A 65-year-old healthy woman presented with a 15-year history of binocular horizontal diplopia worse when looking left. She had previously been thoroughly investigated multiple times for a left sixth nerve palsy (6NP) 15 years ago and had three normal magnetic resonance imaging (MRI) scans of the brain/orbits with contrast, normal acetylcholine receptor antibodies, normal thyroid function tests, normal cerebrospinal fluid, and normal nerve conduction studies and single-fibre electromyography. She was treated with prism glasses, which resulted in resolution of her symptoms in primary position.
She re-presented due to worsening of her double vision and was symptomatic with her prism glasses in primary position for 6 weeks. She had an incomitant esotropia that measured 20 prism diopters in primary position with a left abduction deficit of 50% of normal (Figure 1A). Due to the numerous previously normal investigations and chronic course, neurovascular compression was suspected. 3-Tesla MRI of the brain, including a high-resolution, three-dimensional, T2-weighted SPACE sequence (voxel size 0.5 mm isotropic) covering the posterior fossa, showed contact between the anterior inferior cerebellar artery (AICA) and the left abducens nerve at the nerve root entry zone (Figure 1B–E), which was the likely cause of her 6NP. She was treated with Fresnel prisms and her symptoms resolved and the orthoptic measurements remained stable for 6 months.
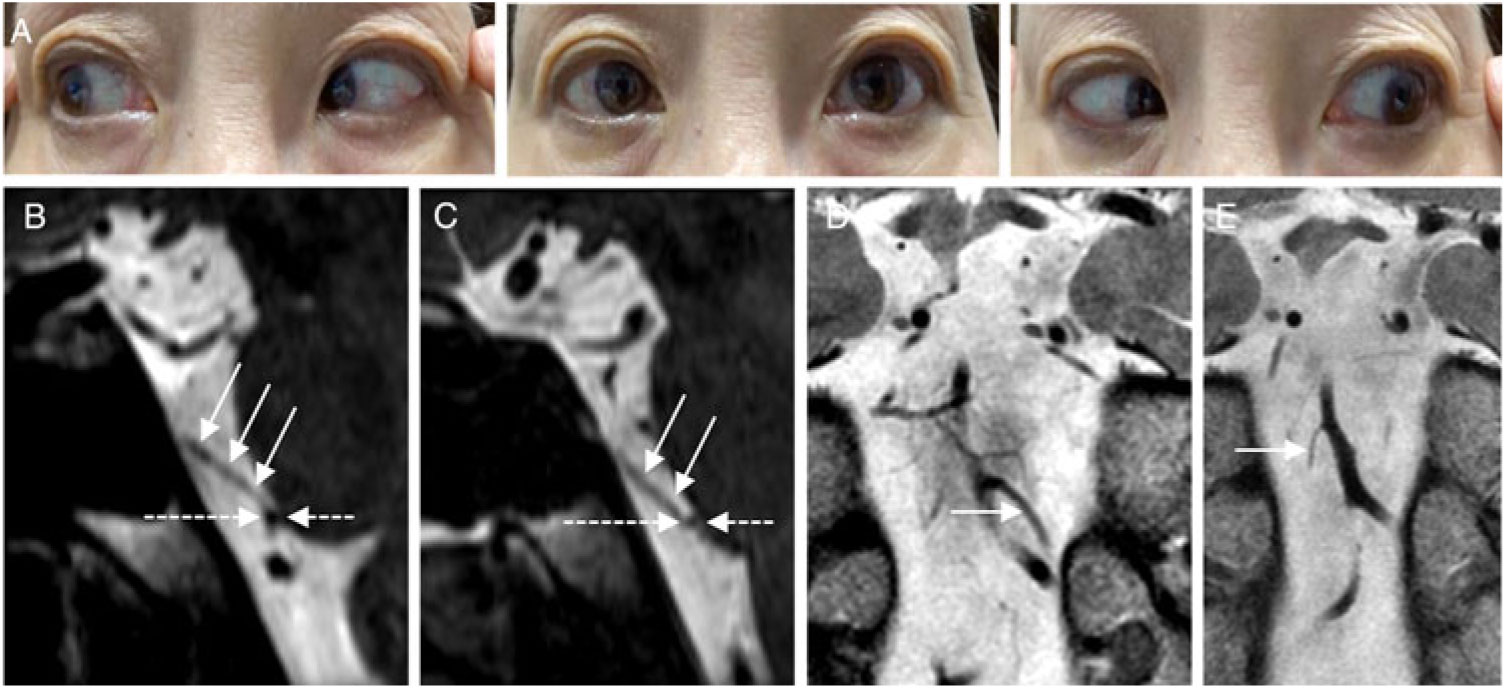
Figure 1: External photo demonstrating a limitation of abduction in the left eye (A). Sagittal-oblique reformat (B) of an axial three-dimensional T2-weighted sequence shows the left abducens nerve cisternal segment (solid arrows) in contact with the left anterior inferior cerebellar artery (AICA) (dotted arrow) at the nerve root entry zone. Sagittal-oblique reformat (C) of the same pulse sequence (C) shows the right abducens nerve (solid arrows) in contact with a much smaller right AICA (dotted arrow). Coronal T2-weighted sequence shows that the left AICA (D, arrow) is much larger than the right AICA (E, arrow).
Neurovascular compression is a well-recognized but rare cause of 6NP. Reference Tsai and Demer1 This may occur from aneurysms, Reference Er, Fraser and Lanzino2 dolichoectactic Reference Zhu, Thulborn, Curnyn and Goodwin3 or relatively normal-appearing vessels Reference Tsai and Demer1 in an aberrant location. This patient had a relative large AICA in contact with the left abducens nerve at the root entry zone, and the mechanism of the 6NP was likely related to mass effect and pulsatility on the abducens nerve in this location. There was also contact of the right AICA with the right abducens nerve, but the right AICA was a much smaller artery than the left AICA, and had no effect on the function of this nerve. The normal anatomic location of the AICA has been shown to be away from the root entry zone of the abducens nerve. Reference Delion, Dinomais and Mercier4 It is recognized that pathology occurs only when vessels are in contact with a cranial nerve at or proximal to the root entry zone, which is the transition zone between the central and peripheral myelin and an area that lacks perineurium and epineurium and is particularly vulnerable to continued pulsatile pressure. Reference Janetta5 , Reference Sandvand, Ringstad and Kerty6
Five previous cases of neurovascular compression of the AICA on the abducens nerve resulting in a 6NP have been described. Reference Sandvand, Ringstad and Kerty6 – Reference Taniguchi, Ii, Kobayashi, Maeda and Tomimoto10 The location of the compression was at the root entry zone in four cases, and the abducens nerve was sandwiched between a persistent trigeminal artery and the AICA in one case. Reference Nakamagoe, Mamada, Shiigai, Shimizu, Koganezawa and Tamaoka9 Every patient experienced spontaneous improvement, and four out of five cases had recurrent sixth nerve palsies and the number of episodes varied from 4 to 11. Reference Sandvand, Ringstad and Kerty6 – Reference Nakamagoe, Mamada, Shiigai, Shimizu, Koganezawa and Tamaoka9 The time to recovery varied from 2 to over 4 months. Reference Kato, Nakajima, Ohnaka, Ishihara and Kawamura7 , Reference Taniguchi, Ii, Kobayashi, Maeda and Tomimoto10 No neurosurgical treatment was pursued in any of the cases. This case demonstrates that neurovascular compression of the abducens nerve from the AICA can also have a chronic course.
Acknowledgments
None.
Disclosures
The authors have no conflicts of interest to disclose.
Statement of Authorship
Conception and design (JAM), data acquisition (BA, DMM, JAM), manuscript draft and preparation (BA, DMM), critical analysis (JAM, DMM), final approval (BA, DMM, JAM).



