Introduction
A recent comprehensive review of the evidence on sex- and gender-specific differences across the entire spectrum of cardiovascular disease has highlighted the paucity of published Canada-specific evidence. Reference Norris, Yip and Nerenberg1 Although some progress has been made in raising awareness of women’s cardiovascular health, it continues to be a major cause of death and disability for women in Canada and worldwide. 2 A pooled analysis of over 2000 patients from randomized controlled trials that received intravenous alteplase for acute ischemic stroke suggested that women benefitted more than men. Reference Kent, Price, Ringleb, Hill and Selker3 By contrast, the MR CLEAN group found a significant treatment interaction between sex and endovascular treatment (EVT) for large vessel occlusion acute ischemic stroke, resulting in an absence of overall effect. Reference de Ridder, Fransen and Beumer4 However, the pooled analysis of seven EVT trials through the HERMES collaboration showed that even though women were significantly older (median, 70 vs. 66 years; p < 0.001), smoked less often, and had higher collateral grades, the effect of EVT on the ordinal modified Rankin Scale was similar compared to men. Reference Chalos, de Ridder and Lingsma5 A combined analysis of the Solitaire FR With the Intention for Thrombectomy (SWIFT), Solitaire FR Thrombectomy for Acute Revascularization (STAR), and Solitaire FR With the Intention for Thrombectomy as Primary Endovascular Treatment (SWIFT PRIME) cohorts showed that women with large vessel occlusion were older than men (69 vs. 64, p < 0.001) with higher rates of atrial fibrillation, but achieved similar outcomes and greater years of optimal life after adjustment for important clinical variables. Reference Sheth, Lee and Warach6 But the results might not be generalizable due to real-world clinical practice patient selection (i.e. treating patients with advanced age, minor stroke, greater premorbid disability, or less stringent imaging selection criteria).
Clinical trial enrollment practices in Canada and the United States of America are similar and reports from the Food and Drug Administration (FDA) have shown that even though women’s participation in clinical trials has improved from < 20% in the 1990s to over 45% between 2010 and 2012, the inclusion in fields like cardiovascular disease and oncology overall remains problematic. Reference Pilote and Raparelli7 Of note, two recent major acute stroke trials achieved equal enrollment of men and women. Reference Goyal, Demchuk and Menon8,Reference Hill, Goyal and Menon9 It is especially important to utilize population-based comparative effectiveness research and other tools to gather evidence to better understand the differences in risk factors, treatments, and outcomes of acute ischemic stroke according to sex.
Our objective was to evaluate the sex differences in EVT for large vessel occlusion ischemic stroke with a population-based study in the province of Alberta, Canada, and provide a greater understanding of how the benefits and risks of EVT might vary between women and men. This knowledge will help inform the clinical decision-making process regarding EVT.
Methods
The data that support the findings of this study are not publicly available at this time.
Provincial EVT Data
All treated acute stroke patients in the province of Alberta, Canada are captured and tracked by the Quality Improvement & Clinical Research (QuICR) registry. Two comprehensive stroke centers (in Calgary and Edmonton) and 15 primary stroke centers provide service for an estimated population of 4 million across about 660,000 sq. km. The registry data are collected in routine clinical care and is considered as a part of the medical record. The current study was approved by the local ethics committee and informed consent by individual participants was waived. To cover a time period between publication of the positive endovascular trials up until the publication of the two clinical trials evaluating imaging selection and EVT in late presenting patients (DAWN, DEFUSE-3) which might have changed practice patterns, we extracted data over 3 years from April 2015 to March 2018.
We included patients 18 years or older that underwent EVT for an acute ischemic stroke due to a proximal large vessel occlusion of the anterior circulation (internal carotid artery, middle cerebral artery M1 and M2 segments, and anterior cerebral artery). Patients with posterior circulation stroke and patients not residing in the province of Alberta were excluded. Data of interest were age, sex, stroke severity according to the National Institutes of Health Stroke Scale (NIHSS) score, date and time of stroke onset or time last seen well, intravenous alteplase treatment (yes/no) as well as interval time metrics for treatment. Time from onset-to-first hyperacute treatment (either intravenous alteplase or EVT) was defined as onset-to-treatment time.
Linkage with Administrative Health Data and Outcomes
Administrative health data are not generated for research purposes, but instead are collected for payment, monitoring, planning, priority setting, and evaluation of health systems. Reference Yu, Holodinsky and Zerna10 We captured outcomes using administrative health data that are captured in the province of Alberta, Canada, through different interactions with the healthcare system (through hospitalizations, ambulatory care, emergency department visits, etc.).
The primary outcome of our study was home-time. Home-time is defined as the number of days that the patient was back at their respective premorbid living situation without an increase in the level of care within 90 days of the index stroke event. Administrative health data were utilized to determine the premorbid living situation as either any form of continuing care facility if that is where the patient had resided in the 2-week period before the index stroke admission or was otherwise inferred to be the private home. Patients who died in hospital after the index stroke admission have by definition a home-time of zero days. Home-time was initially developed from data of the GAIN International trial, and found to be a useful and robust outcome marker for stroke in 2008. Reference Quinn, Dawson, Lees, Chang, Walters and Lees11 Recent work validating home-time as a stroke outcome measure in the province of Alberta has shown that it is less vulnerable to attrition bias compared to other outcome markers prospective studies since it is obtainable in a complete population through administrative health data collection. Reference Yu, Rogers and Wang12 In an analysis of Medicare Beneficiaries in the United States of America as well as a large linked data analysis of the Scottish Stroke Care Audit with routine healthcare data, home-time after stroke was found to be a valid proxy marker for functional recovery. Reference Fonarow, Liang and Thomas13,Reference McDermid, Barber and Dennis14 Data sources used to determine home-time included the inpatient Discharge Abstract Database (acute care hospitals), the National Ambulatory Care Reporting System (emergency department), the National Rehabilitation System (rehabilitation facilities), and the Provincial Continuing Care Information System (supportive living and long-term care facilities).
The secondary outcome of interest was mortality at 90 days, which was determined from linkage with the Provincial Vital Statistics Registry.
ESCAPE Trial: Historical Control Data (Medical Treatment)
The medical treatment arm from the ESCAPE trial served as the historical control group within this study. Reference Goyal, Demchuk and Menon8 The trial has been described in more detail elsewhere, but in short, enrolled patients within 12 h of onset if imaging revealed all of the following: small infarct core is defined as Alberta Stroke Program Early CT Scale (ASPECTS) score of ≥ 6, an occlusion of the anterior circulation involving a proximal artery, and moderate-to-good collateral circulation. Reference Demchuk, Goyal and Menon15 Even though the trial involved sites from across the world, the majority of patients (64.7%) were from Canada, making it an ideal control group. The proportions of men (48%) and women (52%) enrolled in the trial were similar. The trial collected both home-time and mortality at 90 days. Time from onset-to-first hyperacute treatment (in this case intravenous alteplase) was again defined as onset-to-treatment time.
Missing Data
Within the provincial EVT group, we imputed missing NIHSS scores with the group mean and the onset-to-treatment times with the group median from the remaining available data. We imputed the onset-to-treatment time with the group median from the remaining available data and mortality at 90 days with the worst possible outcome (death) for a patient in the ESCAPE medical management group. Thirty-two patients that did not receive intravenous alteplase in the ESCAPE medical management group did not have an onset-to-treatment time recorded. Those times were imputed with the formula of randomization time plus 30 min, similar to the approach used in the HERMES collaboration analyses. Reference Saver, Goyal and van der Lugt16
Statistical Analysis
Standard descriptive statistics were used to measure the central tendency and variability of baseline characteristics. Visualization of home-time was shown using violin plots
Home-time as our primary outcome was truncated at zero and had excess zero counts. The minimum amount of days that can be spent at home during the first 90 days is 0 and the maximum 90 days (if the patient were theoretically to be discharged on the same day of the procedure). Since many patients did not return to their home/prior residence within 90 days of the index stroke, our data had excess zero counts. We explored the use of a negative binomial regression model by graphic assessment (hanging rootogram) as well as other analyses (Akaike information criterion) for model fit. We used a Cragg hurdle regression model because it provided the best fit for the data. Reference Cragg17,Reference Zerna, Rogers and Rabi18 As a first part of the Cragg hurdle regression model, a Bernoulli probability directs the binary outcome of zero (failure, hurdle is not crossed, and the patient does not return to home within 90 days after stroke) or one (success defines as any positive count, hurdle is crossed, and the patient does return home within 90 days after stroke). For the second part of the model, once the hurdle is crossed, a truncated-at-zero count model is utilized. Intravenous alteplase treatment, EVT, age, and baseline NIHSS score were selected as a priori hurdle variables based on their clinical significance for poststroke outcomes and discharge disposition. Additionally, the clinically important baseline variables age, sex, onset-to-treatment time, NIHSS scores, and intravenous alteplase status were included as covariates in the truncated-at-zero count model. We did not include imaging variables because these were not routinely available. Margins plots were used to visualize the effects of the individual variables on the conditional mean estimates of 90-day home-time
For our secondary outcome, which was binary, we used logistic regression analysis to model mortality at 90 days. The same clinically relevant baseline variables as stated above were included in that model.
P-values of less than 0.05 (two-sided) were considered to indicate statistical significance. All statistical analyses were performed using STATA (Stata 16; Stata Corp., College Station, TX, USA).
Results
Within the 3-year period (April 2015–March 2018), 611 patients were treated with EVT in the province of Alberta. We excluded 26 patients who had a permanent residence outside of the province, and thus their outcome could not be determined through administrative health data linkage as well as 9 additional patients who were treated for an isolated occlusion in the posterior circulation. The remaining 576 patients constituted the EVT group of our analysis. The medical treatment group of the ESCAPE trial had a sample size of 150 patients.
Among the total study cohort of 726 patients, 47.8% were women. Within the provincial EVT group, we had 43 (7.5%) missing NIHSS scores and 6 (1.0%) patients had missing onset-to-treatment times. Within the ESCAPE medical management group, we had 1 missing onset-to-treatment time and missing 90-day information on mortality in 3 patients.
Women were on average older than men in the total study cohort (median 74.4 vs. 67.9 years, p < 0.001) and both in the EVT group (median 75.2 vs. 67.8 years, p < 0.001) as well as the medical treatment group (72.8 vs. 68.3 years, p-value = 0.025). However, their median NIHSS scores at baseline, the percentage that received intravenous alteplase, and the onset-to-treatment times were comparable. Details and further baseline characteristics are shown in Table 1. Women who received EVT had a median 90-day home-time of 12 (0–79) days, whereas men achieved a median of 18 (0–83) days. The difference in distribution of home-time between women and men patients is illustrated in Figure 1.
Table 1: Baseline characteristics and secondary outcomes of provincial endovascular treatment (EVT) group
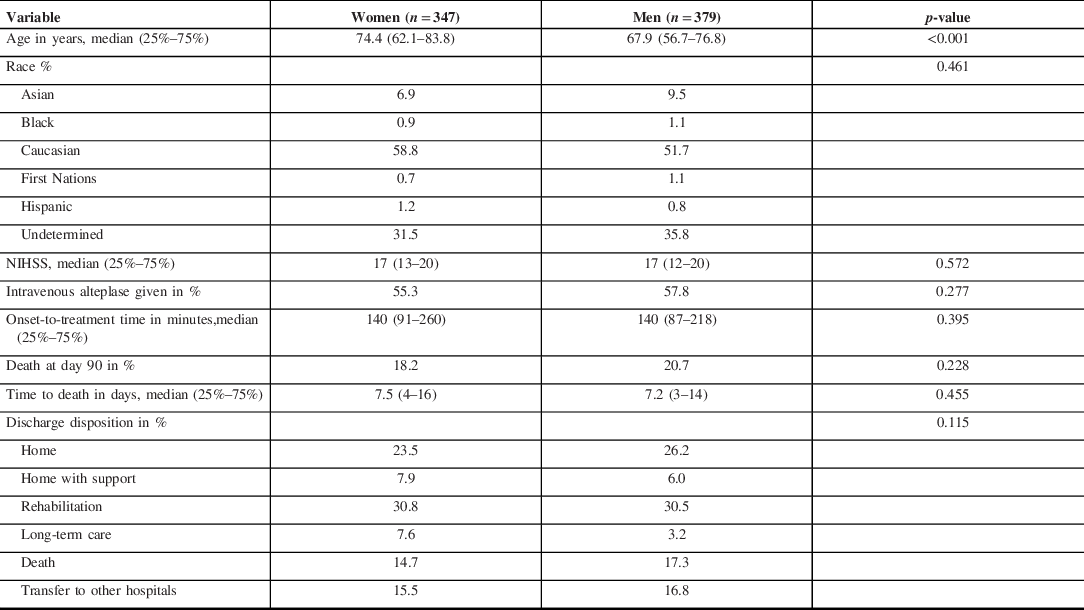
ESCAPE trial = Endovascular Treatment for Small Core and Anterior Circulation Proximal Occlusion With Emphasis on Minimizing CT to Recanalization Times trial; EVT = Endovascular Treatment; QuICR = Quality Improvement & Clinical Research; NIHSS = National Institutes of Health Stroke Scale; mRS = modified Rankin Scale.

Figure 1: Violin plots of 90-day home-time in patients receiving endovascular treatment (EVT) by sex.
Violin plots are a combination of a conventional box-whisker plot and a kernel density plot. The white dot in the middle does represent the median, the thicker blue bar the interquartile range, and the thinner blue line represents the rest of the distribution (aside from outliers which are beyond the distance of 1.5 times the interquartile range from the 25th or 75th percentile). The violin shape is the kernel density plot, which illustrates the probability of a subject to take on a given value (i.e. the wider the shape of the violin plot, the higher the probability).
There was no significant treatment effect modification by sex (p = 0.307) on the primary outcome. However, when adjusted for the a priori defined clinically important variables age, baseline NIHSS score, intravenous alteplase status, and onset-to-treatment-time, the direction of effect continued to show that women had a 90-day home-time increase of 6.08 (95% CI −2.74–14.89, p-value 0.177) days compared to 11.20 (95% CI 1.94–20.46, p-value 0.018) days in men when receiving EVT as compared to medical management. A similar association was found with intravenous alteplase, which was associated with 4.78 (95% CI −2.99–12.55, p-value 0.228) days increase in 90-day home-time in women compared to an average of 9.75 (95% CI 2.26–17.25, p-value 0.011) days in men when they received intravenous alteplase compared to not. The non-modifiable predictor’s age and higher NIHSS score were associated with decreased 90-day home-time in both sexes (all p-value <0.001) (Figure 2).
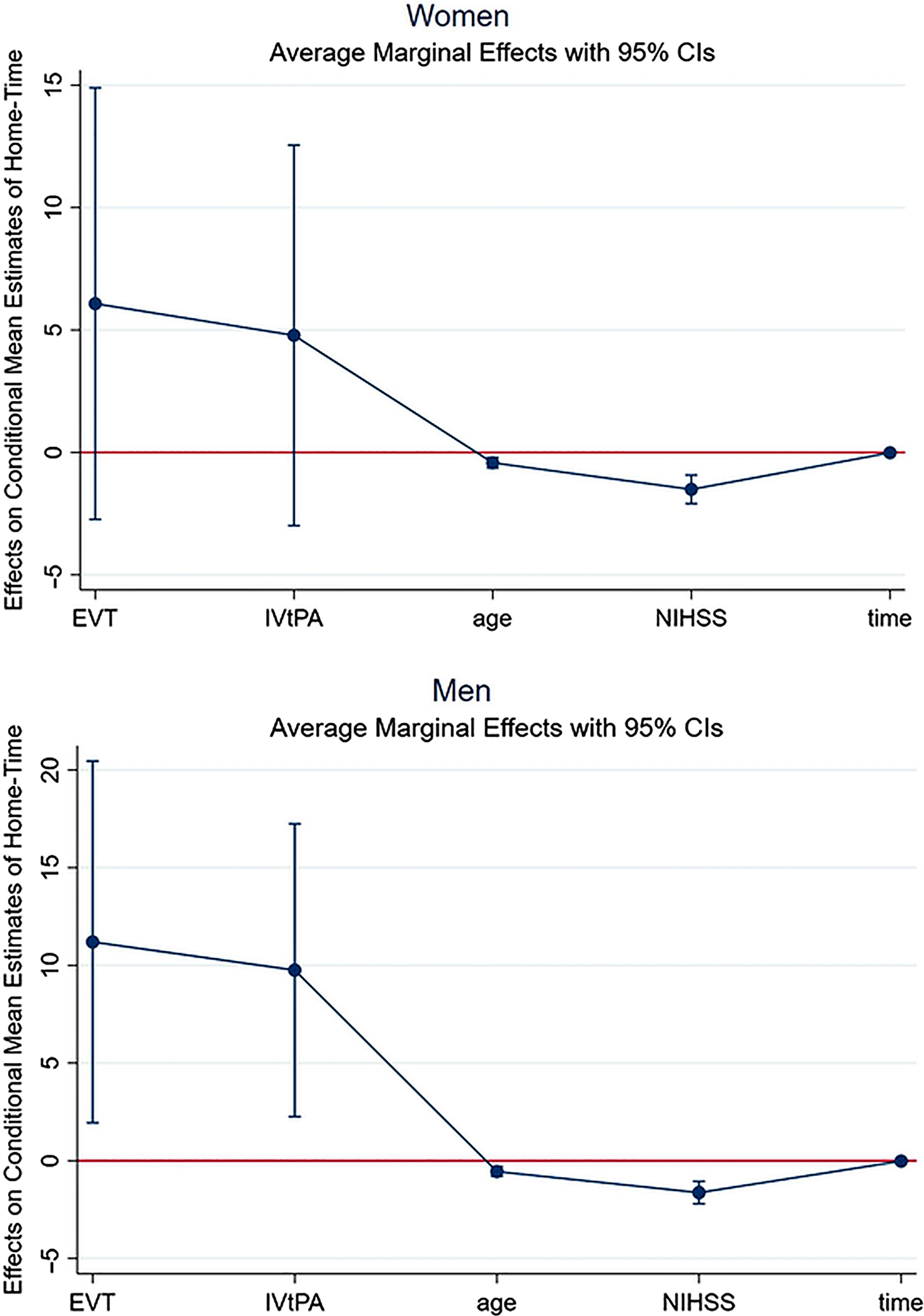
Figure 2: Margins plot showing the effect of baseline variables on the conditional mean estimates of 90-day home-time in the provincial EVT group by sex.
Conditional mean estimate in days (mean, 95% CI) for both sexes for EVT and tPA given are provided in the results section. Further conditional mean estimate in days (mean, 95% CI) for women were age per year older −0.42 (−0.64 to −0.21), NIHSS score per point higher −1.51 (−2.09 to −0.93), and onset-to-treatment time per minute longer −0.01 (−0.03 to −0.00). Further conditional mean estimate in days (mean, 95% CI) for men were: age per year older −0.55 (−0.80 to −0.30), NIHSS score per point higher −1.63 (−2.21 to −1.05), and onset-to-treatment time per minute longer −0.02 (−0.03 to −0.01). EVT = Endovascular Treatment; IV tPA = intravenous alteplase; NIHSS = National Institutes of Health Stroke Scale.
We further explored the difference in 90-day home-time between women and men by stratification according to treatment modality and compared onset-to-treatment time in each stratum between the sexes. Women and men had an equal onset-to-treatment time (within a median of 20 min of each other) in the medical management group if they got both IV alteplase and EVT. However, we found a large difference in median onset-to-treatment time in patients that received endovascular therapy only (IV alteplase ineligible), even though this was not statistically significant. The onset-to-treatment time for women in that group was a median 48 min longer than men, but this delay did not seem to occur in hospital as arrival-to-treatment times were comparable for both sexes (Table 2). When comparing the median and modeled 90-day home-time stratified by age and sex, we saw that the difference in treatment effect between women and men was driven by patients 70 years or older (Table 3).
Table 2: Differences in onset-to-treatment time and arrival-to-treatment time between sexes based on treatment modality

IV=intravenous; EVT=Endovascular Treatment.
Arrival-to-treatment times are not consistently available for the medical management group since the ESCAPE trial only documents arrival at the endovascular-capable center where randomization would occur but for many patients, hyperacute treatment (intravenous alteplase) was initiated at the referral center already.
Table 3: Differences in 90-day home-time (raw data and is derived from Cragg hurdle regression model) of the provincial EVT group stratified by sex and age

The conditional mean estimate refers to the average increase in 90-day home-time when patients have been exposed (in this case received EVT) compared to nonexposed (in this case received medical management).
Since women were on average older than men and treated later than men, we explored if confounding by age and onset-to-treatment time could explain the difference in 90-day home-time. We observed the change in the coefficient of the association of EVT with 90-day home-time in the complete Cragg hurdle regression model compared to Cragg hurdle regression models where either age or onset-to-treatment time had been removed one at a time. For women, the coefficient changed dramatically when removing these variables, whereas it did not for men (Table 4). We, therefore, concluded that the association between EVT and 90-day home-time in women was confounded by age and onset-to-treatment time.
Table 4: Assessment of confounding by age and onset-to-treatment time in Cragg hurdle regression models

There was no association between EVT and mortality at 90 days for either women (OR 0.70, 95% CI 0.36–1.38) or men (OR 0.84, 95% CI 0.42–1.69) in the adjusted analysis. However, older age and higher NIHSS were independent predictors of mortality at 90 days for both sexes (all p < 0.001).
Discussion
In this large population-based study of EVT for large vessel occlusion ischemic stroke assessing 90-day home-time as an outcome, there was no statistically significant difference in outcomes between women and men. However, women consistently had numerically reduced benefits compared to men. This was partly explained (confounded) by age and onset-to-treatment time while arrival-to-treatment times were comparable. This observation suggests that in real-world usage of EVT, women face unique social situations pre-stroke and strategies for equitable access to care for women are needed.
Even though we found no evidence of additive or multiplicative interaction by sex in our study, we saw a direction of effect in that EVT was associated with an increase of 90-day home-time by an average of only 6.08 (95% CI −2.74–14.89, p-value 0.177) days in women compared to an average of 11.20 (95% CI 1.94–20.46, p-value 0.018) days in men. While we cannot argue on the gross outcomes that there is the heterogeneity of treatment effect by sex, the effect difference of more than 5 days in 90-day home-time is a clinically important difference. Further, the identification of confounding by age and interval treatment times is highly relevant.
While age is not modifiable, attitudes toward treatment decisions in the elderly patients are. Women in our cohort were disproportionally older than the men when compared to the pooled analyses of the randomized controlled trials. Although the overall incidence of stroke is higher in men, stroke incidence in women increases sharply after the age of 75 years, to rates exceeding those observed in men, with higher age-specific mortality, greater stroke severity, and increased likelihood of stroke-related disability with higher rates of institutionalization. Reference Bushnell, Reeves and Zhao19,Reference Gall, Tran, Martin, Blizzard and Srikanth20 Thus, the women in our cohort might have had a lower chance of favorable outcomes. However, their age was also higher in the medical management group when compared to men so the magnitude of effect size between treatment and medical management could have been expected to be similar between the sexes.
The time from the first symptoms to receiving treatment can be divided into recognition/alert time, prehospital care time, and the arrival-to-treatment time in the hospital. It is modifiable with attention to the fast recognition of stroke symptoms and quality improvement processes. We found trend differences in the overall median onset-to-treatment time with the largest difference in patients that received endovascular therapy only (IV alteplase ineligible), which was 48 min longer for women compared to men. Part of this might be a lack of awareness of stroke symptoms and women living alone more often than men, resulting in a delay to stroke recognition. With regard to limited data points, we did not find a difference in arrival-to-treatment times once patients reached the hospital in our study. However, the possible existence of differences in attitude toward triaging emergency phone calls, prehospital care, and speed of treatment in hospitals based on the sex of the patient might need to be elucidated through further research.
Other important reasons why there may be outcome differences between women and men are both social and structural. Women are more likely to be institutionalized after stroke either because they are more functionally disabled or because they possibly lack the sufficient social support to return to their community. Reference Katz, Kabeto and Langa21,Reference Lisabeth, Reeves and Baek22 Indeed, 7.62% of women compared to 3.24% of men were discharged to long-term care in our study. The wait for long-term care placement, a pragmatic fact of the Canadian acute hospital care system, in a small proportion of affected individuals might have influenced the 90-day home-time more in women than it did in men. Additionally, numeric home-time may not account for the amount of social and financial support that each patient has that might influence their ability to actually return home, even in a publicly funded healthcare system like Canada’s. Single women, particularly those aged 45–64, experience one of the highest rates of poverty (30%) for any group in Canada. Women also make up the majority of single low-income seniors. 23 Even though we do not have information about the socioeconomic status of the patients in our cohort, these facts might have influenced the 90-day home-time differences between the sexes.
The complete case capture of an entire population in the province of Alberta reflecting real-world practice at a population level is a key strength of our study. Home-time as a patient-centered outcome marker can be established through linkage with administrative health data and thus has the advantage of having complete ascertainment. We do not have comorbidity data and only limited data on the occurrence of symptomatic intracranial hemorrhages or procedural complications. In this respect, home-time obscures some details on the adverse effect of major treatment complications but provides a meaningful global outcome assessment. Further research into the sex differences of adverse outcomes in patients receiving EVT for acute ischemic stroke will be important.
Conclusion
In this province-wide population-based study of EVT for large vessel occlusion ischemic stroke assessing 90-day home-time as an outcome, the trend of reduced benefit for women compared to men was partly explained (confounded) by age and onset-to-treatment time. Future work should explore strategies for more equitable access to care for women and consider their unique social situations pre-stroke and poststroke.
Disclosures
AMD reports personal fees from Medtronic. In addition, he has a patent for Circle NVI issued.
BKM reports board membership and stock ownership with Circle NVI.
MG reports personal fees from Medtronic, Stryker, Microvention, and Mentice.
MDH was the principal investigator of the ESCAPE trial.
The remaining authors have no conflicts of interest to declare.
Statement of Authorship
CZ designed and conceptualized the study, analyzed and interpreted the data, and drafted the manuscript for intellectual content. ER linked the data and revised the manuscript for intellectual content. DMR interpreted the data and revised the manuscript for intellectual content. AMD, NK, BM, TJ, BB, AS, JR, BKM, and MG supported the data acquisition and revised the manuscript for intellectual content. MDH designed and conceptualized the study, interpreted the data, and revised the manuscript for intellectual content.
Funding
CZ holds a Clinician Fellowship Award from Alberta Innovates Health Solutions.
AMD is supported by the Heart & Stroke Foundation of Alberta Chair in Stroke Research.
BKM is supported by the Heart & Stroke Foundation of Alberta Professorship in Stroke Imaging.
MDH reports funding from Alberta Innovates Health Solutions for the QuICR Alberta Stroke Program (Collaborative Research and Innovations Opportunities Team grant) and support from the Heart & Stroke Foundation of Alberta-Hotchkiss Brain Institute Professorship in Stroke Research. The ESCAPE trial was funded by a consortium that included grants to the University of Calgary from Medtronic (Covidien LLC at the time), Alberta Innovates Health Solutions, Heart & Stroke Foundation of Canada, Canadian Institutes for Health Research (Canadian Stroke Prevention Intervention Network), Alberta Health Services, and University of Calgary (Hotchkiss Brain Institute, Department of Clinical Neuroscience, Calgary Stroke Program).








