We report a 63-year-old man who presented with a 6-month history of lower back pain followed by progressive bilateral leg weakness/paresthesia and bowel and bladder incontinence. Examination revealed proximal bilateral lower extremity weakness (3/5) and bilateral lower extremity sensory deficits. Upper extremity strength and sensation were normal. Reflexes were normal in all extremities; Babinki was absent. Patient was unable to walk due to lower extremity weakness.
Neuroimaging showed an enhancing C6 intramedullary lesion and diffuse T2 signal abnormality in the thoracic cord (extending from T5-T6 through the conus medullaris) as well as vascular flow voids along the dorsal surface of the lower cord to the conus medullaris (Figure 1A-1D). Cerebrospinal fluid examination was unremarkable. He received a 5-day course of IV steroids, with minimal symptomatic improvement. Further investigation with spinal angiography revealed a L1 dural arteriovenous fistula (dAVF) (Figure 1E). The dAVF was subsequently embolized with significant clinical improvement (Figure 1F). The cervical lesion was observed with periodic surveillance. Three-month follow-up spinal/cerebral angiography showed no residual vascular lesion or evidence of any vascular malformation in the cervical topography. Six-month follow-up imaging showed that the intramedullary cervical lesion had remained stable.
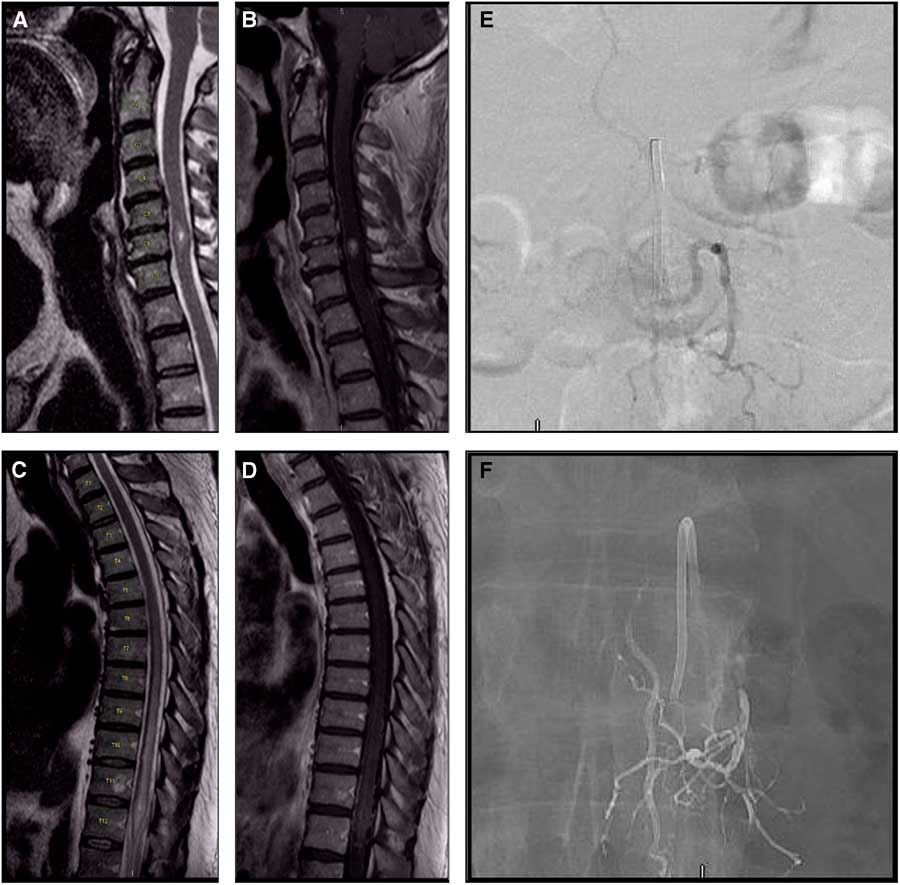
Figure 1 Spinal MRI: sagittal T2 (A) and postcontrast sagittal T1 (B) show an enhancing C6 9 mm intramedullary lesion with mild expansion of the cord and focal edema; (C) sagittal T2 and postcontrast sagittal T1 (D) show diffuse signal abnormality from T5-T6 to the conus medullaris and vascular flow voids along the dorsal surface of the lower cord to the conus medullaris. Spinal angiography (E,F). Pre-embolization spinal angiography (E): anteroposterior injection of the left L1 segmental artery shows a type 1 dural arteriovenous fistula; note arterialized vein at midline. Post-embolization spinal angiography (F) shows Onyx in the left L1 segmental artery (previous point of fistularization) and complete obliteration of the arterialized vein without residual shunting.
Spinal dAVFs are the most common spinal vascular malformations, accounting for ~70% of such lesions.Reference Krings and Geibprasert 1 Most spinal dAVFs are located in the thoracolumbar region. Thoracolumbar dAVFs usually present in older men as venous congestive myelopathy—featuring paraparesis, sensory deficits, back pain and/or genitosphincteric dysfunction.Reference Krings and Geibprasert 1 , Reference Koenig, Thron, Schrader and Dichgans 2 Conversely, cervical spinal dAVFs are more rare and have a wider range of presentations, including myelopathy, subarachnoid hemorrhage and cranial nerve dysfunction.Reference Kim, Willinsky and Geibprasert 3 , Reference Aviv, Shad and Tomlinson 4 Magnetic resonance findings suggestive of dAVFs include (a) centromedullary T2 hyperintensity over multiple segments, (b) T2 flow voids, often more pronounced on the dorsal surface of the cord and (c) diffuse T1 contrast enhancement within the cord.Reference Krings and Geibprasert 1 These findings essentially represent cord edema and dilated, coiled perimedullary vessels. Diagnosis is confirmed with spinal angiography. Treatment options consist of endovascular embolization or microsurgical intervention via targeted laminectomy.Reference Morris 5
Although extremely rare, patients with multiple independent spinal dAVFs have been reported.Reference Hanakita, Takai, Kin, Shojima and Saito 6 Moreover, cases of combined dAVF and spinal lipoma as well as dAVF and spinal dysraphism are similarly rare.Reference Mavani and Nadkami 7 , Reference Krisht, Karsy, Ray and Dailey 8 Occurrence of spinal dAVF and concurrent intramedullary spinal neoplastic lesion has not yet been described, to our knowledge. Regarding our patient, although we cannot provide a definite diagnosis for his cervical lesion (given that it was neither resected nor biopsied), we believe it is highly suspicious for low-grade glioma—based on both clinical and imaging features. Therefore, this patient may be the first reported case of spinal dAVF and concomitant intramedullary spinal neoplasm.
Dural arteriovenous fistula is a rare but treatable cause of progressive paraparesis. This condition should be included in the differential diagnoses of patients (especially older men) presenting with progressive symptoms of myelopathy whose imaging studies show an enlarged cord with intramedullary enhancement and T2 hyperintensity along with flow voids along the dorsal aspect of the cord. This report highlights the importance of pursuing a diagnosis of dAVF even in the setting of a concomitant, non-vascular spinal lesion.
Disclosures
Fábio Nascimento, Jacob Mandel and Lydia Sharp have nothing to disclose. Peter Kan reports consulting for Medtronic and Stryke Neurovascular.
Statement of Authorship
FAN: study concept and design, data analysis and interpretation, drafting manuscript. PK, LS, and JJM: study concept and design, data analysis and interpretation, study supervision, revising manuscript, final approval.



