Pituitary tumors may become symptomatic in pregnancy. While uncommon, non-functioning pituitary adenomas (NFPA) may enlarge and produce a bitemporal visual field defects during pregnancy. These patients are often treated with surgery as chiasmal compression poses a risk of permanent visual deficits and as medical therapy with dopamine agonists is unlikely to reduce the tumor size. We here present a unique case of a patient who presented with bitemporal hemianopia due to chiasmal compression from a NFPA. She declined surgical management and made a complete visual recovery post-partum, despite post-partum images continuing to show chiasmal compression without a significant change in tumor size.
A 27-year-old woman was referred to neuro-ophthalmology for a 2-month history of left greater than right vision loss. She was 17 weeks pregnant (G5P1), but otherwise healthy and on no medications. Initial examination revealed a visual acuity of 20/20 OD and 20/30-2 OS. Humphrey 24-2 SITA-Fast visual fields (HVF) showed a left greater than right bitemporal hemianopia (Figure 1A). Optical coherence tomography (OCT) of the macular ganglion cell-inner plexiform layer (GCIPL) showed very subtle binasal thinning (Figure 1C). An MRI of the sella with contrast was performed and showed a “snowman-shaped” intrasellar and suprasellar, 24 × 20 × 17 mm mass compressing the optic chiasm (Figure 2A). The mass had cystic changes at the suprasellar component, which demonstrated intrinsic T1 hyperintensity within the cyst. The patient had normal endocrinological evaluation in the context of her pregnancy, which included normal adrenocorticotropic hormone (5.4 pmol/L), growth hormone (2.3 µg/L), prolactin (91.1 µg/L), and thyroid-stimulating hormone (1.89 µIU/mL). A neurosurgical consultation recommended surgical resection with the goal of improving and preserving her vision. The patient declined surgical intervention and decided to reconsider after delivery. Her visual field remained essentially stable throughout pregnancy. She delivered her baby via C-section after which she decided to reconsider surgery. However, she noticed a significant improvement in her visual field 5-month post-partum. She continued to notice a gradual improvement over the next several months and at the 15-month post-partum follow-up, her visual acuity was 20/20 in both eyes, HVF was normal (Figure 1B) and OCT GCIPL showed binasal atrophy (Figure 1D). A repeat MRI sella showed stable size of the intrasellar and suprasellar mass with interval decrease in T1 signal of the suprasellar cystic component (Figure 2B). There was stable mass effect on the optic chiasm and pre-chiasmatic optic nerves with the interval development of high T2-signal in the optic nerves.
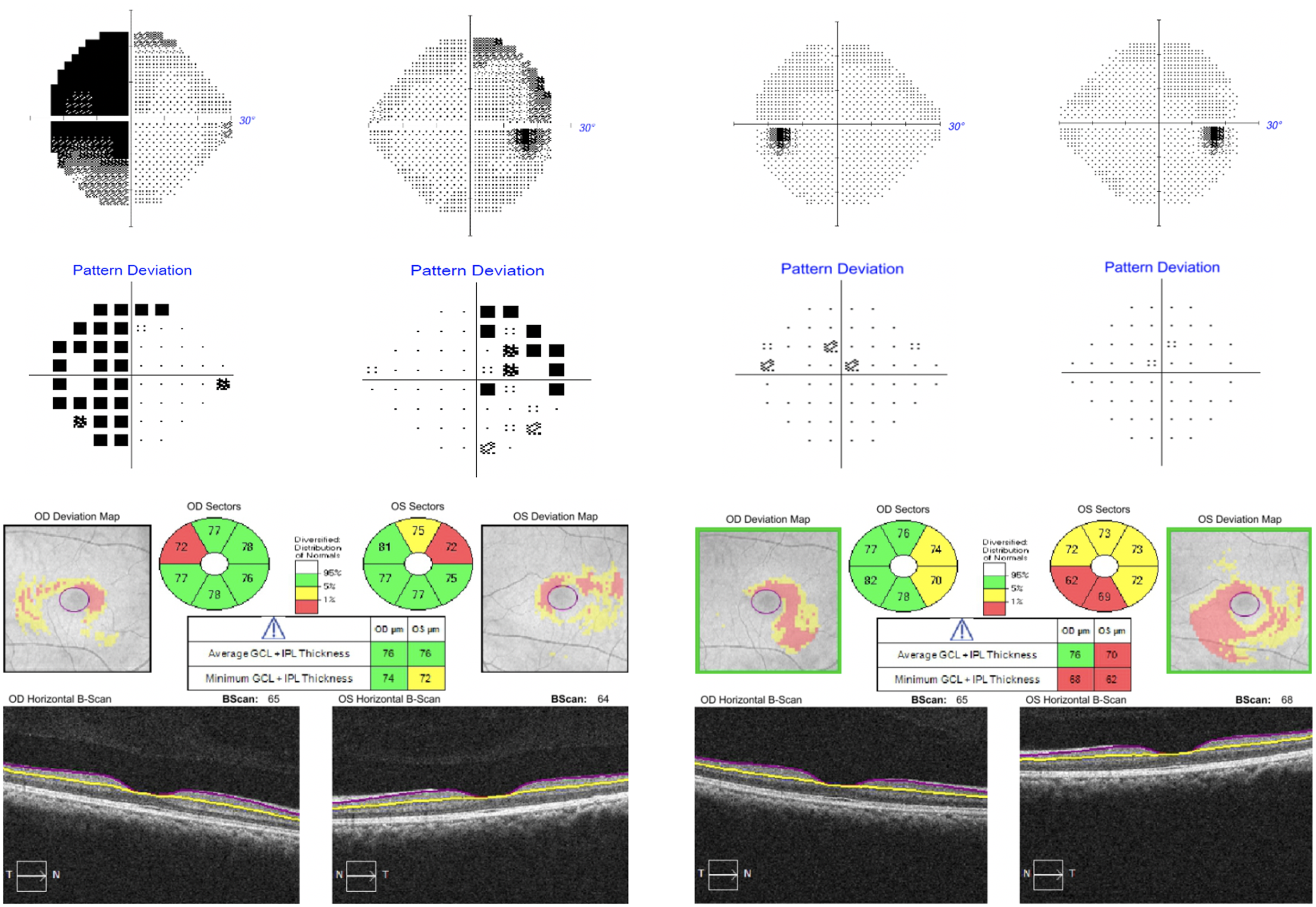
Figure 1: Humphrey 24-2 SITA-Fast visual fields at presentation (A, top left) and final follow-up (B, top right). OCT macular ganglion cell analysis at presentation (C, bottom left) and final follow-up (D, bottom right).
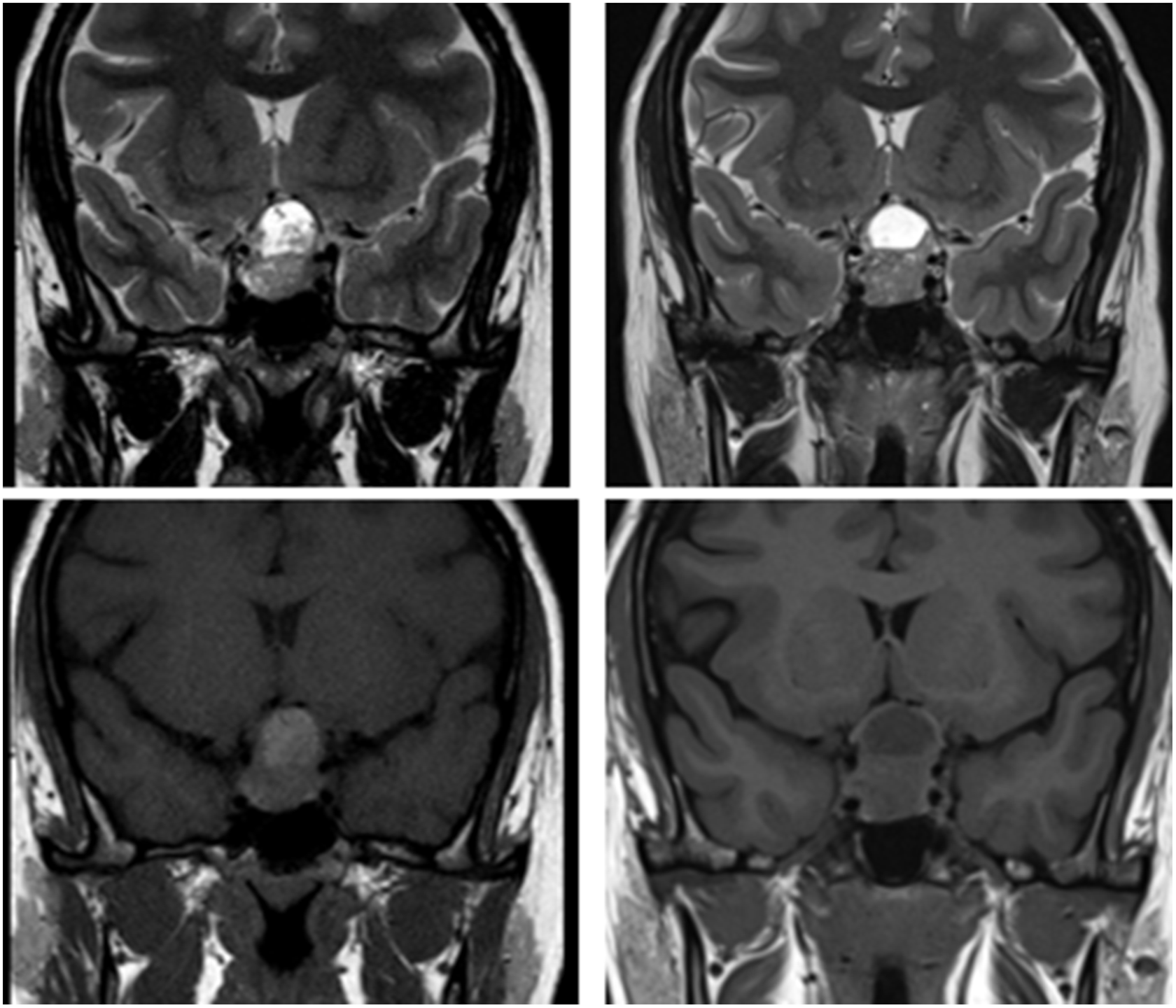
Figure 2: Magnetic resonance imaging at presentation (A) demonstrating T2 (top left) and T1 sequences (bottom left) at presentation and final follow-up (B) demonstrating T2 (top right) and T1 sequences (bottom right).
We here presented a rare case of a NFPA that became symptomatic during pregnancy. The patient declined surgical management and surprisingly made a complete recovery post-partum despite continued chiasmal compression and unchanged tumor size on MRI. We were able to retrieve no other cases of spontaneous improvement of visual field defects post-partum without treatment or surgery in patients with NFPA. Masding et al. presented a similar case of a 29-year-old woman with a NFPA who became symptomatic during pregnancy due to upward tumor displacement from physiologic pituitary hyperplasia. Reference Masding, Lees, Gawne-Cain and Sandeman1 The patient made a complete recovery after therapy with bromocriptine. Similar to our case, the tumor remained stable in size although unlike our case, there was resolution of chiasmal compression.
Spontaneous improvement of visual symptoms and tumor regression has been reported in other pituitary tumors that become symptomatic during pregnancy. Fujimoto et al. described a 27-year-old woman who developed decreased visual acuity, ptosis, and oculomotor palsy in early pregnancy from a large prolactinoma. She was scheduled for surgical excision; however, her symptoms resolved spontaneously 1-month post-partum. Oljenic et al. reported a woman with intermittent visual field disturbances due to chiasmal compression from a suprasellar meningioma. She developed recurrent visual field defects toward the end of all her seven pregnancies. Reference Michelsen and New2 These changes spontaneously resolved post-partum. Ikheda et al. reported a 29-year-old woman who developed headache and visual field defects in the third trimester from lymphocytic hypophysitis. Reference Ikeda and Okudaira3 Her symptoms spontaneously resolved 3-month post-partum with resolution of pituitary mass on imaging. We found one patient where symptomatic improvement was observed despite unchanged imaging appearance. Kinoshita et al. reported a 15-year-old boy with bitemporal hemianopia associated with physical exercise and imaging appearance of chiasmal compression by pituitary hyperplasia. Reference Kinoshita, Yamasaki, Tominaga, Usui and Kurisu4 His symptoms resolved six months after onset despite no changes on imaging. They postulated that transient increase in blood supply due to hormonal factors may have resulted in transient pituitary enlargement and compression.
There are a few potential explanations for the resolution of visual field defects despite ongoing chiasmal compression and insignificantly changed tumor size. It is possible that reduction in size of the pituitary gland post-partum resulted in decreased chiasmal compression. While the chiasmal compression in our case remained insignificantly changed on MRI, size of the pituitary increases during pregnancy decreases 4 days post-partum and gradually returns to normal size within 6 months. Reference Dinč, Esen, Demirci, Sari and Gümele5 Physiologic increase in pituitary size may have impacted the degree of compression between the optic chiasm and NFPA. These subtle changes may have not been detected by imaging. In addition, our patient noticed significant improvement 5-month post-partum, which correlates with the expected period when the pituitary gland returns to normal size. Pituitary apoplexy is another possibility as the initial MRI demonstrated T1 hyperintensity, which may be due to accumulation of subacute (4–21 days) blood or highly proteinaceous fluid – these changes were resolved on follow-up MRIs. It is also possible that the increase in circulating blood volume resulted in increased chiasmal compression not obvious on MRI. In pregnancy, plasma volume starts to increase in the first trimester by about 8%. It has a steep increase in second trimester to 18% and gradually increases to 48% of normal plasma volume by 35–38 weeks. This may have resulted in subtle compression and distortion of the inferior pial network of blood vessels which supplies the chiasm. An additional possibility is vascular shunting and ischemia caused by tumor-induced intracellular or extracellular fluid shifts. These subtle changes through a compressive or ischemic process may explain the improvement in symptoms despite stable imaging appearance. Radiological compression of the optic chiasm without visual field defects is a rare but known observation in the literature, in keeping with our hypothesis that hemodynamic changes in setting of pregnancy may have contributed to our patient’s visual deficits and subsequent recovery. Reference Frisén and Jensen6
To conclude, we here presented a unique case of spontaneous resolution of bitemporal hemianopia from a pituitary adenoma, despite an insignificant change in the appearance of chiasmal compression on magnetic resonance imaging. This case suggests that observation may be reasonable during pregnancy in patients wishing to avoid surgical risks.
Acknowledgement
This manuscript does not include any nonauthor contributors to acknowledge.
Author contributions
Category 1: a. Conception and design: Amir R. Vosoughi and Jonathan A. Micieli; b. Acquisition of data: Amir R. Vosoughi, Jonathan A. Micieli; c. Analysis and interpretation of data: Amir R. Vosoughi and Jonathan A. Micieli. Category 2: a. Drafting the manuscript: Amir R. Vosoughi and Jonathan A. Micieli; b. Revising it for intellectual content: Amir R. Vosoughi, Felix Tyndel, Suradech Suthiphosuwan, Jonathan A. Micieli. Category 3: a. Final approval of the completed manuscript: Amir R. Vosoughi, Felix Tyndel, Suradech Suthiphosuwan, and Jonathan A. Micieli.
Disclosures
The authors do not have any conflicts of interest to disclose.




