Hydrocephalus caused by aqueductal stenosis (AS) is a poorly characterized subtype of hydrocephalus. Although most cases of AS-induced hydrocephalus occur during childhood, rare cases have been observed in adulthood and are classified as an adult chronic subtype.Reference Rodis, Mahr, Fehrenbach, Meixensberger, Merkenschlager and Bernhard 1 As a result a detailed neurological presentation of late-onset AS has not been well described, although a variable degree of akinetic-rigid parkinsonism may be seen in patients with obstructive as well as normal-pressure hydrocephalus. We describe here an elderly male with AS-associated hydrocephalus who presented with a symptom similar to pure akinesia with gait freezing (PAGF),Reference Williams, Holton, Strand, Revesz and Lees 2 suggesting that clinicians should consider the possibility of hydrocephalus, a treatable disease, when diagnosing patients with PAGF phenotype.
A 68-year-old man with no family history of movement disorders was admitted to our hospital because of a year-long gait disturbance. Initially he had occasional start hesitation, but his freezing of gait gradually worsened, and he started to fall six months later. A neurological examination showed a moderate to severe degree of symmetric bradykinesia without rigidity or tremor. The dominant feature was a freezing of gait that prevented the patient from walking without assistance (Video 1). His hypotonic dysarthria was sometimes combined with freezing of speech. During a bedside examination his eye movement did not demonstrate any definite abnormality of saccade or smooth pursuit. The patient did not exhibit urinary or sleep problems, visual hallucinations, or constipation. His wife reported that he had memory disturbances over the past several months. A neuropsychological assessment demonstrated a severe impairment in executive function and a moderate impairment in memory function. However, other higher cortical functions, including attention, visuospatial, and linguistic, were preserved. A 300 mg/day treatment of levodopa did not improve the patient’s PAGF.
A 1.5-T brain MRI revealed not only enlargement of the lateral ventricles, but also a periventricular hyperintensity in contact with the lateral ventricles in axial fluid attenuated inversion recovery (FLAIR) images (Figures 1A and B). The Evans’ index was 0.35, indicating hydrocephalus. Coronal T2-weighted images featured enlarged ventricles; tight, high-convexity, and medial surface subarachnoid spaces; and a bilaterally expanded Sylvian fissure (Figure 1C), suggesting disproportionately enlarged subarachnoid-space hydrocephalus (DESH).Reference Hashimoto, Ishikawa, Mori and Kuwana 3 , Reference Virhammar, Laurell, Cesarini and Larsson 4 T1 sagittal images revealed AS without any obstructive lesion (Figure 1D).
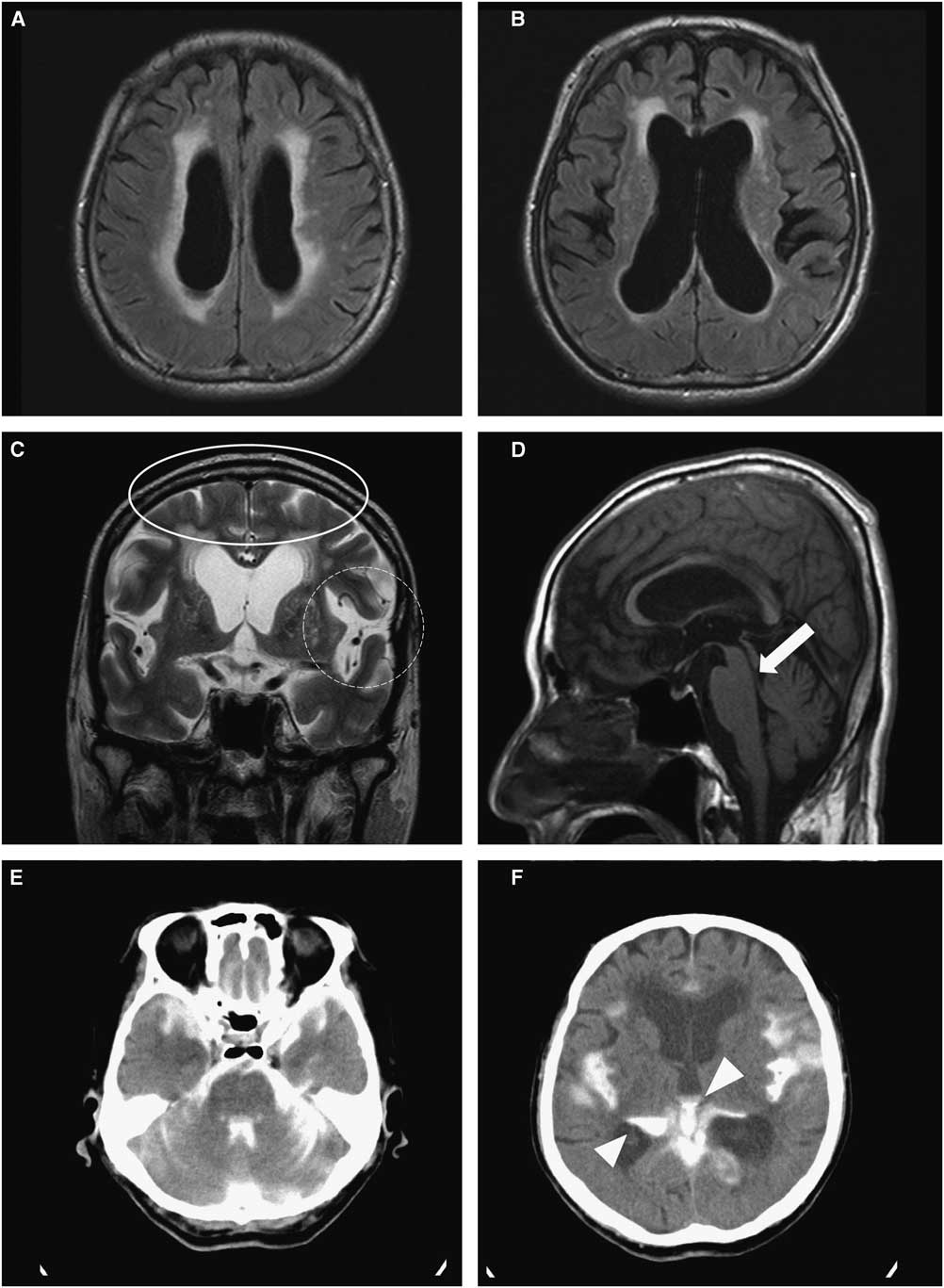
Figure 1 Brain MRI and CT cisternography of the patient revealing hydrocephalus with idiopathic aqueductal stenosis: (A & B) Enlargement of lateral ventricles and periventricular hyperintensity regarded as interstitial edema. (C) Narrow medial sulci (oval ring) and bilaterally dilated Sylvian fissure (dotted round ring), indicating disproportionately enlarged subarachnoid-space hydrocephalus (DESH). (D) Aqueductal stenosis with no obstructive mass or lesion (white arrow). (E & F) CT cisternography five hours after lumbar introduction of metrizamide, showing filling of the fourth ventricle as well as the Sylvian fissure and only a partial filling in the third and lateral ventricles (white arrow heads).
We performed brain metrizamide dynamic CT cisternography on the patient. Five hours later CT cisternography showed a full filling of the fourth ventricle (Figure 1E) but only a small filling of the third and lateral ventricles (Figure 1F), indicating a partial obstruction of AS-associated hydrocephalus. The patient’s gait difficulty was considerably improved after draining approximately 30 cc of cerebrospinal fluid (CSF) from the lumbar cistern; opening pressure at the lumbar puncture was 16 cmH2O. Since the patient responded moderately to CSF drainage, a ventriculoperitoneal (VP) shunt was applied. After the VP shunt operation, the patient’s PAGF symptoms were notably improved without any medication (Video 2). He improved until about two months later, when he died suddenly from an unknown cause.
Idiopathic AS is generally regarded as one of the important etiologies of obstructive hydrocephalus.Reference Zeidler, Dorman, Ferguson and Bateman 5 In our case, however, metrizamide CT cisternography demonstrated an incomplete type of obstructive hydrocephalus, as previously described (Figures 1E and F). Furthermore, the MRI findings were compatible with DESH (Figure 1C), a characteristic feature of idiopathic normal pressure hydrocephalus.Reference Hashimoto, Ishikawa, Mori and Kuwana 3 , Reference Virhammar, Laurell, Cesarini and Larsson 4 In line with our findings, Rodis et al. stated that most cases of late-onset AS resembled typical signs and symptoms of normal pressure hydrocephalus.Reference Rodis, Mahr, Fehrenbach, Meixensberger, Merkenschlager and Bernhard 1 Therefore, our case may indicate that adult chronic AS-associated hydrocephalus could be a transitional status between obstructive and normal-pressure hydrocephalus. It is reasonable to infer a common mechanism between idiopathic normal-pressure hydrocephalus and an incomplete type of obstructive hydrocephalus; some communicating portion of aqueductal stenosis might be responsible for the pathophysiology. In addition, we supposed that was the reason why the patient showed the improvement of gait difficulty after CSF drainage with the lumbar puncture.
A recent study reported that a VP shunt operation led to slight improvement in parkinsonism in some progressive supranuclear palsy (PSP) pathological conditions.Reference Magdalinou, Ling, Smith, Schott, Watkins and Lees 6 However, it has been widely accepted that the parkinsonism in PSP is not relieved by a VP shunt. Since long-term follow-up of the patient was not possible, we cannot completely rule out the possibility of PSP pathology. However, the patient’s MRI showed findings that are typical of AS-associated hydrocephalus without remarkable midbrain atrophy. Furthermore, VP shunting considerably improved the patient’s PAGF, as seen in the videos. We therefore propose that the patient’s symptoms were comparable to those of a chronic adult AS-associated hydrocephalus,Reference Rodis, Mahr, Fehrenbach, Meixensberger, Merkenschlager and Bernhard 1 rather than a PAGF subtype of PSP. Although we could not fully exclude the placebo effect, we assumed that such a considerable improvement was mainly due to the VP shunt operation, rather than the placebo effect.
In conclusion, we suggest that hydrocephalus should be considered as a possible etiology for the PAGF-mimicking phenotype.
ACKNOWLEDGEMENTS
This work was supported by the Soonchunhyang University Research Fund.
DISCLOSURES
Kyum-Yil Kwon and Dong-Kyu Yeo do not have anything to disclose.
SUPPLEMENTARY MATERIAL
To view supplementary material for this article, please visit https://doi.org/10.1017/10.1017/cjn.2016.328



