Introduction
The management of frail older residents’ pharmacotherapy in long-term care (LTC) homes may be challenging for health care teams. In many countries, polypharmacy and potentially inappropriate medications are frequent in such settings (Tamura, Bell, Inaba, & Masaki, Reference Tamura, Bell, Inaba and Masaki2012). In Canada, in 2016, approximately 50 per cent of adults aged 65 and older living in LTC homes used 10 classes of medications or more. This proportion was approximately 25 per cent in older people living in the community (Canadian Institute for Health Information, 2018). Prior studies revealed that older adults living in LTC who use many medications have an increased risk of receiving potentially inappropriate medications (Rancourt et al., Reference Rancourt, Moisan, Baillargeon, Verreault, Laurin and Gregoire2004; Tamura et al., Reference Tamura, Bell, Inaba and Masaki2012). Polypharmacy and the use of potentially inappropriate medications in older adults are associated with increased morbidity, notably because of the increased risk of adverse events and medication interactions (Kim & Parish, Reference Kim and Parish2017), leading to a higher risk of falls (Bor et al., Reference Bor, Matuz, Csatordai, Szalai, Balint and Benko2017; Zia, Kamaruzzaman, & Tan, Reference Zia, Kamaruzzaman and Tan2015), emergency department visits (Jeon, Park, Han, & Kim, Reference Jeon, Park, Han and Kim2018; Wong, Marr, Kwan, Meiyappan, & Adcock, Reference Wong, Marr, Kwan, Meiyappan and Adcock2014), hospitalizations (Canadian Institute for Health Information, 2018; Jeon et al., Reference Jeon, Park, Han and Kim2018; Price, Holman, Sanfilippo, & Emery, Reference Price, Holman, Sanfilippo and Emery2014; Wang, Bell, Chen, Gilmartin-Thomas, & Ilomaki, Reference Wang, Bell, Chen, Gilmartin-Thomas and Ilomaki2018), or death (Dedhiya, Hancock, Craig, Doebbeling, & Thomas III, Reference Dedhiya, Hancock, Craig, Doebbeling and Thomas2010; Perri III et al., Reference Perri, Menon, Deshpande, Shinde, Jiang and Cooper2005). Given that almost 60 per cent of adverse medication events in LTC residents are preventable (Office of Inspector General, 2014), this emphasizes the importance of identifying effective interventions to reduce inappropriate medication use and associated adverse health outcomes among older LTC residents.
Various interventions applied by pharmacists, physicians, or a multidisciplinary team composed of physicians, pharmacists, and nurses have been developed and tested in an attempt to optimize the use of medications prescribed to older adults living in LTC: staff education (Alldred, Kennedy, Hughes, Chen, & Miller, Reference Alldred, Kennedy, Hughes, Chen and Miller2016; Forsetlund, Eike, Gjerberg, & Vist, Reference Forsetlund, Eike, Gjerberg and Vist2011; Loganathan, Singh, Franklin, Bottle, & Majeed, Reference Loganathan, Singh, Franklin, Bottle and Majeed2011; Marcum, Handler, Wright, & Hanlon, Reference Marcum, Handler, Wright and Hanlon2010), residents’ medication reviews (Forsetlund et al., Reference Forsetlund, Eike, Gjerberg and Vist2011; Alldred et al., Reference Alldred, Kennedy, Hughes, Chen and Miller2016; Loganathan et al., Reference Loganathan, Singh, Franklin, Bottle and Majeed2011; Marcum et al., Reference Marcum, Handler, Wright and Hanlon2010), multidisciplinary and multifaceted approaches (Alldred et al., Reference Alldred, Kennedy, Hughes, Chen and Miller2016; Loganathan et al., Reference Loganathan, Singh, Franklin, Bottle and Majeed2011; Marcum et al., Reference Marcum, Handler, Wright and Hanlon2010; Rankin et al., Reference Rankin, Cadogan, Patterson, Kerse, Cardwell and Bradley2018), and the use of clinical decision support technology (Alldred et al., Reference Alldred, Kennedy, Hughes, Chen and Miller2016; Loganathan et al., Reference Loganathan, Singh, Franklin, Bottle and Majeed2011; Marcum et al., Reference Marcum, Handler, Wright and Hanlon2010; Rankin et al., Reference Rankin, Cadogan, Patterson, Kerse, Cardwell and Bradley2018). However, mixed results were found concerning the effectiveness of these interventions to reduce inappropriate medication use or their effect on residents’ related health outcomes such as adverse events or hospital admissions (Nazir et al., Reference Nazir, Unroe, Tegeler, Khan, Azar and Boustani2013; Simonson & Feinberg, Reference Simonson and Feinberg2005; Alldred et al., Reference Alldred, Kennedy, Hughes, Chen and Miller2016; Forsetlund et al., Reference Forsetlund, Eike, Gjerberg and Vist2011; Loganathan et al., Reference Loganathan, Singh, Franklin, Bottle and Majeed2011; Marcum et al., Reference Marcum, Handler, Wright and Hanlon2010; Rankin et al., Reference Rankin, Cadogan, Patterson, Kerse, Cardwell and Bradley2018; Verrue, Petrovic, Mehuys, Remon, & Vander Stichele, Reference Verrue, Petrovic, Mehuys, Remon and Vander Stichele2009).
According to several studies, interdisciplinary interventions involving pharmacists may reduce the use of inappropriate medication and improve related residents’ health outcomes (Christie, Reference Christie2019; Nazir et al., Reference Nazir, Unroe, Tegeler, Khan, Azar and Boustani2013; Tjia, Velten, Parsons, Valluri, & Briesacher, Reference Tjia, Velten, Parsons, Valluri and Briesacher2013). Similarly, studies showed that medication reviews performed by pharmacists, in collaboration with physicians and nurses, are a suitable method to resolve medication-related problems (Halvorsen, Ruths, Granas, & Viktil, Reference Halvorsen, Ruths, Granas and Viktil2010; Wilchesky et al., Reference Wilchesky, Mueller, Morin, Marcotte, Voyer and Aubin2018), and that greater pharmacist involvement in LTC increases physicians’ and nurses’ knowledge and awareness about medications (Verrue et al., Reference Verrue, Petrovic, Mehuys, Remon and Vander Stichele2009).
Considering the findings of these previous studies, we developed a new pharmaceutical care model in LTC: the Project to Evaluate the Pharmaceutical care’ personalization in LTC homes (PEPS). This model builds on pharmacists’ expanded scope of practice and autonomy as granted by Bill 41 (Ministère de la Santé et des Services Sociaux, 2011), which took effect in June 2015 in the province of Quebec, Canada, but had not yet been implemented in LTC homes in 2017. Authority to independently prescribe medication for minor ailments, extend a prescription or adapt and manage pharmacotherapy by changing the prescribed dosage or regimen, or de-prescribing, was granted to pharmacists and implemented in the study. The model also emphasized collaboration among pharmacists, nurses, and physicians, and the integration of residents/families in care decisions to foster the LTC residents’ pharmacotherapy optimization.
In particular, nurses were encouraged to perform a physical and cognitive assessment at the admission of residents, and to also perform follow-up assessments during their stay to detect problems requiring treatment or related to pharmacotherapy. These nurses communicated signs and symptoms of a disease or changes in the residents’ health status or behavior to the pharmacist or the physician, according to the severity of symptoms and the urgency level. The nurse, the pharmacist, and the physician then discussed further assessments or pharmacological and non-pharmacological treatment options. Physicians’ focus was to complete the medical evaluation of residents upon admission, establish diagnoses and treatment goals, and handle complex situations. Pharmacists were prompted to perform regular medication reviews (i.e., upon admission and every 6 months) using published criteria such as OptimaMed criteria (Kroger et al., Reference Kroger, Wilchesky, Marcotte, Voyer, Morin and Champoux2015), and their own clinical judgment, to optimize the residents’ pharmacotherapy. Before changes to the medication were made for the first time, pharmacists discussed with the resident/family to make sure that treatment targets were in agreement with their expectations and level of care. Pharmacists also explained to the resident/family their new role. Moreover, pharmacists worked together with nurses and physicians to support families dealing with difficult medication-related situations. Pharmacists and nurses documented their interventions and the effectiveness of the pharmacological and non-pharmacological treatments attempted, in the residents’ medical file, allowing the physician to be kept informed. The PEPS model and its impact on pharmacotherapy are described in detail in another publication (Garland et al., Reference Garland, Guenette, Kroger, Carmichael, Rouleau and Sirois2021).
The present study aimed to evaluate the experience and satisfaction of health care providers exposed to the PEPS model, and to identify facilitators of and barriers to its implementation, the perceived results, and recommendations for implementing the model in practice.
Method
The PEPS model was implemented for 1 year (March 2017 to May 2018) among residents 65 years of age and older in two LTC homes (A and B) in Quebec City. Older residents were targeted based on their higher risks of polypharmacy and taking potentially inappropriate medications and greater expected benefits. This qualitative study was performed at the end of the implementation period.
Recruitment
In each LTC home, two members of the research team invited the PEPS implementation committee members at the end of their last meeting to participate in an individual interview, and collected names of those interested. Further, health care providers were approached through managers. Special attention was given to recruiting health care providers from various disciplines and units to ensure, whenever possible, the diversity of experiences. A research professional contacted all potential interviewees by phone to give them more information on the study and the interview and schedule an appointment with those interested in participating. She obtained written consent from each interviewee at the time of the interview. The study was approved by the local ethics review board of the Centre intégré universitaire de santé et de services sociaux de la Capitale-Nationale (CIUSSSCN) (#2017-2018-09R).
Data Collection
The research professional conducted the interviews using a semi-structured guide developed in collaboration with a qualitative research consultant. The questions covered specific categories based on the participatory evaluation model suggested by Patton (Reference Patton2008): (1) resources required for support, training, and coaching; (2) activities required by the model; (3) participation in the model’s implementation; (4) reactions to and satisfaction with the model; (5) changes in knowledge, attitudes, and skills; (6) change in practice; and (7) perceived results of the model. Interviewees were also asked about strategies and recommendations for facilitating the implementation of the model. The interview guide was pre-tested with a pharmacist, an assistant head nurse, and a family physician practicing in LTC homes and familiar with the PEPS model. Their comments and reactions allowed the guide to be refined. These test-interviews were not included in the analysis.
Interviews were in person and occurred during working hours. At the end of the interview, the interviewees were invited to fill in a short questionnaire to gather some socio-demographic and professional characteristics. A summary sheet was completed at the end of each interview by the interviewer, and a preliminary analysis of emergent themes was performed. The number of interviews was increased until this preliminary analysis revealed a theoretical saturation of data. All interviews were audio-recorded and transcribed verbatim. A professional translator converted interview transcripts from French to English.
Analysis
A thematic content analysis (Miles, Reference Miles1984; Paillé & Mucchielli, Reference Paillé and Mucchielli2003) of the interviews was performed with the assistance of the NVivo12 software (QSR International). More precisely, we performed a directed content analysis (Hsieh & Shannon, Reference Hsieh and Shannon2005). The research professional who performed the interviews first proceeded to data segmentation and categorization and elaborated a preliminary code book, including themes extracted from Patton’s model (Patton, Reference Patton2008) and emergent themes (Hsieh & Shannon, Reference Hsieh and Shannon2005). Further on, a validation exercise was performed with another research professional. In this phase, the two research professionals independently proceeded to the data categorization from excerpts of four to five interviews using the code book, and then compared their codification. In instances of disagreements, they reviewed and discussed the concepts until a consensus was reached. A third research professional was consulted when an agreement could not be reached. This process was performed four additional times until a coding concordance judged sufficient by the research team in collaboration with a qualitative research consultant was attained. Approximately one third of each interview’s codes have been validated by the two research professionals following this process. The researchers, including health care providers practicing in LTC, were consulted throughout this process and involved in discussions regarding data categorization for refining the analysis.
Results
LTC Homes and Characteristics of Interviewees
The characteristics of each LTC home at the beginning of the implementation are presented in Table 1.
Table 1. Description of the LTC homes where the PEPS intervention was implemented
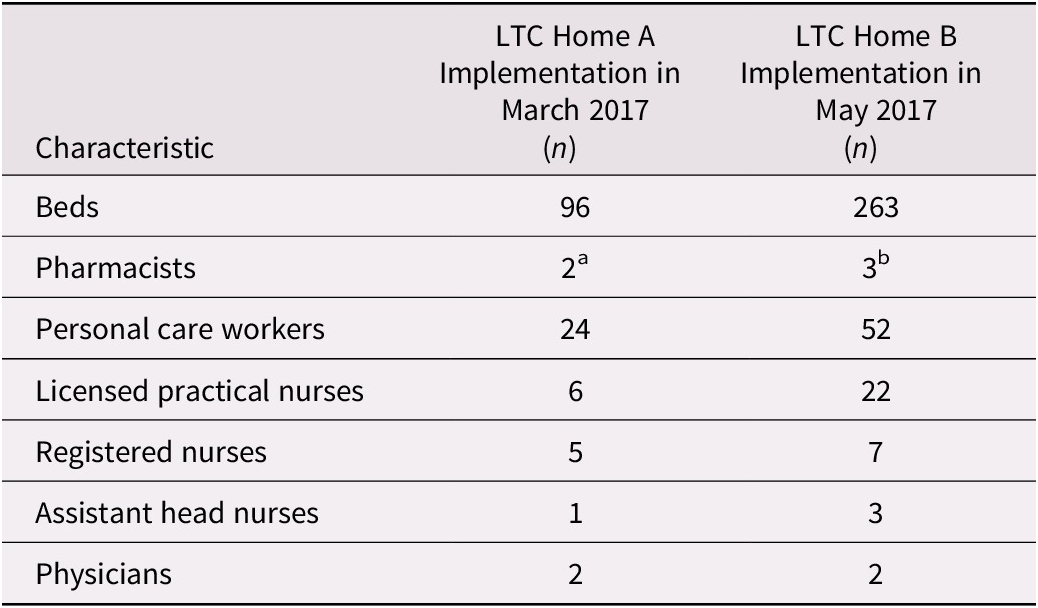
Note. aTwenty-four hours per week in total. bOne full-time equivalent (40 hours per week in total)
Twenty-two health care providers and one manager participated in an interview for an average length of 26 ± 13 minutes. The majority were female (87%) and had 15 ± 10 years of experience on average in their current discipline (see Table 2).
Table 2. Characteristics of participants who took part in an individual interview
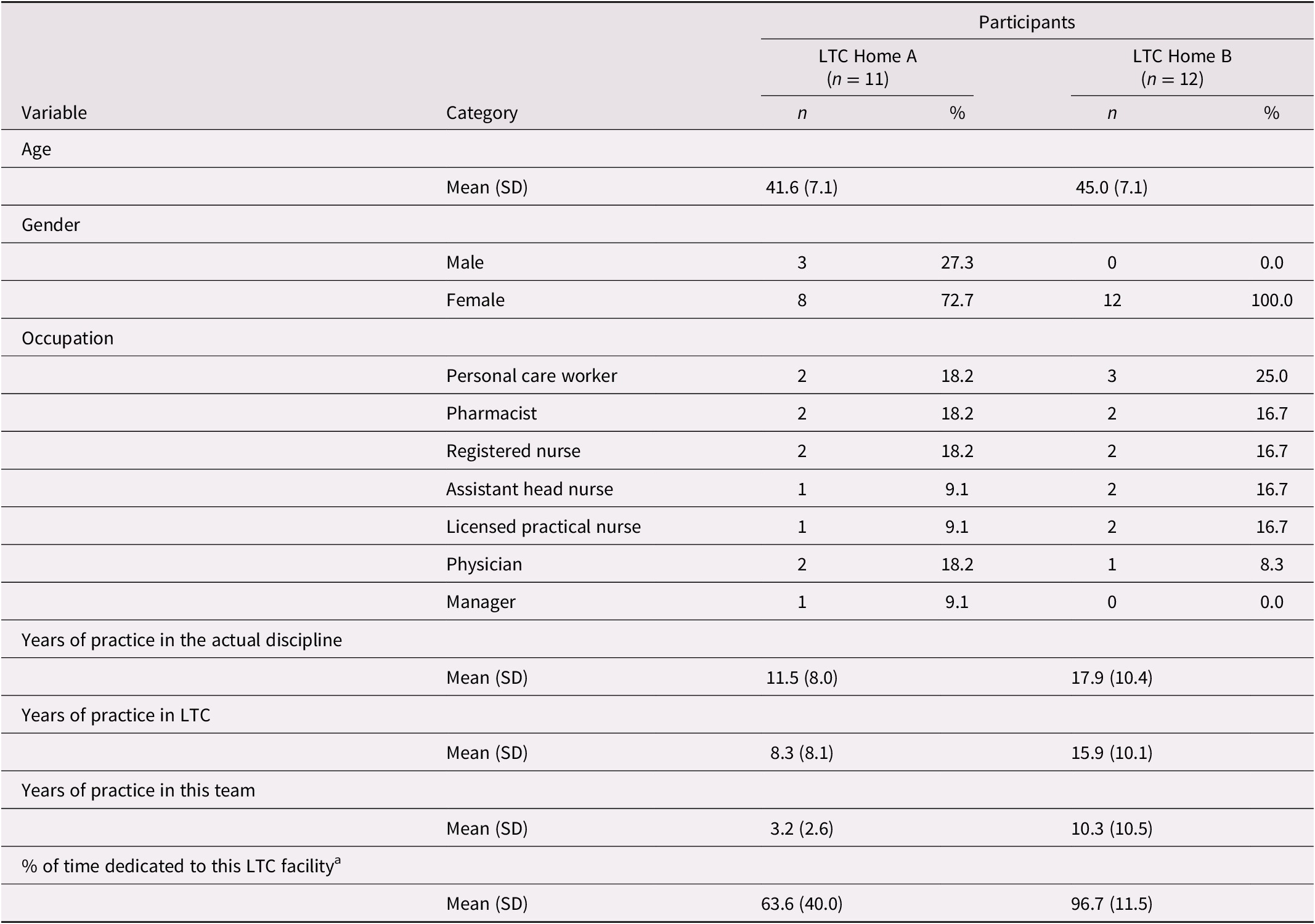
Note. aLTC health care workers may work in different facilities on the same health board.
SD = standard deviation
The following section presents the main results organized according to the categories based on Patton’s model (Patton, Reference Patton2008).
Resources Required for Support, Training, and Coaching
At the beginning of the implementation, the project manager offered training to registered nurses, pharmacists, physicians, licensed practical nurses, and personal care workers. This training seemed sufficient for some registered nurses and a pharmacist to properly implement the new practices. For one registered nurse and one personal care worker, it lacked precision regarding the objectives targeted by the model and the new responsibilities of each member of the health care teams. A regional health board’s mentoring team offered training on clinical assessments to registered nurses within a continuous education effort. This training prompted a structured approach to performing a physical assessment and the documentation of clear notes in the residents’ file, which were perceived beneficial for the pharmacists and physicians in guiding their interventions. Moreover, the pharmacists, the registered nurses, the assistant head nurses, and the physicians could consult the project manager, who acted as a pharmacy mentor, for support or validation. It would have been helpful, however, if the physicians also had access to a mentor in their discipline as believed by this pharmacist (PH):
“[…] I find that on the medical side, the doctors, I think they felt rushed, and they had no one to refer to.”
(PH-04)A local implementation committee was set up in each LTC home. Meetings were held regularly and welcomed representatives of each discipline called out in the PEPS model; that is, nursing, medicine, and pharmacy. During these meetings, the committee members reported their successes and difficulties in applying the model and their questions. The assistant head nurse acted as an intermediary between the committee and the nursing care teams, as indicated by this assistant head nurse (AHN).
[…] once a month, we still had what we called “the PEPS committee”, where we received updates […] or if we had questions or anything coming from the teams, we took these questions to the committee and brought back the answers and how to proceed to the teams.
(AHN-02)Some interviewees reported a need for additional organizational support. One pharmacist would have wished for more freed-up time for training and for integrating the new practices. In LTC Home B, 4th-year pharmacy students in training were involved in the residents’ medication review. This support for pharmacists made it possible to cope with the model’s additional workload without other pharmacy resources allocated.
Participation in the Model’s Implementation
The interviewees identified different factors that facilitated or hindered, from their perspective, the implementation of the model into practice. According to health care providers from all disciplines, in both sites, it required solid collaborative relationships. The availability, proximity, and responsiveness of pharmacists, particularly in LTC Home B, were also perceived as facilitating factors, as this licensed practical nurse (LPN) expressed:
For me, it was very positive because when we were forced to wait for the physician, he or she wasn’t always there or was very busy, which is understandable, but the pharmacist was more available, so it’s easier […] for the resident and us.
(LPN-05)In LTC Home A, health care providers also found that it helped if physicians were on site and accessible for more complex cases. However, in LTC Home B, where there was a lack of physicians for a certain time during the implementation period, this situation seemed to reinforce the registered nurses’ and pharmacists’ new roles. The four pharmacists, one physician, and one manager involved in nursing training reported, however, that the roles of the registered nurse, the pharmacist, and the physician were not sufficiently clear. Gray areas between their roles proved to be challenging, as this pharmacist noted:
[…] if we go back a year, physicians were doing their own thing, so as for me, I knew my role, but now the physician can also take it on, so the tough part has been to pin down each person’s set of tasks.
(PH-04)Physicians, registered nurses, and one pharmacist perceived that communication among them was suboptimal concerning follow-up with residents’ cases, especially at the beginning. Sometimes, changes were made to residents’ medication without the attending physician being aware of those changes. Physicians find it essential to always “keep track” of their patients to offer better support, as this physician (MD) shared:
[…] when there are changes to the medication, as the attending physician, you know, it’s something that I nevertheless wanted to know because…[…] in fact, when you meet families in the hallway, and they tell you “oh he’s no longer taking this medication,” or “the dosage of that medication was increased,” and you’re not aware, and there are side or adverse effects, or in any case, there are things worrying the family, you aren’t aware of it… […] there were some discussions regarding communication when changes are made […]
(MD-03)Physicians reported that when registered nurses contacted them, their evaluations were sometimes suboptimal. One of them felt that registered nurses called on him without having enacted all the interventions that they were authorized to, and that registered nurses should work on their leadership to take better charge of clinical situations that they should be able to manage, as this physician shared:
[…] I experienced situations where there was a lack of leadership, [for instance in cases] in which the nurses among themselves or with the head-nurse or the nurse assigned to help in complex cases [could not address the issue]…things weren’t working. It’s like there wasn’t really a leader; nobody was taking charge of the situation. In the end, nothing happened. You know, the problem was not solved. […] Someone had to come and take charge of the situation, and […] in the end, it’s always the physician who does so.
(MD-01)Some interviewees thought that the assistant head nurse plays a key role and could take on more leadership and raise red flags when she identified situations requiring medical expertise.
Furthermore, one pharmacist and one physician found that some registered nurses, licensed practical nurses, and personal care workers had the reflex of consulting the physician when present, even concerning interventions that a pharmacist or a registered nurse could have performed. According to some interviewees from both LTC homes, high employee turnover, absences, and replacements challenged the PEPS model’s implementation. Newly arriving health care providers had poor knowledge about residents and the new practice model, which sometimes led to a loss of information or non-optimal monitoring.
According to pharmacists, one registered nurse, and one assistant head nurse, the rapid occurrence of changes caused them to have an increase in their workload. Notably, the number of residents to be cared for by each pharmacist was perceived as being too high at the beginning. Similarly, the occurrence of changes to residents’ medication in short periods was a challenge to provide care, given the behavior changes it induced in some residents, as shared by this assistant head nurse:
[…] at the beginning of the project, there were many changes, for example to the medication, all of which happened at the same time. It’s as if it started too quickly. […] But we saw, for some [residents] it went well, for others not so well, but it was a lot at the same time. So, at a certain point, we said, “hold on one sec, slow down.” Because, although it was going well, you know, sometimes, we asked ourselves, “how can it be that caregiving has become more difficult?” You know, they [residents] collaborate less, are in a worse mood, or are more aggressive. And then, we noted that, oops, there’d been changes to the medication […]
(AHN-03)Changes In Knowledge, Attitudes, and Skills, and Change in Practice
For several pharmacists, registered nurses, and physicians, applying the PEPS model required a period of adaptation and a learning process. In particular, registered nurses learned over time in which contexts they should call on a physician or a pharmacist regarding medication problems. For some registered nurses, licensed practical nurses, and personal care workers, applying the PEPS model did not seem to have entailed any significant changes to their usual practice, whereas doing this did change the old habits of other health care providers. In particular, registered nurses found their “empowered” role and their increased responsibilities to be challenging. In the beginning, they found it difficult to interact directly with pharmacists; for example, adjusting a medication dose without discussing such matters with a physician. Physicians had to adapt to this new role for pharmacists as shared by this physician:
Then regarding the pharmacist, at first I found it weird, I found it difficult because, you know, they [the pharmacists] were suddenly playing a little … well … what was historically my role, huh, you know, in adjusting the medication and all that.
(MD-03)However, physicians gradually appreciated the new role of pharmacists and working in collaboration with them. On the pharmacists’ side, changes in their practice were welcomed and met their expectations concerning their increased autonomy following Bill 41. They reorganized their work effectively based on their new responsibilities. Interviewees also reported that some licensed practical nurses and personal care workers were resistant to the new model’s changes. In particular, they had worries or disagreements about adjustments made to older residents’ medication, such as reducing antipsychotics, because they sometimes observed behavioral changes following these modifications. Their attitudes evolved favorably after receiving ongoing education about the new practices and observing PEPS’s positive impact.
Reactions to and Satisfaction with the Model
At the end of the implementation, most health care providers reported being satisfied with their new practices and did not want to return to the way things were before. Many interviewees, including at least one in each discipline, thought that the PEPS model should be implemented in all LTC homes.
Assistant head nurses, physicians, pharmacists, personal care workers and one manager all perceived that families were satisfied, reassured, or grateful for the care and services based on the PEPS model and seemed to be open to the pharmacists’ increased involvement. Families were able to get a quicker response to their medication-related questions through pharmacists and felt more involved in the residents’ care and decisions, as this physician reported:
[…] they [the families] liked it because they were consulted […] by different professionals, including pharmacists, among others. You know, when they [the pharmacists] made changes, they had to call the families. […] they [the families] were thus better informed regarding the medication used, changes, and so on […]. In any case, it was really well perceived, in general, by families.
(MD-03)However, some interviewees shared that a few families had worries and disagreed with changes, particularly those made by a pharmacist instead of a physician, or did not fully understand why changes were made.
Perceived Impacts of the Model Implementation
In both LTC homes, most interviewees observed that the PEPS model implementation made it possible to intervene more quickly and save time, particularly in the absence of a physician or when admitting new residents. The model made it possible to take greater advantage of the expertise of each professional. In both homes, it led to better use of the physicians’ limited time and improved their accessibility. It enabled physicians to see more residents, go into more depth in their interventions, and offer better support to the residents and their families. Several health care providers in both LTC homes also noted improvement in the evaluation, management, and monitoring of residents by on-site health care teams. In LTC Home B, the PEPS model was perceived as useful, even indispensable, in the context of a shortage of medical resources. In both LTC homes, assistant head nurses, pharmacists, one physician, one registered nurse, and one licensed practical nurse perceived an improvement in the performance, effectiveness, and efficiency of their team, as this registered nurse (RN) highlighted:
[…] I find it so effective that I’m beginning to question the need for a physician’s near constant presence as we had before. You know, I agree that you need a physician in the facility for new things, acute situations, but much less than before because the role of pharmacists is really important, and it greatly simplifies teamwork.
(RN-04)In LTC Home A, assistant head nurses, registered nurses, physicians, and pharmacists found that applying the model brought better collaboration and communication within their team and strengthened their bonds. In both LTC homes, physicians and pharmacists reported that they now increasingly want to work as a team.
Moreover, according to health care providers from all disciplines, the PEPS model’s application facilitated registered nurses’ and pharmacists’ autonomy in resolving situations without a physician. It encouraged the use of available tools such as collective prescriptions (i.e., those made “by a physician or a group of physicians to a professional or an authorized person, specifying the medications, treatments, examinations…to be provided to a group of patients or for clinical situations specified in this prescription…”) (Collège des médecins du Québec, 2012). Assistant head nurses, physicians, and pharmacists felt more involved in the caregiving process and reported greater job satisfaction. Pharmacists, in particular, found their practice more exciting and stimulating and felt a greater appreciation of their role by the health care teams, as this pharmacist expressed:
[…] more appreciation of the role, you know between spending your time suggesting things in a file that nobody will read or that nobody bothers to complete, or does so late, and managing problems right away then seeing the impact…, […] professionally, it’s stimulating, and it pushes us to be up to date and to be pro-active and to take much better care of our patients.
(PH-02)For their part, the physicians found that applying the model reduced their workload, as this physician reported:
It was amazing for me […]. It made things a little easier in that respect…well enormously, in fact. You know, on the nursing side, in terms of the number of calls, at the beginning and all of that, it was really extraordinary the fact that there’s more and more use being made of collective prescriptions.
(MD-03)In LTC Home B, two assistant head nurses, two registered nurses, one licensed practical nurse, and one manager noted that the model made it sometimes possible to avoid transferring residents to the hospital and avoided back-and-forth trips between the facility and the hospital, especially in a context of medical resource shortage, as this assistant head nurse shared:
It’s also much better for us and the clientele because we avoid many transfers. So families are reassured because we can keep many more residents [in the facility if there is a problem], and there’s much less coming and going, all this, you know, so they’re in the comfort of their cozy rooms and their living environment, and they have access to all the services needed promptly.
(AHN-02)In general, interviewees believed that the PEPS model led to a better quality of care for residents, more comfort and relief, and a better quality of life. A partnership between the pharmacist and the registered nurse facilitated, for example, better pain management for those residents considered challenging to evaluate or treat. Two assistant head nurses, one registered nurse, one pharmacist, and one personal care worker felt that their practices were more patient centered.
Only two interviewees reported negative impacts of the PEPS model: one personal care worker and an assistant head nurse observed some aggressive behaviour among older residents for whom changes had been made to their medication. The same personal care worker also reported having seen more falls among these residents.
Strategies for Facilitating the Implementation of the Model and Recommendations
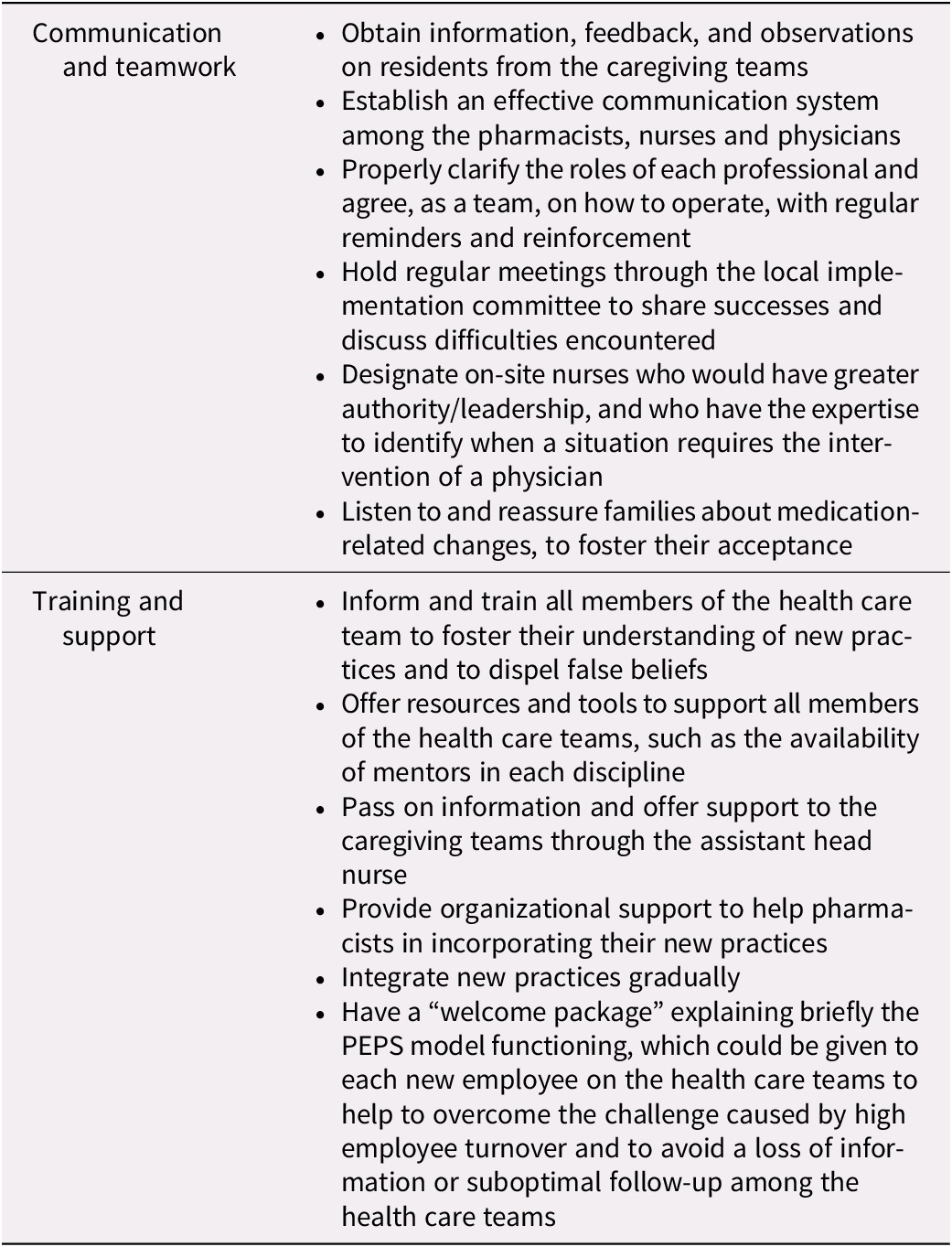
The interviewees shared strategies that they had experienced as facilitators for implementing the PEPS model in their practice and recommendations. Those strategies and recommendations are summarized in Table 3.
Table 3. Strategies for facilitating implementation of the model and recommendations
Discussion
Using Patton’s model (Patton, Reference Patton2008), this study identified several factors needing to be fostered when integrating a new practice model in LTC settings, based on the experience with implementing the PEPS model.
First of all, the rapid occurrence of changes seemed to have caused work overload for pharmacists and registered nurses. In particular, pharmacists perceived that additional resources would have been required to free up time for training and gradually integrate their new practices. Support in the reorganization of their work to optimize their time was also perceived as essential. Caspar, Cooke, Phinney, & Ratner (Reference Caspar, Cooke, Phinney and Ratner2016) recommend that any interventional research conducted in LTC settings should minimally include change management, at least in the short term, for health care providers who are asked to embark on a change initiative that would likely produce additional stress. In the current study, regular meetings with the local implementation committees were perceived as helpful by the interviewees. It provided them with a space for sharing successes and discussing difficulties encountered and strategies to overcome them. All the pharmacists found it useful to be able to consult a resource pharmacist for support or validation. The literature review by Caspar et al. (Reference Caspar, Cooke, Phinney and Ratner2016) also revealed that interventions, including mentoring and team meetings, are effective for implementing new skills and practices among health care providers in LTC settings.
Some registered nurses found it challenging to deal with their increased autonomy and responsibilities. Their feeling was congruent with observations made by physicians who sometimes found that registered nurses contacted them for clinical situations that they themselves, or a pharmacist, should be able to manage, or that the documentation that these nurses made in the residents’ files was incomplete. These findings are similar to those of a study conducted in Australia. In that study, some physicians believed the LTC nursing staff lacked skills, notably regarding the documentation and management of medication-related issues, and thought that this situation added unnecessarily to the physicians’ responsibility (Palagyi, Keay, Harper, Potter, & Lindley, Reference Palagyi, Keay, Harper, Potter and Lindley2016). The current context of LTC nurses’ work overload may also compromise the quality and efficiency of nursing assessments and documentation (Voyer et al., Reference Voyer, McCusker, Cole, Monette, Champoux and Ciampi2014). In the current study, the range of training offered to registered nurses, including clinical mentoring, was perceived as beneficial in optimizing registered nurses’ physical assessments and documentation. A systematic review also revealed that mentorship programs are an effective strategy for improving nursing competencies (Chen & Lou, Reference Chen and Lou2014).
Furthermore, in the present study, the registered nurses’ and pharmacists’ ongoing training of the licensed practical nurses and personal care workers appeared an effective approach to reassure them and lessen their resistance to changes and concerns. Interviewees also perceived that the assistant head nurse had a crucial role in supporting and training the nursing care teams. This opinion is in line with a study by Monette et al. (Reference Monette, Monette, Sourial, Vandal, Wolfson and Champoux2013), which showed that the involvement of a trained nurse well known by the staff facilitated and supported continuous learning of the nursing staff and personal care workers.
The deployment of the new pharmacists’ role was challenging at first for physicians, which is consistent with findings of another qualitative study reporting that it was challenging for physicians when pharmacists questioned their prescribed medication therapy decisions (Halvorsen et al., Reference Halvorsen, Ruths, Granas and Viktil2010). In the current study, this situation required regular team discussions and reminders to clarify the pharmacists’, physicians’, and registered nurses’ roles and ways to work together, because of grey areas identified between their roles. Other qualitative studies also found that pharmacists’ professional contribution and role in LTC homes’ multidisciplinary team were unclear to physicians and nurses (Halvorsen, Stensland, & Granas, Reference Halvorsen, Stensland and Granas2011; Kwak, Lee, Oh, Ji, & Kim, Reference Kwak, Lee, Oh, Ji and Kim2019). These ambiguities highlight the importance of “mutual understanding” among health care providers in LTC homes, as the pharmacists’ role may overlap with those of other health care providers (Kwak et al., Reference Kwak, Lee, Oh, Ji and Kim2019). In the current study, the physicians gradually got used to the new role of pharmacists. The physicians reported that they now want to work in partnership with the pharmacists and perceived the pharmacists’ contribution as beneficial for the residents’ follow-ups and the optimization of medication use. Similarly, in another qualitative study, physicians and nurses who experienced collaboration with pharmacists valued their contribution and perceived that this collaboration improved residents’ pharmaceutical care (Halvorsen et al., Reference Halvorsen, Stensland and Granas2011).
The physicians also reported poor communication with pharmacists at the beginning of PEPS implementation. Some physicians were surprised by changes made to residents’ medication without the physicians having been made aware of the changes first. In the current study, establishing an effective communication system among the pharmacists, registered nurses, and physicians was a key strategy. In particular, follow-up tools were developed in collaboration with the local implementation committees and were successfully implemented. The assistant head nurse also played a pivotal role, by passing information between the nursing care teams and the local implementation committee.
Giving a “welcome package” to each new employee explaining the PEPS model functioning was also suggested, to overcome the challenge caused by high employee turnover. This strategy could avoid a loss of information or suboptimal follow-up among the health care teams. At the end of the study, some licensed practical nurses and personal care workers who were approached for an interview were not aware of the PEPS model’s implementation in their LTC home, which may have hindered the model’s application.
Nevertheless, the PEPS model’s implementation enabled pharmacists and registered nurses to have greater autonomy, and empowered them as intended. They felt more involved in the caregiving process and experienced greater job satisfaction. Another study also found that a higher level of empowerment is associated with greater job satisfaction among nurses practicing in LTC settings (Li, Kuo, Huang, Lo, & Wang, Reference Li, Kuo, Huang, Lo and Wang2013). Pharmacists also found their practice more exciting and stimulating and felt a greater appreciation of their role by the health care teams. These changes met their expectations concerning their increased autonomy following the implementation of Bill 41. In one LTC home, the absence of access to on-site physicians during a certain time reinforced the need for increased registered nurse–pharmacist collaboration for the resolution of minor health problems. This registered nurse–pharmacist collaboration was also perceived as an asset, considering the significant shortage of physicians in Canada (Malko & Huckfeldt, Reference Malko and Huckfeldt2017) and physicians’ increasing caseload of LTC residents (Frank, Seguin, Haber, Godwin, & Stewart, Reference Frank, Seguin, Haber, Godwin and Stewart2006; Gibbard, Reference Gibbard2017). Applying the PEPS model also improved the physicians’ availability and accessibility and freed up their time for resolving more complex situations, which was perceived as a critical element for the model’s success.
Moreover, interviewees perceived that applying the PEPS model, mainly because of the pharmacists’ huge availability, decreased the need to transfer residents to an emergency department for situations judged not urgent or of low severity that could be safely managed in the LTC home without a physician. This observation is consistent with a study in which LTC health care providers had the feeling that they often transferred residents to an emergency department for problems that fell within their scope of practice, such as medication reviews (McCloskey, Reference McCloskey2011). Some interviewees in the current study thought that the assistant head nurse could take on more leadership and raise red flags when she identified situations requiring medical expertise.
Generally, in both LTC homes, numerous health care providers perceived better performance, effectiveness, and efficiency by their health care team in providing residents’ care and support. This observation is also corroborated by a systematic review (Tricco et al., Reference Tricco, Thomas, Veroniki, Hamid, Cogo and Strifler2019), suggesting that changes in the health care team’s structure, including multidisciplinary collaboration, may reduce the risk of adverse health outcomes among residents. In one LTC home, some interviewees identified better communication and collaboration among their team, which has strengthened their bonds. This team cohesion may lead to increased work satisfaction (Tourangeau, Cranley, Spence Laschinger, & Pachis, Reference Tourangeau, Cranley, Spence Laschinger and Pachis2010). Lastly, health care providers felt that most older residents and their families reacted positively to the new practices brought by the PEPS model, including de-prescribing of medications, when the providers took time to explain the changes and reassured the residents and families. Other authors (Reeve, Low, & Hilmer, Reference Reeve, Low and Hilmer2016) have highlighted that discussions between the health care providers and the older adult or family caregiver about withdrawing medications influenced the family caregivers’ openness towards de-prescribing.
Otherwise, using a qualitative design in this study enabled gathering in-depth experiences and feedback from health care providers who tested the PEPS model in their LTC home. Several strengths of this approach can be underlined. First, the views of all involved types of health care providers were considered, which enabled a comprehensive assessment of the experience with the PEPS model. Second, a professional interviewer uninvolved in care or the model’s development, using a semi-structured guide, conducted the interviews. This approach allowed health care providers to express their opinions or concerns freely. Third, the health care providers were exposed to the PEPS model during a significant period (12 months) before sharing their opinion. However, this time lag might have affected the recall of their experience at the beginning of the PEPS model’s implementation in their practice. Some limitations must also be acknowledged. The PEPS model was implemented in only two LTC homes. The interviewees’ perceptions of the PEPS model might not be generalizable to all LTC health care providers or LTC homes. Several inherent factors of LTC homes, such as the characteristics of the residents (e.g., demographics, health conditions), the health care providers (e.g., experience, personal beliefs), the LTC home (e.g., resources, number of beds), and the organizational culture may have influenced the results (Hughes, Lapane, Watson, & Davies, Reference Hughes, Lapane, Watson and Davies2007). However, the two LTC homes that took part in the study were different regarding the health care teams’ size and professional resources, and similar in many respects to those in Quebec. Finally, LTC residents and families were not interviewed, as prior experiences revealed that this involvement might cause them an additional burden. Findings on the impact of the PEPS model on them are based on health care providers’ perceptions. Future studies could gather the residents/families’ experiences and perspectives regarding the pharmacists’ role in LTC homes based on the PEPS model, and the impact of the pharmacists’ interventions.
Conclusion
Applying the PEPS model seems to be an effective way to use the pharmacists’ and registered nurses’ expertise to their full extent in LTC homes, facilitate collaboration among pharmacists, registered nurses, and physicians, and make better use of the limited time devoted to LTC residents by family physicians. This practice model may increase work satisfaction in LTC homes and positively influence the quality of care and residents’ well-being. Like any significant change in practices, this model’s implementation should be gradual and should include proper training, coaching, and mentoring for all types of health care providers and thorough involvement of all stakeholders. Nurse mentoring and sufficient pharmacist resources also seemed to be crucial elements for successful implementation. Our results may facilitate the PEPS model’s implementation or the implementation of similar models in other LTC homes, or develop similar interdisciplinary collaboration models fostering better pharmaceutical care.
Acknowledgements
We are grateful to all the health care workers of the CIUSSSCN who applied the PEPS model and kindly shared their experience. We also thank Julie Castonguay who reviewed the interview guide and the qualitative analysis process, Lilianne Bordeleau and Steve Paquet who have been involved in the validation exercise, Sylvie Roy who translated the quotes from French to English, Carolina Tisnado-Garland who participated to a test interview and who took part in discussions on the results, and Caroline Sirois who also took part in the discussions on data categorisation.






