Ascertainment of baseline rates of cerebral venous thrombosis (CVT) has taken on significant recent importance in evaluating frequency of CVT as a complication of both COVID-19 and COVID-19 vaccination, particularly in the context of vaccine-induced thrombosis with thrombocytopenia. Reference Taquet, Husain, Geddes, Luciano and Harrison1 Previous estimates of the incidence of CVT vary widely, ranging from 3 Reference Stam2 to 20 Reference Otite, Patel and Sharma3 per million person-years, with more recent studies reporting a higher incidence than previous.
Factors that may account for discrepancies in estimates include 1) increased use of routine neurovascular imaging, Reference Otite, Patel and Sharma3 2) case ascertainment method for CVT Reference Devasagayam, Wyatt, Leyden and Kleinig4 (e.g. using administrative data, prospective reporting, use of other EMR free text), and 3) inconsistent exclusion of CVT secondary to another condition (e.g. trauma). Reference Kristoffersen, Harper, Vetvik, Zarnovicky, Hansen and Faiz5
International Classification of Disease (ICD) diagnosis coding is commonly used for case ascertainment in administrative data. Because administrative data are generated during routine clinical care and not for research purposes, it provides a wealth of data for identifying trends and patterns in large sets of real-world patient data. However, there can be many potential sources of error when ICD codes are used to capture diagnosis and treatment, ranging from errors of transcription to those from coder inattention or inexperience. Reference O'Malley, Cook, Price, Wildes, Hurdle and Ashton6 Therefore, determining the validity of specific ICD diagnosis codes allows interpretation of analysis of administrative data within its limitations. For example, while previous studies have shown good evidence of validity for both ICD-9 and 10 codes in identifying patients with ischemic stroke in administrative data, Reference McCormick, Bhole, Lacaille and Avina-Zubieta7 procedural codes used for the use of thrombolytics in stroke are likely less reliable. Reference Zhou, Allo, Mlynash and Field8 Here we examined the accuracy of administrative codes for CVT.
Cases of CVT admitted to a large Canadian tertiary stroke center (catchment of approximately 1.25 million) between 2008 and 2018 were identified using two case identification strategies: 1) free text search through all hospital electronic radiology reports using Boolean logic regardless of modality and body part and then subsequently confirming cases on manual reading of the full radiology report; 2) searching for ICD 10th Canadian iteration (ICD-10-CA) CVT diagnostic codes in all hospitalizations between 2008 and 2018 (see Table 1). Electronic medical records were reviewed to verify diagnoses of CVT identified using either strategy and the clinical context of the CVT diagnosis (Figure 1) to calculate positive predictive value (PPV) of ICD-10 codes. Sensitivities of ICD-10 codes were calculated against all identified cases of CVT identified using either strategy and were subsequently verified by chart review as the gold standard. Statistical analysis was performed using STATA/IC 15.1 (StataCorp LLC, College Station, TX). Approval was obtained from the Clinical Research Ethics Board at the University of British Columbia.
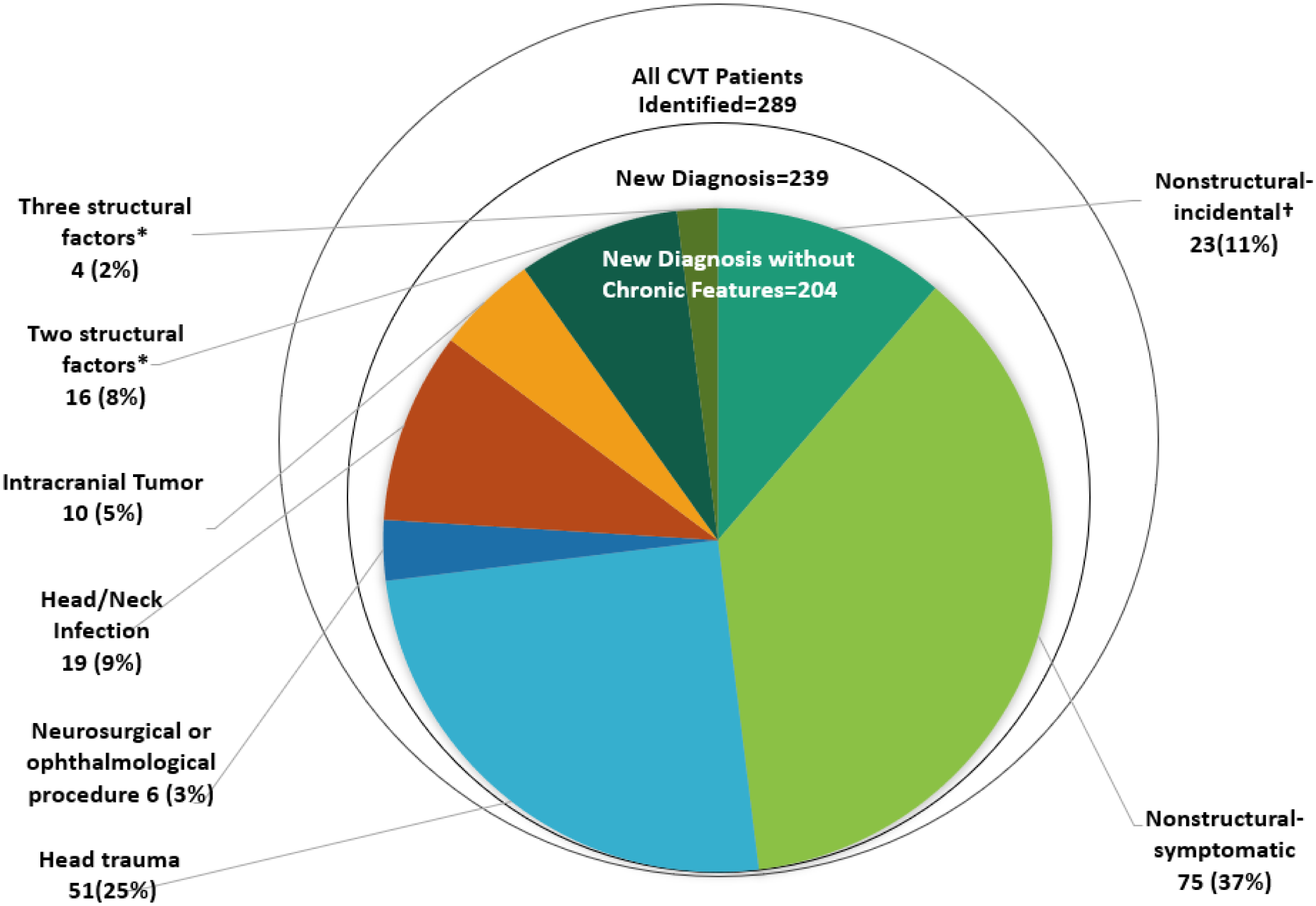
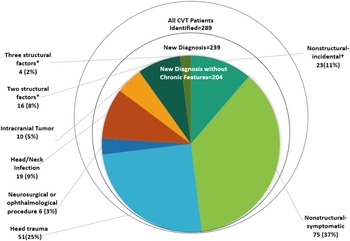
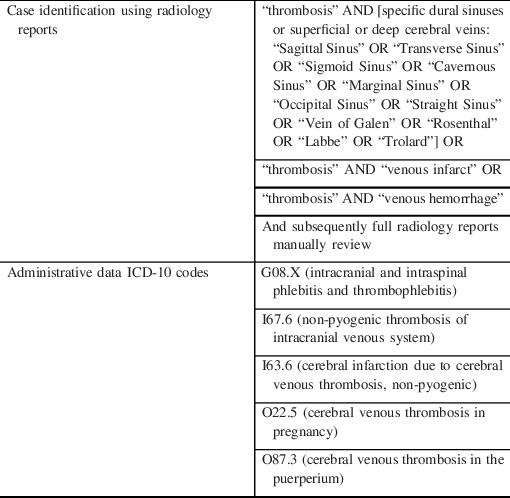
Figure 1: Cases identified using combined method of ICD-10 discharge codes and radiology database search. *Structural defined as associated with 1) head/neck Infection, 2) neurosurgical/ophthalmological procedures, 3) intracranial tumor, or 4) head trauma. †Cases deemed incidental if found on neuroimaging for an indication not attributable to the CVT (e.g. ischemic stroke).
Table 1: CVT case identification method
Through our search of radiology reports, 2530 radiology reports from 1775 patients were flagged. All reports were read in full and 282 patients with a current or prior history of CVT by radiology report were identified. We excluded cases with isolated thrombosis of the internal jugular vein, superior or inferior ophthalmic veins, or venous thrombosis associated with concurrent dural arteriovenous fistulas. Administrative data ICD-10-CA codes identified 120 patients.
After a full electronic chart review, 4/282 patients identified using radiology reports were false positives and confirmed not to have CVT on subsequent confirmatory imaging and chart review. Of patients identified using ICD codes, 7/120 were determined to have a diagnosis miscoded as CVT after chart review (Supplementary Table 1).
Using radiology reports and ICD codes for case ascertainment, 289 CVT cases were confirmed after chart review: 176 were identified only through radiology search, 11 were identified only through administrative data, and 102 were identified on both. Of these 289 cases, there were 239 new diagnoses, 204 of which were acute events without chronic features on imaging. Only 75 cases (37%) were new, symptomatic CVTs not provoked by trauma or structural processes (Figure 1). Sensitivity and PPV for ICD-10 codes depending on clinical context are reported in Table 2 and for individual ICD-10 codes in Supplementary Table 2.
Table 2: PPV and sensitivity of ICD-10 CVT codes
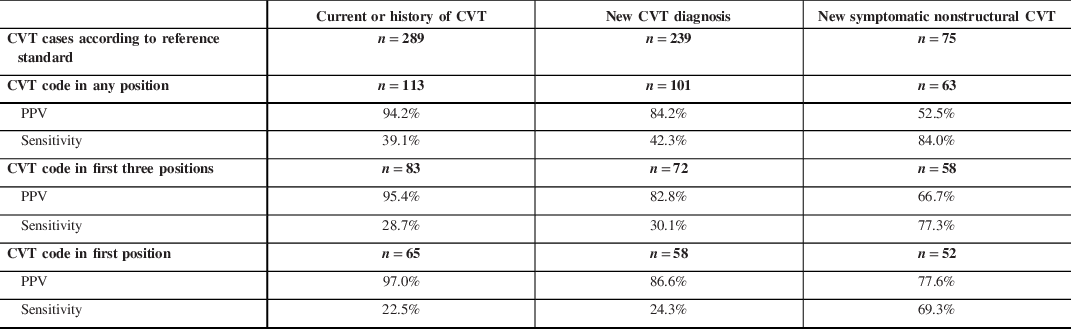
Within our study, the combination of all CVT codes has a high PPV of 94.2% for identifying patients with either a current or history of CVT. This is similar to another previous study of ICD-10 codes (PPV of 92.3%) Reference Handley and Emsley9 and higher than one older study reporting a PPV of 75.7% for ICD-9 codes (325.0, 437.6, and 671.5) in any position for CVT. Reference Liberman, Kamel, Mullen and Messé10 The sensitivity of a ICD-10 CVT code in any position within our study is lower than previously reported for ICD-9 CVT codes (39.1 vs. 77.8% Reference Liberman, Kamel, Mullen and Messé10 ) which may be a result of our more inclusive search strategy for identifying cases in radiology reports. Notably, within our study, 4/282 patients identified using radiology reports were found to not have a true diagnosis of CVT upon further chart review suggesting additional confirmation of diagnosis beyond radiology reports is useful to exclude imaging artifact and CVT mimics.
The majority of CVT identified were incidentally diagnosed in the context of intracranial processes such as trauma, surgery, infection, or masses. Only 37% were symptomatic, nonstructural incident diagnoses. As the management and prognosis of incidental versus symptomatic CVT may differ, this information has implications in the interpretation of CVT rates identified through administrative data. This is especially relevant when these codes are used to establish baseline incidence and to examine risks associated with population-based interventions such as COVID-19 vaccination.
Our study has limitations. First, data for this validation analysis come from a single urban tertiary hospital which does not have an obstetrical service; thus, the accuracy of these codes could not be assessed. Additionally, there may also be reduced generalizability to non-teaching rural hospitals with fewer cases of trauma and complicated head and neck infections. Second, our data are based on ICD-10-CA. Within Canadian administrative coding standard, the first diagnosis code reflects the most responsible diagnosis contributing to longest length of stay, as opposed to the diagnosis at admission to hospital, which is the coding practice in the United States. This may alter the generalizability of our findings when only the code within the first position is used. Finally, more detailed clinical information was not available for analysis, which limits our fuller understanding of the clinical context for individual cases.
In conclusion, administrative data have high PPV but low sensitivity for CVT (39.1%). Sensitivity was higher (84.0%), when cases of interest were limited to those with new symptomatic CVT without an obvious provoking structural cause. Our findings suggest that relying solely on CVT ICD codes for identifying CVT cases within administrative data may result in underestimation of overall CVT burden, and that reported rates of CVT may include incidentally diagnosed cases and cases secondary to structural processes.
Funding
The work is supported by a Project Grant for the Canadian Institutes of Health Research. TSF is supported by a Sauder Family/Heart and Stroke Professorship of Stroke Research from the University of British Columbia, the Heart and Stroke Foundation of Canada, the Vancouver Coastal Health Research Institute, and the Michael Smith Foundation for Health Research. AYXY is supported by the Heart and Stroke Foundation of Canada New Investigator Award. MDH receives grant funding from NoNO Inc., Medtronics LLC, Boehringer Ingelheim and Biogen Inc. through the University of Calgary.
Disclosures
TSF receives in-kind study medication from Bayer Canada and has received honoraria from Servier for speaker’s bureau work. The remaining authors have no conflicts of interest to declare.
Statement of Authorship
TSF, MH, and LZ were responsible for constructing the research and analysis plan. WH and LZ carried out data extraction. LZ and TSF carried out data analyses and preparation of figures. LZ and AY carried out preparation of tables and supplemental tables. The first draft was prepared by LZ and TSF and revised for intellectual content by all authors.
Supplementary Material
To view supplementary material for this article, please visit https://doi.org/10.1017/cjn.2021.235.