In the setting of acute trauma, low-density cerebrospinal fluid may enter and accumulate within the subdural space through an arachnoid membrane tear resulting in an acute traumatic subdural hygroma. Acute subdural hygromas are a relatively common post-traumatic mass lesion with its incidence being reported as 5–20%. Reference Lee1 When mixed with acute subdural hemorrhage, the resulting mixed density acute subdural hematohygroma (ASHH) is often misdiagnosed as an acute-on-chronic subdural hematoma (ACSH). The erroneous assumption of an underlying chronic component may underestimate the severity of a patient’s acute injury, and it may occur even when recent prior imaging demonstrates no pre-existing subdural collection. Accurate characterization of the acuity and severity of injury may influence the choice of surgical technique. Radiologists at trauma centres face the challenge of differentiating between ACSH and ASHH when imaging demonstrates mixed density extra-axial collections.
In the setting of acute trauma, a radiologist must avoid automatically pronouncing a mixed density subdural collection as acute-on-chronic, and should instead consider the differential of ASHH. Imaging findings that support a diagnosis of ASHH include the following: 1. Significant mass effect, sulcal effacement, and midline shift. 2. Sharp delineation between low density and high density components. 3. Absence of internal strand-like areas of intermediate density associated with chronic subdural hematoma. Figure 1 shows these findings in a case of ASHH while Figure 2 shows a case of ACSH. It is also essential to review previous imaging studies which may establish the presence or absence of a pre-existing subdural hematoma. Accurate diagnosis of ASHH can lead to improvements in patient outcomes through appropriate selection of therapeutic options and surgical techniques as well as furthering knowledge of its imaging characteristics, natural history and evolution.
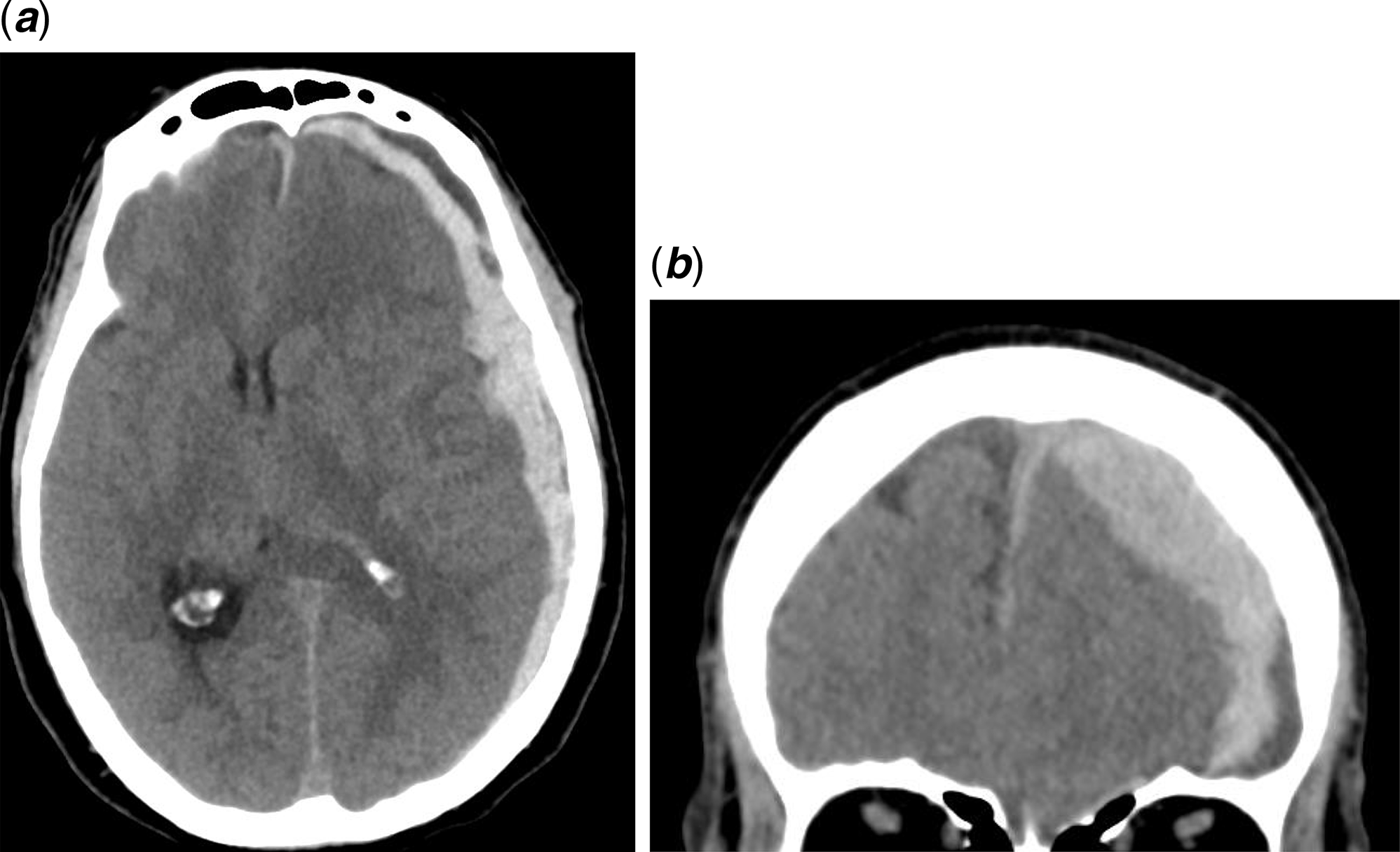
Figure 1: Axial (A) and coronal (B) view of a CT scan of the head for a 76-year-old male with an acute subdural hematohygroma. This patient presented with a history of headache, confusion and falls and was on anticoagulants. There is sulcal effacement notable on the coronal view and midline shift is present. There is a sharp delineation between low density and high density components. There is a lack of strand-like areas of intermediate density.
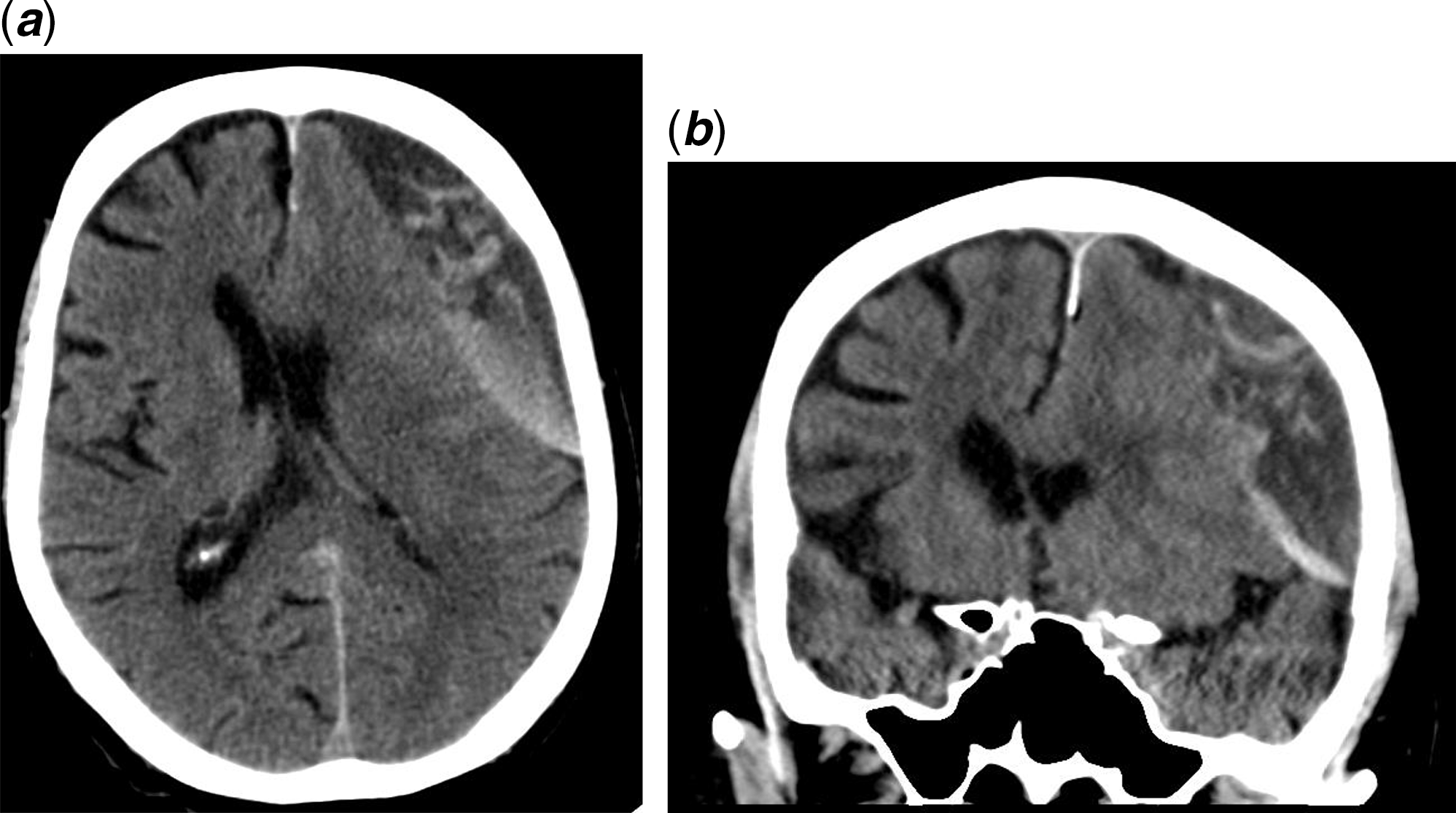
Figure 2: Axial (A) and coronal (B) view of a CT scan of the head for an 88-year-old male with an acute-on-chronic subdural hematoma. This patient presented with right arm weakness since the morning and a history of headaches following a head injury from a syncopal episode 1 month ago (CT head was negative at that time). There are strands of intermediate density associated with chronic subdural hematoma and hazy delineation between low density and high density components.
Disclosures
The authors have no conflicts of interest to declare.
Statement of Authorship
T.E. – Drafting the manuscript.
N.K. – Guidance, supervision and revision of the manuscript.




