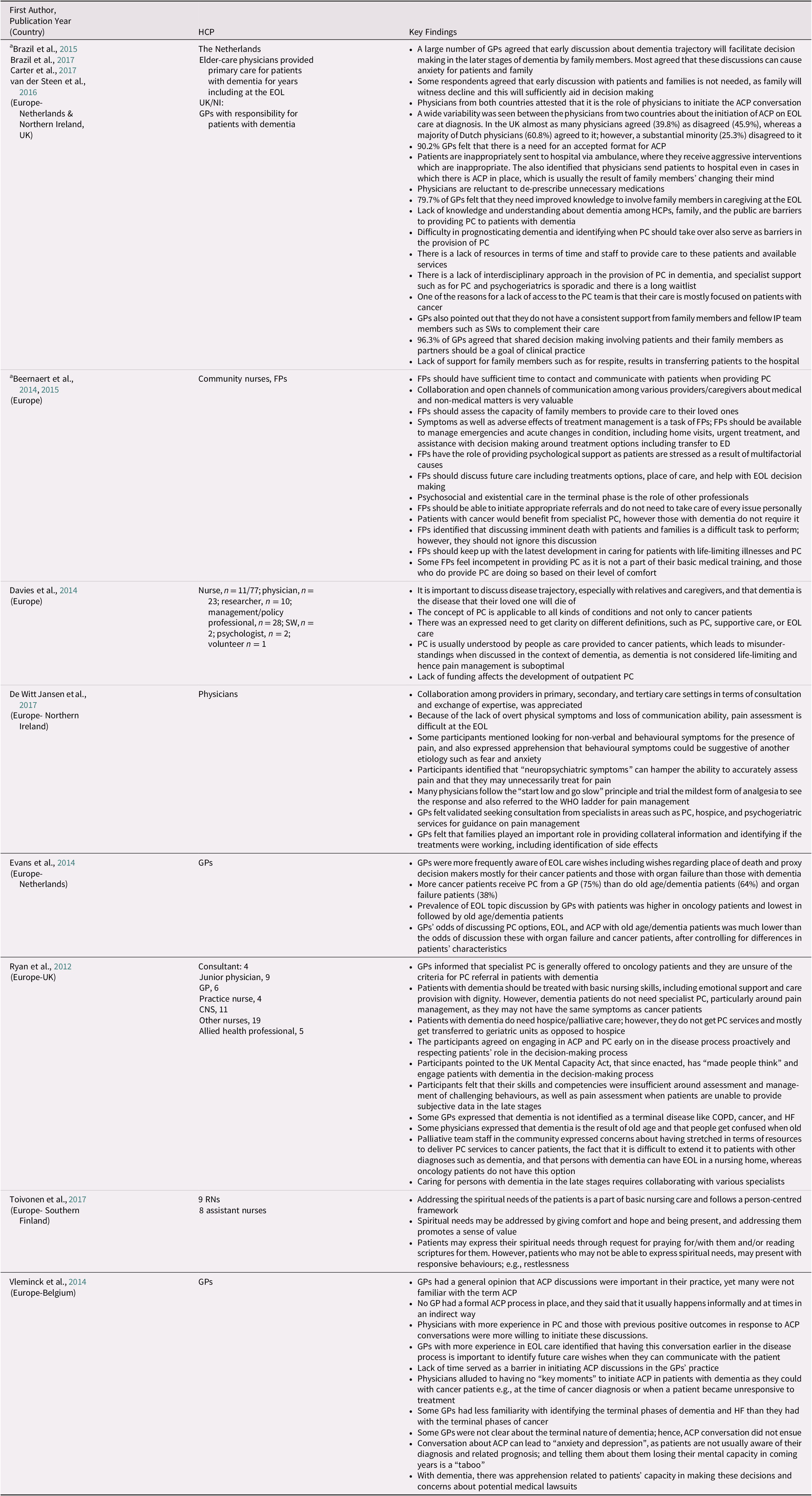
Note. aDenotes study presented in more than one article.
ACP = advance care planning; CNS = clinical nurse specialist; COPD = chronic obstructive pulmonary disease; ED = emergency department; EOL = end of life; FP = family physician; GP = general practitioner; HCP = health care practitioner; HF = heart failure; NI = Northern Ireland; PC = palliative care; PCP = primary care provider; WHO = World Health Organization; IP = interprofessional; SW = social worker.
ACP
Six of the eight studies highlighted ACP as part of a palliative approach (Beernaert et al., Reference Beernaert, Deliens, Vleminck, Devroey, Pardon and Den Block2014; Brazil et al., Reference Brazil, Carter, Galway, Watson and van der Steen2015; Davies et al., Reference Davies, Maio, van Riet Paap, Mariani, Jaspers and Sommerbakk2014; Evans et al., Reference Evans, Pasman, Donker, Deliens, Van den Block and Onwuteaka-Philipsen2014; Ryan et al., Reference Ryan, Gardiner, Bellamy, Gott and Ingleton2012; Vleminck et al., Reference Vleminck, Pardon, Beernaert, Deschepper, Houttekier and Audenhove2014). The findings were mixed regarding the appropriate timing of conducting ACP discussions. Many physicians agreed that early discussions promote the person’s role in the decision-making process and provide the opportunity to express their wishes while they can communicate them (Beernaert et al., Reference Beernaert, Deliens, Vleminck, Devroey, Pardon and Den Block2014; Davies et al., Reference Davies, Maio, van Riet Paap, Mariani, Jaspers and Sommerbakk2014; Ryan et al., Reference Ryan, Gardiner, Bellamy, Gott and Ingleton2012; Vleminck et al., Reference Vleminck, Pardon, Beernaert, Deschepper, Houttekier and Audenhove2014). Conversely, some physicians had reservations about early ACP discussions, believing that the caregivers need to experience the decline in the advanced stages to help with treatment decisions (Brazil et al., Reference Brazil, Carter, Galway, Watson and van der Steen2015; Vleminck et al., Reference Vleminck, Pardon, Beernaert, Deschepper, Houttekier and Audenhove2014). Many participants raised the concern that ACP discussions may cause anxiety among patients and caregivers and take away hope (Beernaert et al., Reference Beernaert, Deliens, Vleminck, Devroey, Pardon and Den Block2014; Brazil et al., Reference Brazil, Carter, Galway, Watson and van der Steen2015; Vleminck et al., Reference Vleminck, Pardon, Beernaert, Deschepper, Houttekier and Audenhove2014). Furthermore, physicians underlined that their lack of training leads to challenges with diagnosing a person in the early stages and projecting its trajectory, serving as a barrier to ACP discussions (Beernaert et al., Reference Beernaert, Deliens, Vleminck, Devroey, Pardon and Den Block2014; Brazil et al., Reference Brazil, Carter, Galway, Watson and van der Steen2015; Vleminck et al., Reference Vleminck, Pardon, Beernaert, Deschepper, Houttekier and Audenhove2014).
Pain and symptom management
This was highlighted in all studies except one (Vleminck et al., Reference Vleminck, Pardon, Beernaert, Deschepper, Houttekier and Audenhove2014). Concerning challenges in managing pain and other symptoms, physicians expressed difficulty in identifying and assessing distressing symptoms in persons with advanced dementia (Davies et al., Reference Davies, Maio, van Riet Paap, Mariani, Jaspers and Sommerbakk2014; De Witt Jansen et al., Reference De Witt Jansen, Brazil, Passmore, Buchanan, Maxwell and McIlfatrick2017; Ryan et al., Reference Ryan, Gardiner, Bellamy, Gott and Ingleton2012). These challenges result from a person’s lack of communication abilities to describe troubling symptoms, which sometimes result in responsive behaviours. Physicians expressed difficulty identifying the etiology of behavioural symptoms and concern that they do not want to medicate patients for the wrong reasons (Davies et al., Reference Davies, Maio, van Riet Paap, Mariani, Jaspers and Sommerbakk2014; De Witt Jansen et al., Reference De Witt Jansen, Brazil, Passmore, Buchanan, Maxwell and McIlfatrick2017; Ryan et al., Reference Ryan, Gardiner, Bellamy, Gott and Ingleton2012; Toivonen et al., Reference Toivonen, Charalambous and Suhonen2017). Practitioners, therefore, emphasized the role of caregivers for the assessment of distressing symptoms as well as response to treatments (De Witt Jansen et al., Reference De Witt Jansen, Brazil, Passmore, Buchanan, Maxwell and McIlfatrick2017; Ryan et al., Reference Ryan, Gardiner, Bellamy, Gott and Ingleton2012).
Participants indicated a lack of resources and personnel to optimize symptom management in the community (Brazil et al., Reference Brazil, Carter, Galway, Watson and van der Steen2015). They highlighted that caring for persons with dementia requires collaboration and open channels of communication among various specialists including palliative, psychogeriatric, and hospice care, as well as sectors for consultation and seamless care transitions (Beernaert et al., Reference Beernaert, Deliens, Vleminck, Devroey, Pardon and Den Block2014; Davies et al., Reference Davies, Maio, van Riet Paap, Mariani, Jaspers and Sommerbakk2014; De Witt Jansen et al., Reference De Witt Jansen, Brazil, Passmore, Buchanan, Maxwell and McIlfatrick2017; Ryan et al., Reference Ryan, Gardiner, Bellamy, Gott and Ingleton2012).
Psychosocial and spiritual care
Seven of the eight studies related to practitioners’ perspectives identified psychosocial support as an essential feature of a palliative approach in dementia care, whereas only two studies explicitly mentioned the importance of spiritual care (Brazil et al., Reference Brazil, Carter, Galway, Watson and van der Steen2015; Toivonen et al., Reference Toivonen, Charalambous and Suhonen2017).
Participants in one study reported that persons with dementia should be treated with basic nursing skills that include psychosocial and emotional support (Ryan et al., Reference Ryan, Gardiner, Bellamy, Gott and Ingleton2012). Whereas participants in several other studies indicated that it is the role of the physicians to address the needs requiring psychosocial support (Beernaert et al., Reference Beernaert, Deliens, Vleminck, Devroey, Pardon and Den Block2014; Brazil et al., Reference Brazil, Carter, Galway, Watson and van der Steen2015; Ryan et al., Reference Ryan, Gardiner, Bellamy, Gott and Ingleton2012). Physicians also pointed to a lack of funding for interdisciplinary teams to complement their care in supporting persons with dementia and caregivers at home (Brazil et al., Reference Brazil, Carter, Galway, Watson and van der Steen2015; Davies et al., Reference Davies, Maio, van Riet Paap, Mariani, Jaspers and Sommerbakk2014; Ryan et al., Reference Ryan, Gardiner, Bellamy, Gott and Ingleton2012). Physicians expressed frustration about the difficulty of acquiring community support for informal caregivers such as respite care to relieve their stress, resulting in unnecessary hospital transfers (Brazil et al., Reference Brazil, Carter, Galway, Watson and van der Steen2015; Carduff et al., Reference Carduff, Jarvis, Highet, Finucane, Kendall and Harrison2016). One study also highlighted the need for the integration of health and social care services for the optimal delivery of a palliative approach (Davies et al., Reference Davies, Maio, van Riet Paap, Mariani, Jaspers and Sommerbakk2014).
The process of shared decision making
The shared decision-making process was highlighted in six of eight studies addressing the perspectives and experiences of physicians and nurses (Brazil et al., Reference Brazil, Carter, Galway, Watson and van der Steen2015; Davies et al., Reference Davies, Maio, van Riet Paap, Mariani, Jaspers and Sommerbakk2014; De Witt Jansen et al., Reference De Witt Jansen, Brazil, Passmore, Buchanan, Maxwell and McIlfatrick2017; Evans et al., Reference Evans, Pasman, Donker, Deliens, Van den Block and Onwuteaka-Philipsen2014; Ryan et al., Reference Ryan, Gardiner, Bellamy, Gott and Ingleton2012; Vleminck et al., Reference Vleminck, Pardon, Beernaert, Deschepper, Houttekier and Audenhove2014). Participants recognized that shared decision making involving patients and their caregivers as partners should be a goal of clinical practice (Brazil et al., Reference Brazil, Carter, Galway, Watson and van der Steen2015; Ryan et al., Reference Ryan, Gardiner, Bellamy, Gott and Ingleton2012). They perceived that persons with dementia should be engaged in the conversation about their future care because of the impending loss of decisional capacity, hence acknowledging the patients’ role in decision making (Brazil et al., Reference Brazil, Carter, Galway, Watson and van der Steen2015; Ryan et al., Reference Ryan, Gardiner, Bellamy, Gott and Ingleton2012; Vleminck et al., Reference Vleminck, Pardon, Beernaert, Deschepper, Houttekier and Audenhove2014). Shared decision making also involved engaging caregivers in the late stages for the purpose of identifying treatment options according to the best interests of the person living with dementia (Davies et al., Reference Davies, Maio, van Riet Paap, Mariani, Jaspers and Sommerbakk2014; De Witt Jansen et al., Reference De Witt Jansen, Brazil, Passmore, Buchanan, Maxwell and McIlfatrick2017; Evans et al., Reference Evans, Pasman, Donker, Deliens, Van den Block and Onwuteaka-Philipsen2014; Ryan et al., Reference Ryan, Gardiner, Bellamy, Gott and Ingleton2012).
Question 2: Impact of a Palliative Approach in Dementia Care
Of the 17 studies, 9 reported on the impact of a palliative approach in the care of older adults with dementia in primary care settings and examined a variety of interventions and outcome measures (Carduff et al., Reference Carduff, Jarvis, Highet, Finucane, Kendall and Harrison2016; Clevenger et al., Reference Clevenger, Cellar, Kovaleva, Medders and Hepburn2018; Daaleman et al., Reference Daaleman, Ernecoff, Kistler, Reid, Reed and Hanson2019; Holley et al., Reference Holley, Gorawara-Bhat, Dale, Hemmerich and Cox-Hayley2009; Hum et al., Reference Hum, Wu, Ali, Leong, Chin and Lee2018; London et al., Reference London, McSkimming, Drew, Quinn and Carney2005; Nakanishi et al., Reference Nakanishi, Hirooka, Morimoto and Nishida2017; Sternberg et al., Reference Sternberg, Sabar, Katz, Segal, Fux-Zach and Grofman2019; Treloar et al., Reference Treloar, Crugel and Adamis2009) (See Table 3. for details on these outcomes). Eight of nine studies involved patients in the advanced stage of the disease, whereas one did not report the dementia stage (Daaleman et al., Reference Daaleman, Ernecoff, Kistler, Reid, Reed and Hanson2019). The outcomes describing the impact of a palliative approach were focused on the impacts on patient-related outcomes, most of which were reported by caregivers and/or assessed by health care practitioners, as described in the following paragraphs (Clevenger et al., Reference Clevenger, Cellar, Kovaleva, Medders and Hepburn2018; Holley et al., Reference Holley, Gorawara-Bhat, Dale, Hemmerich and Cox-Hayley2009; London et al., Reference London, McSkimming, Drew, Quinn and Carney2005; Nakanishi et al., Reference Nakanishi, Hirooka, Morimoto and Nishida2017; Sternberg et al., Reference Sternberg, Sabar, Katz, Segal, Fux-Zach and Grofman2019; Treloar et al., Reference Treloar, Crugel and Adamis2009); caregiver-related outcomes (Carduff et al., Reference Carduff, Jarvis, Highet, Finucane, Kendall and Harrison2016; Clevenger et al., Reference Clevenger, Cellar, Kovaleva, Medders and Hepburn2018; Holley et al., Reference Holley, Gorawara-Bhat, Dale, Hemmerich and Cox-Hayley2009; Sternberg et al., Reference Sternberg, Sabar, Katz, Segal, Fux-Zach and Grofman2019; Treloar et al., Reference Treloar, Crugel and Adamis2009); and health care utilization (Clevenger et al., Reference Clevenger, Cellar, Kovaleva, Medders and Hepburn2018; Daaleman et al., Reference Daaleman, Ernecoff, Kistler, Reid, Reed and Hanson2019; Holley et al., Reference Holley, Gorawara-Bhat, Dale, Hemmerich and Cox-Hayley2009; Hum et al., Reference Hum, Wu, Ali, Leong, Chin and Lee2018; London et al., Reference London, McSkimming, Drew, Quinn and Carney2005; Sternberg et al., Reference Sternberg, Sabar, Katz, Segal, Fux-Zach and Grofman2019; Treloar et al., Reference Treloar, Crugel and Adamis2009). Table 3 presents significant findings from the studies related to the impact of this approach.
Table 3. Studies addressing the impact of palliative approach in dementia care
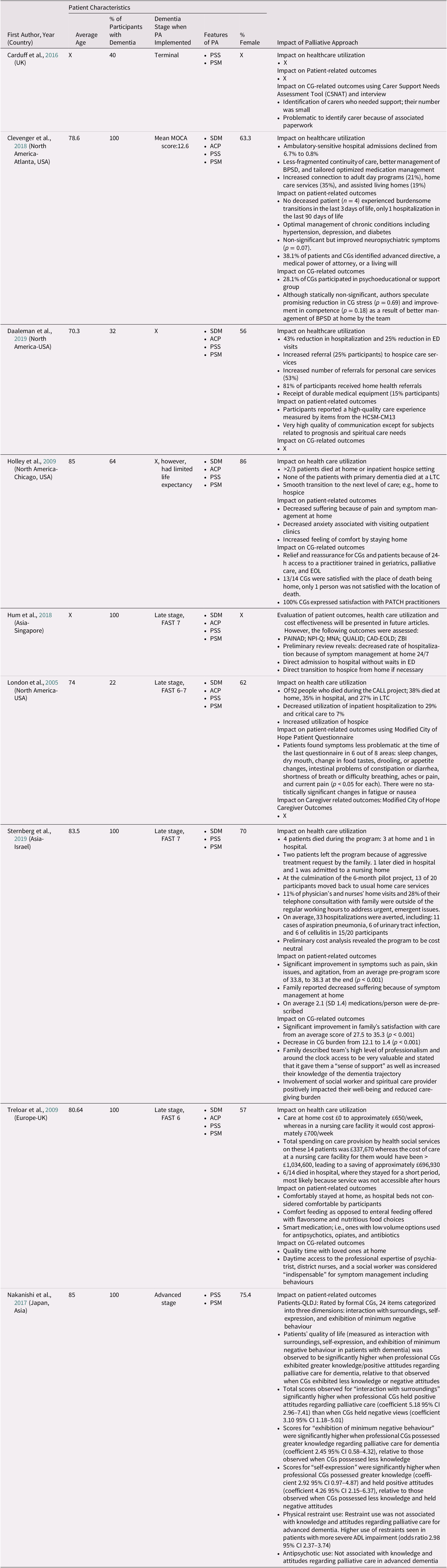
Note. ✓ = Yes; X = not mentioned/reported
ACP = advance care planning; ADL = activities of daily living; BPSD = Behavioral and Psychological Symptoms of Dementia; CAD-EOLD = Comfort Assessment in Dying With Dementia; CALL Project = Comprehensive, Adaptable, Life- Affirming, Longitudinal (CALL) palliative care project; CG = caregiver; CI = confidence interval; ED = emergency department; EOL: end of life; FAST = Functional Assessment Staging; HCSMCM13: Home Care Satisfaction Measure-Care Management Service; LTC = long-term care; MNA: Mini Nutritional Assessment; MOCA = Montreal Cognitive Assessment; NPI-Q: Neuropsychiatric Inventory Questionnaire, severity domain; caregiver distress domain; PAINAD: Pain Assessment in Advanced Dementia; PATCH = Palliative Access Through Care at Home; PSM = pain and symptom management; PSS = psychosocial and spiritual support; QLDJ = Japanese QOL instrument for older adults experiencing dementia; QUALID = Quality of Life in Late-Stage Dementia; SDM = Shared Decision Making; ZBI = Zarit Burden Interview to assess impact of caregiving.
Impact of a palliative approach on patient-related outcomes
Several researchers focused on patient-related outcomes such as a decrease in suffering, increased ability to stay home (Clevenger et al., Reference Clevenger, Cellar, Kovaleva, Medders and Hepburn2018; Holley et al., Reference Holley, Gorawara-Bhat, Dale, Hemmerich and Cox-Hayley2009; Hum et al., Reference Hum, Wu, Ali, Leong, Chin and Lee2018; London et al., Reference London, McSkimming, Drew, Quinn and Carney2005; Treloar et al., Reference Treloar, Crugel and Adamis2009), and improvement in the quality of life (Hum et al., Reference Hum, Wu, Ali, Leong, Chin and Lee2018; Nakanishi et al., Reference Nakanishi, Hirooka, Morimoto and Nishida2017). Overall, investigators reported that optimization of pain and symptom management including the use of oral feeding as opposed to enteral nutrition (Treloar et al., Reference Treloar, Crugel and Adamis2009) at home in the advanced stages led to a reduction in overall suffering (Clevenger et al., Reference Clevenger, Cellar, Kovaleva, Medders and Hepburn2018; Holley et al., Reference Holley, Gorawara-Bhat, Dale, Hemmerich and Cox-Hayley2009; London et al., Reference London, McSkimming, Drew, Quinn and Carney2005; Sternberg et al., Reference Sternberg, Sabar, Katz, Segal, Fux-Zach and Grofman2019; Treloar et al., Reference Treloar, Crugel and Adamis2009). Only one study reported on medication de-prescribing (Sternberg et al., Reference Sternberg, Sabar, Katz, Segal, Fux-Zach and Grofman2019).
Clevenger et al. (Reference Clevenger, Cellar, Kovaleva, Medders and Hepburn2018) examined the Integrated Memory Care Clinic (IMCC) led by advanced practice nurses that delivered interdisciplinary comprehensive primary and behavioural care management around the clock at home. The program led to the identification and management of chronic diseases, identification of advanced directives (38%), and non-significant improvement in neuropsychiatric symptoms severity (p = 0.07) as well as caregiver distress (p = 0.69) related to behavioural symptoms. Sternberg and colleagues examined a home hospice program offered to older adults with advanced dementia, which also included after-hour service (Sternberg et al., Reference Sternberg, Sabar, Katz, Segal, Fux-Zach and Grofman2019). The program led to statistically significant improvement in participants’ symptom management scores (p ≤ 0.001) at the end of the program when compared with the baseline scores; also, the program led to an average medication de-prescribing of 2.1 (standard deviation [SD] 1.4) unnecessary medications per person.
One study used a patient self-reported tool called the Modified City of Hope questionnaire to assess the improvement in physical symptoms (p ≤ 0.05) over time with interventions provided through a palliative care program at home (London et al., Reference London, McSkimming, Drew, Quinn and Carney2005). Participants included patients in the advanced stages of various diseases, including dementia. However, authors do not provide details on how data were acquired from these individuals, given that loss of communication abilities is inevitable in advanced dementia (Fazel, Hope, & Jacoby, Reference Fazel, Hope and Jacoby2000). Hence, there is a concern related to the threat to internal validity in terms of how the patients completed the questionnaire, and it is challenging to contextualize the findings. In their qualitative analysis, Holley et al. found that a decrease in suffering and an increase in comfort resulted from the optimal management of issues at home, such as sleep problems, dry mouth, constipation or diarrhea, breathing concerns, and pains, as well as decrease in psychological and physical distress associated with attending outpatient clinic appointments, because care was provided at home (Holley et al., Reference Holley, Gorawara-Bhat, Dale, Hemmerich and Cox-Hayley2009). Nakanishi and colleagues measured quality of life as an interaction with surroundings, self-expression, and exhibition of minimum negative behaviour in patients with dementia (Nakanishi et al., Reference Nakanishi, Hirooka, Morimoto and Nishida2017). The participants were professional caregivers to community-dwelling older adults with advanced dementia; for example, nurses and nursing assistants, who completed these measures. Researchers found that patients’ quality of life was significantly higher (p ≤ 0.05) when professional caregivers exhibited greater knowledge of dementia or possessed positive attitudes regarding palliative care in dementia. Conversely, the investigators also found that the use of physical restraints was higher in patients with severe impairment in the activities of daily living regardless of the professional caregivers’ knowledge and attitudes regarding palliative care for advanced dementia (Odds ratio 2.98 95% confidence interval [CI] 2.37–3.74).
Impact of a palliative approach on caregiver outcomes
Five studies reported on caregiver outcomes (Carduff et al., Reference Carduff, Jarvis, Highet, Finucane, Kendall and Harrison2016; Clevenger et al., Reference Clevenger, Cellar, Kovaleva, Medders and Hepburn2018; Holley et al., Reference Holley, Gorawara-Bhat, Dale, Hemmerich and Cox-Hayley2009; Sternberg et al., Reference Sternberg, Sabar, Katz, Segal, Fux-Zach and Grofman2019; Treloar et al., Reference Treloar, Crugel and Adamis2009). Main outcomes measured included: identification of carers needing support (n = 1), caregivers’ participation in psychoeducation (n = 1), caregiver stress (n = 2), caregiver competence (n = 1), caregivers’ satisfaction with care at home (n = 3), and quality time spent at home (n = 1). The investigators in one United Kingdom-based study developed a model to identify, assess, and support carers in primary care practice (Carduff et al., Reference Carduff, Jarvis, Highet, Finucane, Kendall and Harrison2016). They found that carers valued the connection with their primary care practice. However, because of time-consuming paperwork to acquire support, only 36 per cent of the eligible carers participated in this program, whereas Clevenger and colleagues (Reference Clevenger, Cellar, Kovaleva, Medders and Hepburn2018) provided caregivers opportunities to engage in psychoeducation and support groups, where 38.1 per cent of caregivers participated. Although statistically non-significant, there was a reduction in caregiver stress (p = 0.69) and an improvement in caregiver competence (p = 0.18) in managing responsive behaviours in consultation with the IMCC team (Clevenger et al., Reference Clevenger, Cellar, Kovaleva, Medders and Hepburn2018).
Caregivers reported a sense of relief and support because of the 24-hour access to practitioners with training in geriatrics, palliative care, and end-of-life care for symptom management (Holley et al., Reference Holley, Gorawara-Bhat, Dale, Hemmerich and Cox-Hayley2009; Sternberg et al., Reference Sternberg, Sabar, Katz, Segal, Fux-Zach and Grofman2019), and also reported an increase in their knowledge of the dementia trajectory (Sternberg et al., Reference Sternberg, Sabar, Katz, Segal, Fux-Zach and Grofman2019). In another study, caregivers found that access to professionals, including a social worker and spiritual care provider, had a positive impact on their well-being and lessened their caregiving burden (Sternberg et al., Reference Sternberg, Sabar, Katz, Segal, Fux-Zach and Grofman2019; Treloar et al., Reference Treloar, Crugel and Adamis2009).
Impact of a palliative approach on health care utilization
Seven studies reported an impact on health care utilization, where specific outcomes included: death at home versus in hospital and/or long-term care homes (Holley et al., Reference Holley, Gorawara-Bhat, Dale, Hemmerich and Cox-Hayley2009; London et al., Reference London, McSkimming, Drew, Quinn and Carney2005; Sternberg et al., Reference Sternberg, Sabar, Katz, Segal, Fux-Zach and Grofman2019; Treloar et al., Reference Treloar, Crugel and Adamis2009), decrease in emergency department visits and hospitalization (Clevenger et al., Reference Clevenger, Cellar, Kovaleva, Medders and Hepburn2018; Daaleman et al., Reference Daaleman, Ernecoff, Kistler, Reid, Reed and Hanson2019; London et al., Reference London, McSkimming, Drew, Quinn and Carney2005; Sternberg et al., Reference Sternberg, Sabar, Katz, Segal, Fux-Zach and Grofman2019), reduction in health care costs (Treloar et al., Reference Treloar, Crugel and Adamis2009), smooth care transitions including to hospice (Clevenger et al., Reference Clevenger, Cellar, Kovaleva, Medders and Hepburn2018; Daaleman et al., Reference Daaleman, Ernecoff, Kistler, Reid, Reed and Hanson2019; Holley et al., Reference Holley, Gorawara-Bhat, Dale, Hemmerich and Cox-Hayley2009; Hum et al., Reference Hum, Wu, Ali, Leong, Chin and Lee2018), and care coordination for the receipt of appropriate services such as day programs (Clevenger et al., Reference Clevenger, Cellar, Kovaleva, Medders and Hepburn2018).
Two studies reported that the majority of patients died at home as a result of optimal symptom management (Clevenger et al., Reference Clevenger, Cellar, Kovaleva, Medders and Hepburn2018; Holley et al., Reference Holley, Gorawara-Bhat, Dale, Hemmerich and Cox-Hayley2009; Treloar et al., Reference Treloar, Crugel and Adamis2009). Two studies reported on the cost of the program; one reported considerable savings when the cost of care was compared between home and a nursing care facility for the 14 participants in the program (Treloar et al., Reference Treloar, Crugel and Adamis2009), whereas one reported that preliminary cost analysis revealed the program to be cost neutral (Sternberg et al., Reference Sternberg, Sabar, Katz, Segal, Fux-Zach and Grofman2019). Authors reported a decrease in hospitalization rate and improved care transitions because of optimal symptoms management at home (Hum et al., Reference Hum, Wu, Ali, Leong, Chin and Lee2018; London et al., Reference London, McSkimming, Drew, Quinn and Carney2005; Sternberg et al., Reference Sternberg, Sabar, Katz, Segal, Fux-Zach and Grofman2019) including after hours (Hum et al., Reference Hum, Wu, Ali, Leong, Chin and Lee2018; Sternberg et al., Reference Sternberg, Sabar, Katz, Segal, Fux-Zach and Grofman2019). For example, in one study, the rate of hospitalization decreased to 29 per cent, and critical care admission decreased to 7 per cent among the participants when compared with the much higher national averages of 71 and 36 per cent, respectively (London et al., Reference London, McSkimming, Drew, Quinn and Carney2005), whereas in another study, hospital admissions declined to 0.8 per cent from 6.7 per cent (Clevenger et al., Reference Clevenger, Cellar, Kovaleva, Medders and Hepburn2018). In comparison, in one study, 6 of the 14 participants died in the hospital following a short hospitalization (Treloar et al., Reference Treloar, Crugel and Adamis2009). The authors speculated that the symptoms could have been alleviated had the service been available after hours. Interestingly, Sternberg et al. reported a 6-month mortality of 20 per cent in the participants in their pilot hospice program, declaring that this was less than predicted in the literature, suggesting that existing survival prognosis tools for persons living with advanced dementia have inconsistent predictive validity of 6-month mortality (Sternberg et al., Reference Sternberg, Sabar, Katz, Segal, Fux-Zach and Grofman2019).
Discussion
The review included 17 studies, the majority of which were published recently, pointing to the relevance and the growing awareness of an integrated palliative approach in caring for persons living with dementia in primary care settings. No studies were found that looked at the integration of a palliative approach in persons with mild to moderate dementia. As such, the findings in this article relate to the integration of a palliative approach in advanced dementia, which appears to be most common. Primary care providers are reluctant to initiate ACP discussions because of the barriers related to the unpredictable and protracted trajectory of dementia, leading to difficulty in prognostication and concerns about stripping hope and causing psychological distress, as well as lack of training and experience in caring for the persons with dementia (Beernaert et al., Reference Beernaert, Deliens, Vleminck, Devroey, Pardon and Den Block2014; Brazil et al., Reference Brazil, Carter, Galway, Watson and van der Steen2015; Vleminck et al., Reference Vleminck, Pardon, Beernaert, Deschepper, Houttekier and Audenhove2014). Primary care physicians worry about the ability to offer appropriate symptom management and psychosocial support to patients and caregivers (Brazil et al., Reference Brazil, Carter, Galway, Watson and van der Steen2015; Davies et al., Reference Davies, Maio, van Riet Paap, Mariani, Jaspers and Sommerbakk2014; Ryan et al., Reference Ryan, Gardiner, Bellamy, Gott and Ingleton2012). This is because of a lack of interdisciplinary approach, collaboration among specialties and sectors (Beernaert et al., Reference Beernaert, Deliens, Vleminck, Devroey, Pardon and Den Block2014; Davies et al., Reference Davies, Maio, van Riet Paap, Mariani, Jaspers and Sommerbakk2014; De Witt Jansen et al., Reference De Witt Jansen, Brazil, Passmore, Buchanan, Maxwell and McIlfatrick2017; Ryan et al., Reference Ryan, Gardiner, Bellamy, Gott and Ingleton2012), and integration of health and social services (Davies et al., Reference Davies, Maio, van Riet Paap, Mariani, Jaspers and Sommerbakk2014).
In this review, we have operationalized a definition of a palliative approach in the context of dementia and used this definition to scope the existing literature in this area. There is variability in the literature regarding what constitutes an integrated palliative approach to care for older adults with dementia at various stages within their trajectory from the perspective of non-palliative specialists. Therefore, setting out the four main components of a palliative approach; that is, ACP, pain and symptoms management, psychosocial and spiritual support, and the process of shared decision making, was a necessary first step. Given the lack of clarity as to the core components of a palliative approach in the care of older adults with dementia in primary care settings, future investigation is required to test this definition.
The uncertainty related to the appropriate timing of the integration of a palliative approach in dementia care was a prominent theme identified in this review. It is recommended that a palliative approach should be integrated early with chronic disease management to enhance the quality of life of patients and their caregivers throughout the disease trajectory and not just at the end of life (Canadian Hospice Palliative Care Association, 2015; Durepos et al., Reference Durepos, Wickson-Griffiths, Hazzan, Kaasalainen, Vastis and Battistella2017; Hines et al., Reference Hines, McCrow, Abbey, Foottit, Wilson and Franklin2011). However, there remain substantial gaps in integrating a palliative approach with chronic disease management, resulting in aggressive treatment and investigations at the end of life leading to compromised care experiences (Durepos et al., Reference Durepos, Wickson-Griffiths, Hazzan, Kaasalainen, Vastis and Battistella2017). Persons with mild to moderate dementia can evaluate, interpret, and derive meaning in their lives (Cheong et al., Reference Cheong, Fisher, Goh, Ng, Koh and Yap2015; Hegde & Ellajosyula, Reference Hegde and Ellajosyula2016), making early stages a highly appropriate time for engaging patients and their care partners in discussions about dementia trajectory, care approaches, goals, and wishes for ongoing and future care. Nevertheless, how early after the diagnosis should these discussions commence remains a question that requires further exploration.
Advance care planning can promote patients’ autonomy and prepare their caregivers for future care decisions. We found that primary care practitioners are concerned about causing anxiety and destroying a person’s hope with the integration of a palliative approach in dementia care, specifically when discussing ACP. However, in other populations, early integration of palliative care that included ACP improved quality of life and reduced depression symptoms in participants (Hoerger et al., Reference Hoerger, Greer, Jackson, Park, Pirl and El-Jawahri2018; Temel et al., Reference Temel, Greer, Muzikansky, Gallagher, Admane and Jackson2010). Participants in these studies received less aggressive care at the end of life than those in the standard care group (Temel et al., Reference Temel, Greer, Muzikansky, Gallagher, Admane and Jackson2010). Such prospective studies are also needed for persons with early stages of dementia, to examine the short-term and long-term impact on clinically significant outcomes.
A significant finding of our review was related to a lack of access to community agencies to enhance psychosocial support for patients and caregivers. Community-dwelling older adults with dementia live with informal caregivers and receive more care from them than from paid caregivers (Alzheimer’s Association, 2014). Although anticipatory grief was not specifically examined in any of the included studies, it is frequently experienced by informal caregivers of persons with dementia throughout the course of the disease, and it is associated with an increased level of caregiving burden and depression (Garand et al., Reference Garand, Lingler, Deardorf, DeKosky, Schulz and Reynolds2012). As previously identified, one of the main components of an integrated palliative approach is psychosocial and spiritual support for the patients and caregivers. Therefore, lack of identification and supports for their unmet needs could lead to burnout and portend unnecessary hospitalizations. Hence, it is crucial that primary care practitioners have access to interprofessional teams, including social workers and spiritual care providers throughout the dementia trajectory, to establish a comprehensive and coordinated plan of care. It is also imperative to recognize that an integrated care approach requires aligning the health and social care systems, as health and social care needs are inextricably connected (McGilton et al., Reference McGilton, Vellani, Yeung, Chishtie, Commisso and Ploeg2018). Hence, an unmet psychosocial need may potentially minimize the effect of a well-planned health intervention.
The process of shared decision making was identified as an essential feature to actualize an integrated palliative approach in dementia care. Shared decision making requires building rapport with patients and caregivers, as well as respecting a person’s capacity and dependence on others (Elwyn et al., Reference Elwyn, Frosch, Thomson, Joseph-Williams, Lloyd and Kinnersley2012). Decision-making capacity worsens as dementia progresses, making it more critical to engage the caregivers at the outset of dementia, as their role is instrumental and dynamic in optimizing care for persons with dementia through its progression. By means of the opportunities to engage in the process of shared decision making, caregivers can learn about the care wishes and values of the older adults they care for, which can potentialiy result in increased decision-making confidence when the person with dementia loses their ability to make personal care decisions, as well as during the periods of crisis.
We identified nine studies that examined the integration of a palliative approach in the care of older adults with dementia in primary care settings. The outcomes were related to impact on the patients, such as a decrease in suffering as a result of pain and symptom management at home (Clevenger et al., Reference Clevenger, Cellar, Kovaleva, Medders and Hepburn2018; Holley et al., Reference Holley, Gorawara-Bhat, Dale, Hemmerich and Cox-Hayley2009; Hum et al., Reference Hum, Wu, Ali, Leong, Chin and Lee2018; London et al., Reference London, McSkimming, Drew, Quinn and Carney2005; Sternberg et al., Reference Sternberg, Sabar, Katz, Segal, Fux-Zach and Grofman2019; Treloar et al., Reference Treloar, Crugel and Adamis2009), on the caregivers, such as satisfaction with care (Holley et al., Reference Holley, Gorawara-Bhat, Dale, Hemmerich and Cox-Hayley2009; Sternberg et al., Reference Sternberg, Sabar, Katz, Segal, Fux-Zach and Grofman2019; Treloar et al., Reference Treloar, Crugel and Adamis2009), and on health care utilization, such as a decrease in inpatient hospitalization (Clevenger et al., Reference Clevenger, Cellar, Kovaleva, Medders and Hepburn2018; Daaleman et al., Reference Daaleman, Ernecoff, Kistler, Reid, Reed and Hanson2019; London et al., Reference London, McSkimming, Drew, Quinn and Carney2005; Sternberg et al., Reference Sternberg, Sabar, Katz, Segal, Fux-Zach and Grofman2019). The synthesis of outcomes for a palliative approach in dementia care presented methodological challenges. This was noted in another systematic review that evaluated randomized controlled trials examining the efficacy of a palliative approach in advanced dementia (Sampson et al., Reference Sampson, Ritchie, Lai, Raven and Blanchard2005). The investigators in this review found that in advanced dementia, validated measures, including pain scales and caregiver reports of symptom control and satisfaction, may be inaccurate. Furthermore, patients with late stages of dementia have verbal difficulty, and scales measuring satisfaction with care usually have positive responses, resulting in skewed distribution (Volicer, Hurley, & Blasi, Reference Volicer, Hurley and Blasi2001). Our findings also raise questions about the use and efficacy of tools to measure outcomes in studies of impact, as eight of nine studies addressing the impacts of this approach recruited patients in the advanced stage. There remains a need to identify and validate appropriate measures sensitive to palliative approach interventions throughout the trajectory of the illness; for example, using behaviour-based tools when verbal communication is no longer accessible. Sternberg at al. reported a lack of survival tools with consistent predictive validity of 6-month mortality for advanced dementia; as a result, over 60 per cent of participants in the study were transferred back to regular home care service at the culmination of the pilot home-based hospice project (Sternberg et al., Reference Sternberg, Sabar, Katz, Segal, Fux-Zach and Grofman2019). This is likely related to the unpredictable and protracted trajectory of dementia, complicated by the presence of multi-morbidities and a high level of frailty. Hence, placing a person with dementia in a numerical range of prognosis for the receipt of optimal care in the community does not seem to provide patient-centred care. Therefore, it is vital to acknowledge the terminal and progressive nature of dementia at the outset to customize care per unique individual needs and circumstances, regardless of the dementia stage.
It is important that primary care clinicians mindfully incorporate each of the four components of palliative approach laid out in this review in caring for persons living with dementia in community throughout the course of the disease. This would also acknowledge the definition of palliative care by the World Health Organization (WHO), which asserts that it is applicable early with the management of life-limiting conditions and aims to improve the quality of life of patients and caregivers by addressing their physical, psychosocial, and spiritual care needs (World Health Organization, 2020). The specific interventions for each of the four components of a palliative approach will differ with the progression of dementia, level of frailty, and individual needs of patients and caregivers. Also, the integrated palliative approach goes beyond the person’s death to providing for the bereavement care needs of the caregivers (Schulz et al., Reference Schulz, Mendelsohn, Haley, Mahoney, Allen and Zhang2003). As our findings suggest, clinicians will need to advance their knowledge and expertise on the complexity of dementia care, including communication skills to broach difficult topics with patients and caregivers such as the terminal and progressive nature of dementia, inevitable loss of communication abilities, and need for early ACP discussions.
Recommendations for Future Research and Clinical Practice
Future research should focus on longitudinal studies to establish the benefits of a palliative approach integrated over the trajectory of dementia, including for those persons in the early stage. Specific interventions with appropriate outcome measures need to be identified and validated. Also, there is a need to determine the timing at which a palliative approach should be integrated with dementia management that is tailored to individual preferences and values. Typically, older adults with dementia, especially those who are recipients of home and community care services (Mondor et al., Reference Mondor, Maxwell, Hogan, Bronskill, Gruneir and Lane2017), also have multiple chronic conditions. As it is, persons with dementia have an increased likelihood of hospitalizations with 3.68 times higher odds than those without dementia (Bynum et al., Reference Bynum, Rabins, Weller, Niefeld, Anderson and Wu2004). With each additional chronic disease, there is an even higher risk of frequent hospitalizations and visits to emergency departments (Mondor et al., Reference Mondor, Maxwell, Hogan, Bronskill, Gruneir and Lane2017). These exposures to the health care system can serve as opportune times for hospital and community-based clinicians to broach the subject of ACP, assess the need for psychosocial and spiritual support for patients and caregivers, and optimize pain and symptom management through the process of shared decision making.
Our findings suggest that health care providers in primary care practice must be trained and available to manage patients at home for an effective, integrated palliative approach in caring for their patients at all stages of dementia. Physicians in primary practice already have a lack of primary care resources and heavy workloads. Therefore, there is a need to innovate community-based interdisciplinary models of care delivery that address care and symptom management at home. These models should have the capacity to amalgamate health care provided by various sectors while coordinating services provided by health and social services; and optimizing support for patients as well as for informal caregivers (Cohn et al., Reference Cohn, Corrigan, Lynn, Meier, Miller and She-ga2017). Furthermore, primary care clinicians should be able know the components of the integrated palliative approach with dementia care to be able to measure its delivery and effectiveness in their setting in order to highlight their role in the delivery of palliative care at the system level and be recognized by the system planners (Shadd et al., Reference Shadd, Burge, Stajduhar, Cohen, Kelley and Pesut2013). Hence, future research should be designed by looking at indicators of an integrated palliative approach in caring for community- dwelling individuals with dementia in primary care.
In light of the growing number of older adults, the health care systems are presented with challenges whereby there is a shortage of practitioners who are well versed in caring for older adults. A large number of those who are providing care to this group of patients are critically underprepared to serve the needs of their older patients (Institute of Medicine Committee, 2008). Hence, there is tremendous potential to design and evaluate interdisciplinary models of care that may involve advanced practice nurses such as NPs. Studies examining the outcomes related to the care provided by NPs to residents of long-term care homes have revealed greater family satisfaction with end-of-life care (Liu, Guarino, & Lopez, Reference Liu, Guarino and Lopez2012) and reduction in the cost of care (Bauer, Reference Bauer2010).
Given the fact that the majority of community-dwelling older adults with dementia receive assistance with the activities of daily living from unpaid caregivers (Kasper, Freedman, Spillman, & Wolff, Reference Kasper, Freedman, Spillman and Wolff2015), future work should also involve an exploration of the perspective and experiences of caregivers related to this approach. Longitudinal studies need to be designed to explore the sources of anticipatory grief at different stages of dementia and specific interventions to address them. Finally, one of the barriers to the integration of a palliative approach in the care of older adults with dementia was primary care practitioners’ lack of education and experience in caring for this group of individuals. This is a concern and calls for the design and implementation of educational and capacity-building strategies included as part of the basic professional education, which should also be mandated as part of continuing education activities.
Strengths and Limitations
There is not a single agreed-upon conceptual framework of a palliative approach for persons with dementia through the illness trajectory, including the early stages, the strength of our study is that we consolidated and synthesized a model that focused on four consistent components. The scoping review results showed that the model we proposed was relevant, as most of the studies we found had at least three of the four features embedded in them; that is., ACP, pain and symptom management, psychosocial and spiritual support; and the process of shared decision making. Developing the definition of an integrated palliative approach from the existing literature was an important step to guide our search strategy, data extraction, and synthesis, because of a lack of clarity as to what constitutes this approach for persons living with dementia throughout the trajectory, and not just at the late stage. Our study had several limitations. We excluded studies involving other settings such as acute care or long-term care because of our inclusion criteria that the study needed to address palliative care principles for persons with dementia in primary care settings. Hence, of 2,153 abstracts, we only identified 17 that met the inclusion criteria. Although the review sheds light on the state of evidence on the topic of inquiry, it only includes studies published in English, potentially missing out on literature that may be available in other languages. Also, to capture all the relevant studies from the selected databases, we did not exclude studies based on the quality. This allowed us to present results that include lower quality studies, to be able to summarize the breadth of the available literature.
Conclusion
To our knowledge, this review is the first to operationalize the definition of a palliative approach in the care of older adults with dementia throughout the disease trajectory in primary care, which was necessary based on existing work which had focused on persons in the late stages of dementia or was developed for palliative experts. The findings of the review indicate that there is a lack of studies dealing with older adults with dementia in primary care settings, particularly in the early stages. Future research is needed to confirm whether the integration of a palliative approach early on in the dementia trajectory offers the opportunity to understand and honour a person’s wishes for present and future health care, prepare caregivers for making future care decisions, and increase the likelihood of receiving goal-concordant end-of-life care.
Acknowledgements
This research was supported by Maria and Walter Schroeder Institute for Brain Innovation and Recovery.
Supplementary Materials
To view supplementary material for this article, please visit http://doi.org/10.1017/S0714980821000349.







