Pancreatic cancer is the seventh leading cause of cancer-related deaths worldwide. Distant metastases have been reported in up to 75% of patients. Reference Hishinuma, Ogata, Matsui and Ozawa1 Pancreatic cancer patients may rarely present with neuro-ophthalmic findings such as diplopia, relative afferent pupillary defects (RAPDs), and optic disc edema (ODE) due to metastasis to the orbit, choroid, and optic nerve nerve. Reference Shields, Welch and Malik2 Here, we present a rare manifestation of pancreatic cancer metastases, bilateral ODE with preserved visual function due to optic nerve sheath (ONS) metastases.
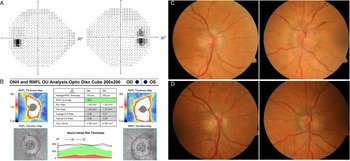
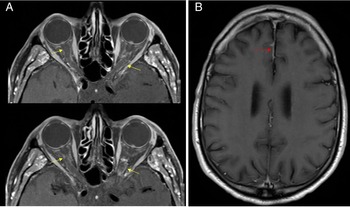
A 75-year-old man was referred to neuro-ophthalmology for transient diplopia. He had a history of pancreatic adenocarcinoma diagnosed 13 months prior and treated with 13 cycles of gemcitabine and Abraxane chemotherapy. Due to local recurrence of disease, he had a pyloric stent inserted. His most recent computed tomography of the thorax/abdomen/pelvis 1 month prior to presentation showed three small hypoattenuating liver lesions consistent with metastases and a stable locally infiltrative pancreatic head mass. Two weeks prior to presentation, he developed lightheadedness and transient vertical binocular diplopia for a few minutes when looking upward. He was referred to neuro-ophthalmology for this visual change. Examination revealed visual acuity of 20/20 in both eyes, and Humphrey 24-2 SITA-Fast visual fields were normal (Figure 1A). Pupils were equal sizes and reactive to light without a RAPD. Dilated fundus examination revealed moderate bilateral ODE with peripapillary hemorrhages in the left eye (Figure 1C). Optical coherence tomography of the retinal nerve fiber layer showed an average thickness of 260-um right eye and 329-um left eye (Figure 1B). The remainder of the macula and peripheral retina were normal in both eyes. He underwent an magnetic resonance imaging (MRI) of the brain, orbits, and magnetic resonance venography of the brain with contrast which showed patchy enhancement of the ONSs on both eyes and leptomeningeal disease along the right frontal parasagittal region (Figure 2). This was thought to represent leptomeningeal and ONS metastatic deposits. He underwent a lumbar puncture in the left lateral decubitus position, and this showed an opening pressure of 15 cm of water and with normal cerebrospinal fluid protein and glucose. Malignant cells consistent with pancreatic adenocarcinoma were detected on cytological analysis. He underwent palliative radiotherapy (20 Gy in five fractions) to the whole brain. Neuro-ophthalmology follow-up 3 months after revealed stable and normal visual function (20/20 in both eyes and normal Humphrey 24-2 SITA-Fast visual fields). The ODE considerably improved (Figure 1D). His overall condition deteriorated and he died 2 months later.

Figure 1: (A) Humphrey 24-2 SITA-Fast visual fields at presentation were normal in both eyes. (B) OCT RNFL at presentation demonstrated elevated RNFL in both eyes. (C) At presentation, there was bilateral optic disc edema with left peripapillary hemorrhages in the left eye that significantly improved 3 months later (D).

Figure 2: (A) Magnetic resonance of the orbits with contrast demonstrating patchy enhancement of the optic nerve sheaths on both eyes. (B) MRI of the brain with contrast showed a small area of frontal leptomeningeal enhancement along the right frontal lobe.
Overall, leptomeningeal metastasis (LM) develops in 5%–8% of metastatic cancer cases. However, the incidence of LM in pancreatic cancer is incredibly low, with Farahvash et al. Reference Farahvash, Knox and Micieli3 finding only 19 English cases in their literature review, and describing the only previous case of leptomeningeal disease from pancreatic cancer involving the optic nerve. However, this patient presented with complete vision loss (no light perception) and had a much different presentation than our patient whose bilateral ODE was incidentally discovered. The reason for our patient’s preservation of vision was likely due to only involvement of the ONS with possible secondary inflammation rather than involvement of the optic nerve substance itself. Our patient had no signs or symptoms of raised intracranial pressure, and the opening pressure was within a normal range, indicating that it was not papilledema.
The most common cause of bilateral ODE with preserved visual function is papilledema. It is important, however, to consider other causes of bilateral ODE with preserved visual function in patients with cancer such as ONS metastases. We were unable to find another case of cancer with ONS involvement with preserved visual function, and there are numerous cases of ONS metastases causing ODE with visual decline. Gasperini et al. Reference Gasperini, Black and Van Stavern4 report a case of ONS metastases secondary to breast cancer. Visual decline in this case was thought to be due to direct infiltration of the ONS subsequently causing a compressive optic neuropathy. A similar case was documented by Lui and Margolin, Reference Liu and Margolin5 who reported papilledema and an optic neuropathy secondary to leptomeningeal carcinomatosis. This patient had marked generalized depression of the visual fields at neuro-ophthalmology presentation. McFadzean et al. Reference McFadzean, Brosnahan, Doyle, Going, Hadley and Lee6 present a case of sudden vision loss secondary to leptomeningeal carcinomatosis from rectal cancer. In their patient, postmortem histological analysis demonstrated dense infiltration of the subarachnoid space surround the optic nerves with metastatic rectal adenocarcinoma cells. These cases highlight that ONS metastases may reduce visual function by direct infiltration and compression of the ONS itself, as well as infiltration of the subarachnoid space with metastatic cells that then compress the optic nerve.
Optic perineuritis (OPN) is an inflammatory disorder of the ONS that can be idiopathic or occur secondary to systemic conditions such as vasculitis. Reference Purvin, Kawasaki and Jacobson7 While optic nerve inflammation usually results in visual deficits, inflammation of the ONS alone may preserve visual function. Yu et al. Reference Yu and Micieli8 reported a case of OPN secondary to microscopic polyangiitis, with bilateral ODE and preserved visual function. Parker and Pula Reference Parker and Pula9 report a case of a 41-year old male who initially presented to ophthalmology with bilateral ODE and preserved visual acuity ultimately diagnosed with OPN secondary to neurosyphilis. A review by Purvin et al. Reference Purvin, Kawasaki and Jacobson7 showed seven OPN patients with BCVA 20/20 or better in their affected eye at initial presentation (50% of included patients). Inflammation of the ONS may lead to thickening from subsequent fibrosis. Reference Parker and Pula9 While fibrosis of the ONS may eventually cause compression of the optic nerve and a subsequent visual defect, some patients may maintain good visual function throughout the disease course.
In conclusion, pancreatic adenocarcinoma may metastasize to the ONS and cause bilateral ODE with preserved visual function. Although this presentation is usually due to papilledema, this case adds to the differential diagnosis of this presentation. As a consequence of advancements in diagnostic and treatment therapies for pancreatic adenocarcinoma, more patients are living longer and may develop metastases to irregular locations. Clinicians should be vigilant of this as timely diagnosis and treatment may improve quality of life in these patients.
Funding
None.
Conflicts of Interest
None.
Statement of Authorship
Conception and design (ABP, JAM), Data Collection (ABP, JAM), Drafting the manuscript (ABP), Critical revisions (JAM), Final approval (ABP, JAM).