An 83-year-old man with a history of melanoma resected from the chest 3 years prior presented with 2 weeks of confusion. Brain MRI identified a 4.4 cm enhancing mass (Figure 1A-B). He underwent subtotal resection. Pathology demonstrated glioblastoma (GBM), IDH-wild type, and MGMT promoter unmethylated. Next-generation sequencing revealed microsatellite stability with low tumor mutation burden (3 mutations/Mb), CDK4 amplification, TERT promoter mutation, TP53 mutation, and no EGFR or PDGFRA alterations.
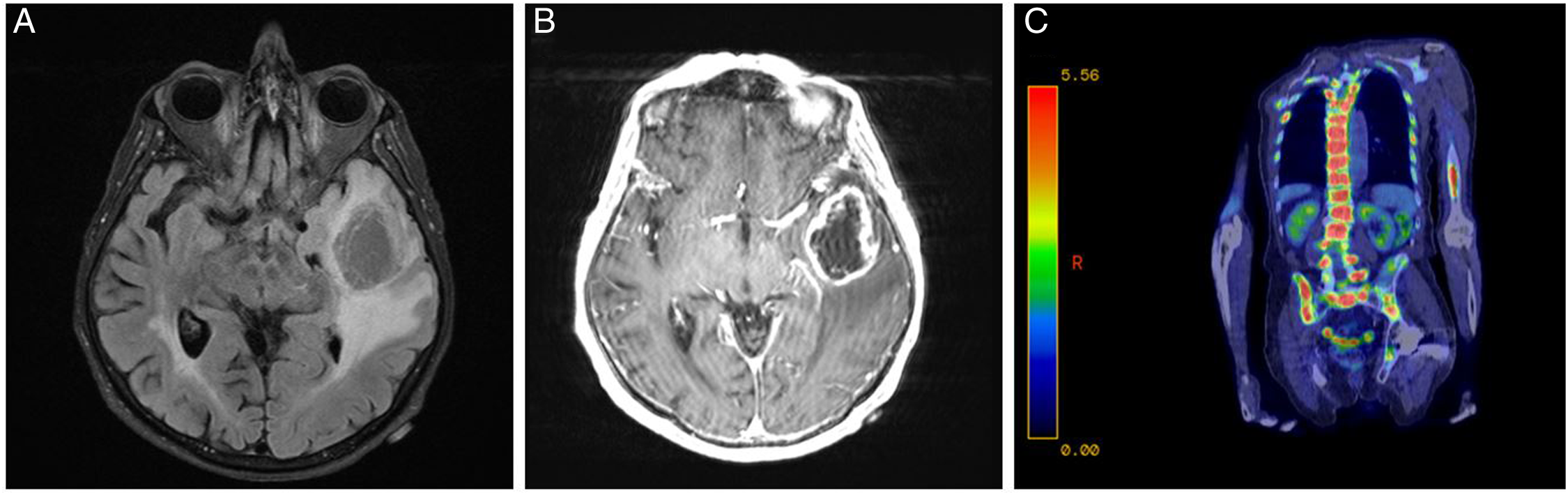
Figure 1: Axial T2 FLAIR MRI of the brain demonstrating a left temporal lobe mass with surrounding vasogenic edema (A) and ring enhancement on MRI of the brain with contrast (B). PET-CT scan showing extensive metastases to the vertebrae and pelvis (C).
He received proton beam radiation therapy (40 Gy) with concurrent and adjuvant temozolomide as part of a clinical trial. Twenty-two months after initial diagnosis, he had radiographic progression. He was treated with bevacizumab with pembrolizumab, added on a compassionate-use basis due to his strong interest in receiving immunotherapy.
Thirteen months later, a lumbar spine CT scan obtained for fall evaluation revealed lytic lesions. A subsequent PET scan showed extensive additional metastases (Figure 1C). CT-guided bone biopsy confirmed the diagnosis of metastatic GBM (Figure 2). The neoplastic cells stained positive for SOX10, synaptophysin, synaptophysin B, GFAP, and OLIG2. The patient experienced rapid clinical deterioration and died four days later.
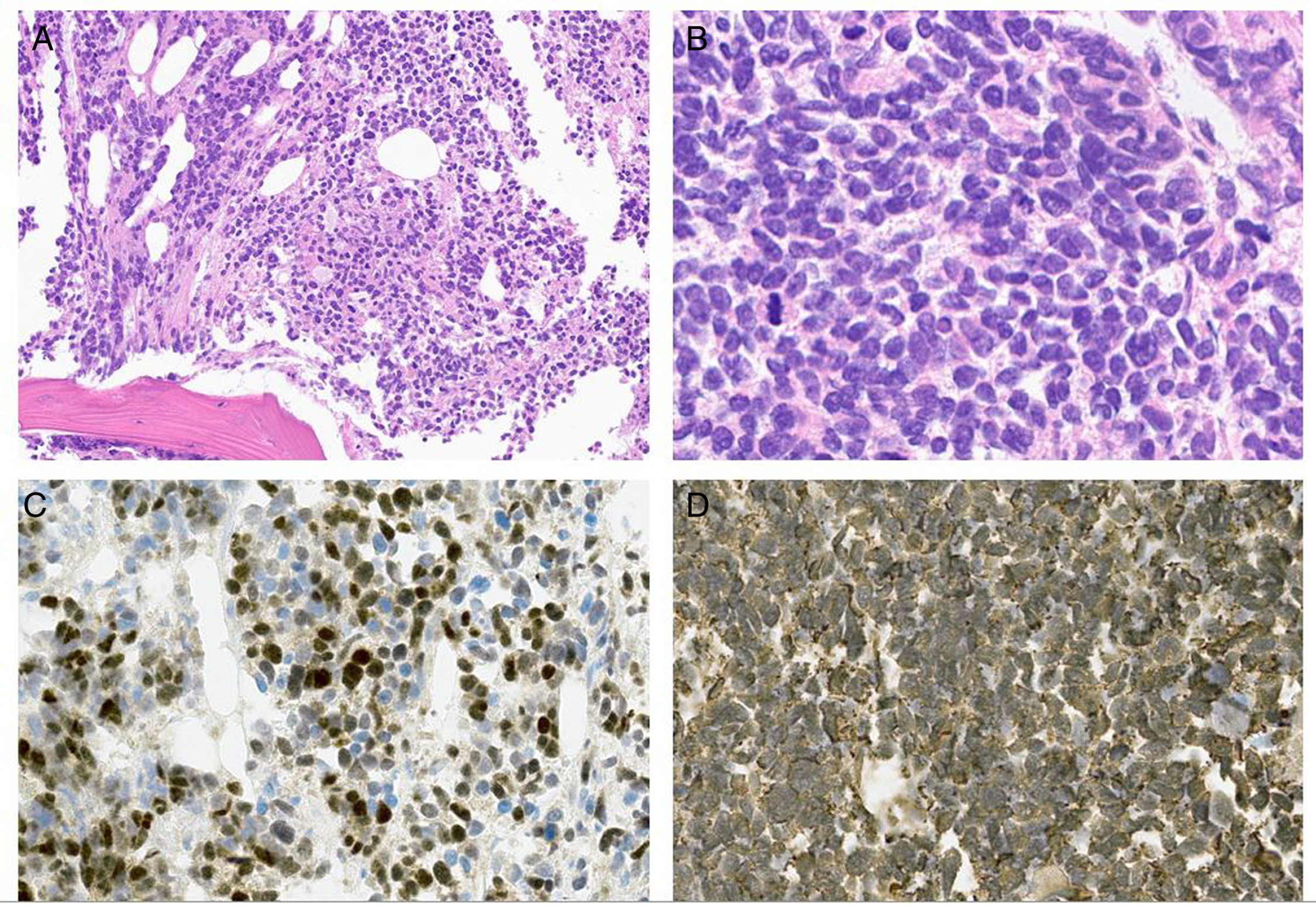
Figure 2: Low-power (A) and high-power (B) images of tumor pathology from pubic bone biopsy with a spicule of trabecular bone visible in the lower left aspect of Figure 2A. The tumor was highly cellular, composed of compact small round cells with scant cytoplasm with scattered mitotic features. Tumor immunostains were positive for OLIG2 (C) and GFAP (D), consistent with glioblastoma.
Extracranial metastasis from GBM is rare, estimated to occur in <2% of cases. Reference Kalokhe, Grimm, Chandler, Helenowski, Rademaker and Raizer1 This rarity has been attributed to the blood-brain barrier, the lack of traditional lymphatics within the brain, immunologic suppression of extracranial GBM growth, and difficulty invading extracranial extracellular matrices. Reference Lah, Novak and Breznik2 GBM’s poor prognosis also temporally limits its opportunity to metastasize. Reference Kumaria, Teale, Kulkarni, Ingale, Macarthur and Robertson3
GBM may spread hematogenously, as circulating tumor cells were detected in 21% of patient’s peripheral blood. Reference Müller, Holtschmidt and Auer4 Some GBM cells can evade the immune response, especially in immunocompromised patients. Reference Lah, Novak and Breznik2 Dissemination through cerebrospinal fluid has also been suggested, especially in those with a ventriculoperitoneal shunt. Reference Kalokhe, Grimm, Chandler, Helenowski, Rademaker and Raizer1 Direct invasion of the skull, the glymphatic system, and transneural spread along peripheral nerves may be other routes for GBM travel. Reference Lah, Novak and Breznik2,Reference Kumaria, Teale, Kulkarni, Ingale, Macarthur and Robertson3
Risk factors for GBM metastasis include male gender and age <60 at diagnosis. Reference Kalokhe, Grimm, Chandler, Helenowski, Rademaker and Raizer1 Gliosarcomas, accounting for 2% of all glioblastomas, more frequently metastasize extracranially. Reference Wirsching, Galanis and Weller6 EGFR amplification has been discovered in cases of GBM metastasis with circulating tumor cells. Reference Müller, Holtschmidt and Auer4 BRAF-targeted therapy has achieved a clinical response in both intracranial and extracranial metastatic GBM. Reference Munjapara, Heumann and Schreck7 While our patient did not have a diagnosis of gliosarcoma and no EGFR or BRAF mutations were identified in his tumor, bevacizumab has also been associated with early GBM metastasis, which he received at the time of his first progression. Reference Pàez-Ribes, Allen and Hudock5
Metastatic GBM most commonly involves bone (38%), lymph nodes (37%), lungs (32%), and liver (18%), Reference Kalokhe, Grimm, Chandler, Helenowski, Rademaker and Raizer1 all active on our patient’s PET scan. Osseous metastases, which may be lytic or sclerotic, are mostly to thoracic vertebrae and may spread hematogenously via the surrounding extensive venous plexus. Reference Strong, Koduri and Allison8
Due to the limited number of cases, optimal management and prognostic implications of extracranial GBM metastases remain unclear. Reference Kalokhe, Grimm, Chandler, Helenowski, Rademaker and Raizer1 Incidence of extracranial metastasis will likely increase with development of improved therapeutics for GBM. Despite its rarity, clinicians should be aware of GBM’s potential to metastasize, as this pattern of spread can significantly impact patient’s quality of life.
Funding
This research was in part funded by the grant number UL1 TR002377 from the National Center for Advancing Translational Sciences.
Competing interests
The authors do not have any conflicts of interest to disclose.
Statement of authorship
L.W. performed a literature review and drafted the manuscript, J.L.C. cared for the patient and critically reviewed the manuscript, S.J.C. cared for the patient and critically reviewed the manuscript, M.R. reviewed the pathology, provided pathology imaging, and critically reviewed the manuscript, U.S. conceptualized and supervised the work, cared for the patient, and critically reviewed the manuscript.




