An 80-year-old man was seen in urgent neuro-ophthalmology consultation for bilateral vision loss. He had a past medical history of hypertension and metastatic stage IV colorectal adenocarcinoma. Four months prior to presentation, he developed gradual onset, painless blurred vision in his right eye. He underwent cataract surgery in that eye, but his vision continued to decline to the point of no light perception. He developed new onset, painless, blurred vision in his left eye 3 weeks prior to presentation and woke up with no light perception in his left eye one day prior to presentation.
On examination, he had no light perception vision in both eyes, his pupils were mid-dilated and did not respond to light. Dilated fundus examination revealed right optic disc pallor and was normal in the left eye (Figure 1). Due to concern for a compressive or infiltrative lesion of the anterior visual pathways, he underwent magnetic resonance imaging of the orbits and sella with contrast and this revealed an extra-axial mass in the planum sphenoidale and tuberculum sellae with bony erosion and encasement/infiltration of the bilateral optic nerves (Figure 2). The imaging features were highly characteristic of a metastatic lesion. An urgent neurosurgery consultation was obtained and he was not thought to be a good candidate for surgery. Urgent radiation therapy was initiated (30 Gy in 10 fraction) with methylprednisolone 1 gram daily for 5 days with an oral dexamethasone taper, but he remained no light perception in both eyes at a 3-month follow-up. Repeat computed tomography of the chest and abdomen at the 3-month follow-up showed new liver and other metastases.

Figure 1: Optic nerve photos demonstrating right optic disc pallor in the right eye and a normal appearing optic nerve in the left eye. The patient was pseudophakic in the right eye, which contributes to the pallor in the right eye.
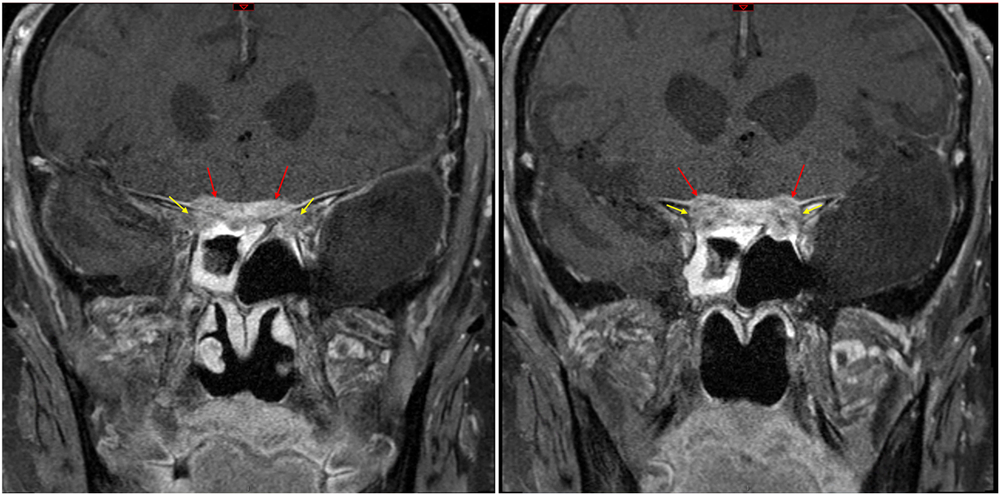
Figure 2: Coronal T1 post-contrast magnetic resonance imaging (MRI) demonstrating an extra-axial mass in the region of the planum sphenoidale and tuberculum sellae (red arrows) with bony erosion and encasement/infiltration of the bilateral optic nerves (yellow arrows).
Colorectal adenocarcinoma very rarely metastasises to the brain and optic nerves. Large-scale retrospective review of colorectal adenocarcinoma cases from multiple sites reveal a 0.1%–4% incidence of brain metastases.Reference Mege, Sans, Ouaissi, Iannelli and Sielezneff1,Reference Nozawa, Ishihara and Kawai2 Brain metastases usually have a poor prognosis with usually less than 9 month life expectancy.Reference Mege, Sans, Ouaissi, Iannelli and Sielezneff1,Reference Nozawa, Ishihara and Kawai2 The most common presenting symptom is headache, and surgical resection produces the best survival outcome.Reference Mege, Sans, Ouaissi, Iannelli and Sielezneff1,Reference Nozawa, Ishihara and Kawai2 Colon cancer metastases causing vision loss is extremely rare, with only case reports mentioning metastasis to the optic nerve,Reference Jamall, Theodoraki, Amin, Verity and Bates3 parasellar region,Reference Neroni, Artico, Pastore, Esposito and Fraioli4,Reference Issa, Thota, Spiro, Daw, Chiesa and Haddad5 and to a pituitary adenoma.Reference Noga, Prayson, Kowalski, Sweeney and Mayberg6 Although metastases to the anterior visual pathways are a rare cause of vision loss, new reduction of vision, changes in extraocular motility or visual field defectsReference Al-Aridi, El Sibai, Fu, Khan, Selman and Arafah7 and new endocrine abnormalities such as secondary hypothyroidism or diabetes insipidusReference Ariel, Sung, Coghlan, Dodd, Gibbs and Katznelson8 should increase suspicion and initiate imaging to look for compressive aetiologies.
Despite the low incidence of brain metastasis from colorectal adenocarcinoma, there is an overall large patient population at risk. It remains an important differential diagnosis in a patient with new neurological or visual changes and a history of cancer. Metastasis anywhere along the anterior visual pathways could cause vision changes manifesting as visual acuity reduction or visual field defects. Patients presenting with vision loss and a history of cancer should be evaluated for signs of optic neuropathy and timely investigations should be initiated to preserve as much vision as possible.
Disclosures
The authors have no conflicts of interest to declare.
Statement of Authorship
JCYW and JAM were both involved in the project conception, authorship and editing.




