The Ontario Coil Embolization Task Force, established by Critical Care Services Ontario as part of their program to support improved access to neurosurgical services in Ontario, was a time-limited entity providing advice to the Ministry of Health and Long-Term Care of Ontario. The aim was to describe the services available in Ontario for treating cerebral aneurysms and to ensure that the Province was equipped to meet current and future demand. Task Force membership was comprised of neurosurgeons, interventional neuroradiologists, administrative leaders from Local Health Integration Networks throughout Ontario, and Ministry representatives. The Task Force was co-chaired by Dr. Karel Terbrugge, neuroradiologist, and Dr. Stephen Lownie, neurosurgeon (a complete list of members is in Table 1).
Table 1: Ontario Coil Embolization TaskForce membership
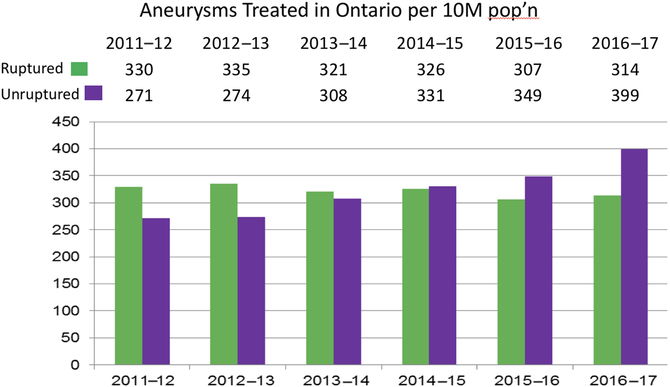
There are 15 neurosurgical centers in the province of Ontario (11 adult and 4 pediatric). During 2011–2017 the number of annual aneurysm ruptures remained stable at 314–330 per 10 million persons per year. On the other hand the number of unruptured aneurysms treated annually increased from 271 to 399 per 10 million. Data are summarized in Figure 1. The results indicate that coiling of unruptured aneurysms is being offered more frequently with each passing year.
Figure 1: Cerebral aneurysms treated in Ontario, per 10 million persons
A steady decline in the proportion of aneurysms treated by clipping versus coiling was observed. From the first 3 years of data collected there was a steady decline in the proportion of intracranial aneurysms treated by clipping. During 2011–2012, 35% of aneurysms were treated with clipping. By 2013–2014 this dropped to 26%. Of centers that performed clipping during 2013–2014 only 5 centers performed 20 or more. A few tertiary neurosurgery centers in Ontario provided almost no aneurysm clipping.
Task Force members developed a consensus of the factors in the decision to offer coiling treatment to individuals with an unruptured aneurysm. These include the presence of an aneurysm size 7 mm or greater in the anterior circulation (4 mm in the posterior circulation); the presence of an aneurysm of any size causing a cranial nerve palsy; or the presence of an aneurysm exhibiting growth on follow-up imaging. Relative factors include aneurysm shape, for example, lobulation; positive family history; and inability to treat the aneurysm surgically. In decision-making, there should be a division along the lines of asymptomatic aneurysms versus aneurysms presenting with cranial nerve palsy or headache. Relative contraindications include the presence of chronic or malignant disease associated with a reduced life expectancy of <5 or 5–10 years; the presence of a neurocognitive disorder; and patient age greater than 80 years.
Case costing analysis was done using 2012–2013 data from the five centers with mature coiling programs. Analysis was based on average case costs using Ontario Case Costing Initiative funding methodology; allocation methodology for fixed costs; length of stay ranges and averages; and average Health Inpatient Group (HIG) weights per hospital. The weighted average treatment cost for the surgical clipping of a ruptured aneurysm case was $76,664, while the cost for coiling was $72,481. The weighted average treatment cost for clipping an unruptured aneurysm was $19,121, whereas the cost for coiling was $23,729.
The Task Force recommended that certain requirements in clinical care be met by all hospitals offering coiling services to aneurysm patients. These included patient-level care considerations for ruptured and unruptured aneurysms; hospital service requirements including an active neurovascular program, resource and competency standards, and technology requirements including biplane digital subtraction angiography; and the establishment of multidisciplinary decision-making processes. It was recommended that all neurosurgical centers with coiling programs establish clinical criteria for coiling ruptured and unruptured intracranial aneurysms consistent with the Task Force report. All neurosurgical centers with coiling programs should participate in hospital- and provincial-level performance management initiatives, including reporting and analysis of coiling and clipping case information, monitoring outcomes on performance indicators, and taking action to improve quality measures at hospital and system levels. Hospitals providing coil embolization services should also maintain neurosurgical aneurysm clipping programs. It was recommended that smaller volume coiling centers, particularly in remote areas of the province, partner with existing Ontario neurovascular teaching centers to help mentorship of designated clinicians, as well as fulfillment of the program’s human resource, technology, and patient care outcome requirements. Existing neurovascular teaching centers with established postgraduate training programs would require special consideration with the aim to preserve trainee case volumes to ensure excellent aneurysm care for future generations.
The findings of the Ontario Coil Embolization Task Force will help to inform aneurysm care now and in the future.



The Ontario Coil Embolization Task Force, established by Critical Care Services Ontario as part of their program to support improved access to neurosurgical services in Ontario, was a time-limited entity providing advice to the Ministry of Health and Long-Term Care of Ontario. The aim was to describe the services available in Ontario for treating cerebral aneurysms and to ensure that the Province was equipped to meet current and future demand. Task Force membership was comprised of neurosurgeons, interventional neuroradiologists, administrative leaders from Local Health Integration Networks throughout Ontario, and Ministry representatives. The Task Force was co-chaired by Dr. Karel Terbrugge, neuroradiologist, and Dr. Stephen Lownie, neurosurgeon (a complete list of members is in Table 1).
Table 1: Ontario Coil Embolization TaskForce membership
There are 15 neurosurgical centers in the province of Ontario (11 adult and 4 pediatric). During 2011–2017 the number of annual aneurysm ruptures remained stable at 314–330 per 10 million persons per year. On the other hand the number of unruptured aneurysms treated annually increased from 271 to 399 per 10 million. Data are summarized in Figure 1. The results indicate that coiling of unruptured aneurysms is being offered more frequently with each passing year.
Figure 1: Cerebral aneurysms treated in Ontario, per 10 million persons
A steady decline in the proportion of aneurysms treated by clipping versus coiling was observed. From the first 3 years of data collected there was a steady decline in the proportion of intracranial aneurysms treated by clipping. During 2011–2012, 35% of aneurysms were treated with clipping. By 2013–2014 this dropped to 26%. Of centers that performed clipping during 2013–2014 only 5 centers performed 20 or more. A few tertiary neurosurgery centers in Ontario provided almost no aneurysm clipping.
Task Force members developed a consensus of the factors in the decision to offer coiling treatment to individuals with an unruptured aneurysm. These include the presence of an aneurysm size 7 mm or greater in the anterior circulation (4 mm in the posterior circulation); the presence of an aneurysm of any size causing a cranial nerve palsy; or the presence of an aneurysm exhibiting growth on follow-up imaging. Relative factors include aneurysm shape, for example, lobulation; positive family history; and inability to treat the aneurysm surgically. In decision-making, there should be a division along the lines of asymptomatic aneurysms versus aneurysms presenting with cranial nerve palsy or headache. Relative contraindications include the presence of chronic or malignant disease associated with a reduced life expectancy of <5 or 5–10 years; the presence of a neurocognitive disorder; and patient age greater than 80 years.
Case costing analysis was done using 2012–2013 data from the five centers with mature coiling programs. Analysis was based on average case costs using Ontario Case Costing Initiative funding methodology; allocation methodology for fixed costs; length of stay ranges and averages; and average Health Inpatient Group (HIG) weights per hospital. The weighted average treatment cost for the surgical clipping of a ruptured aneurysm case was $76,664, while the cost for coiling was $72,481. The weighted average treatment cost for clipping an unruptured aneurysm was $19,121, whereas the cost for coiling was $23,729.
The Task Force recommended that certain requirements in clinical care be met by all hospitals offering coiling services to aneurysm patients. These included patient-level care considerations for ruptured and unruptured aneurysms; hospital service requirements including an active neurovascular program, resource and competency standards, and technology requirements including biplane digital subtraction angiography; and the establishment of multidisciplinary decision-making processes. It was recommended that all neurosurgical centers with coiling programs establish clinical criteria for coiling ruptured and unruptured intracranial aneurysms consistent with the Task Force report. All neurosurgical centers with coiling programs should participate in hospital- and provincial-level performance management initiatives, including reporting and analysis of coiling and clipping case information, monitoring outcomes on performance indicators, and taking action to improve quality measures at hospital and system levels. Hospitals providing coil embolization services should also maintain neurosurgical aneurysm clipping programs. It was recommended that smaller volume coiling centers, particularly in remote areas of the province, partner with existing Ontario neurovascular teaching centers to help mentorship of designated clinicians, as well as fulfillment of the program’s human resource, technology, and patient care outcome requirements. Existing neurovascular teaching centers with established postgraduate training programs would require special consideration with the aim to preserve trainee case volumes to ensure excellent aneurysm care for future generations.
The findings of the Ontario Coil Embolization Task Force will help to inform aneurysm care now and in the future.
Disclosures
The authors have no conflicts of interest to declare.
Statement of Authorship
Primary author: SPL. Manuscript review and approval: KGT, BL, SPL.