Bell’s palsy is the most common cause of facial mononeuropathy and the main etiology is most likely reactivation of latent herpes viral infections, including herpes simplex virus 1 (HSV-1), in the geniculate ganglia.Reference Zandian, Osiro and Hudson 1 Herpes simplex virus 1 is the most common cause of sporadic infectious encephalitis; however, it is unclear whether this is caused by reactivation of latent virus or by primary infection.Reference Bradshaw and Venkatesan 2 The mechanism of CNS entry is also unclear, and theories include both retrograde transport through cranial nerves or hematogenous dissemination.Reference Bradshaw and Venkatesan 2 To our knowledge, no case of idiopathic facial neuropathy temporally associated with HSV encephalitis has been published. We report a case of Bell’s palsy followed 7 weeks later by PCR-confirmed HSV encephalitis.
A 73-year-old woman with a history of chronic kidney disease, hypertension, and dyslipidemia, developed complete left-sided facial weakness within a few hours. Her Family Physician prescribed a 7-day course of oral famciclovir and prednisone for a diagnosis of Bell’s palsy. Her facial weakness improved and was at baseline 4 weeks later. She did not have a previous history of cold sores or genital herpes.
Approximately 7 weeks after the onset of facial weakness she was brought to the Emergency Department following two episodes of vomiting. Her family had noticed progressive somnolence, generalized weakness, and confusion over the preceding 4 weeks. On assessment, she was afebrile, not oriented to date and minimally communicative. Initial investigations for delirium including bloodwork and CT head were within normal limits. Overnight, she became febrile with increased drowsiness. A clinical diagnosis of meningoencephalitis was made and empiric IV acyclovir, ceftriaxone, vancomycin, and ampicillin were started. Initial lumbar puncture was unsuccessful. While undergoing repeat lumbar puncture on post-admission day 2 she became obtunded requiring intubation and admission to the intensive care unit.
Subsequent MRI demonstrated cortical expansion and abnormal signal intensity of the left anterior temporal lobe and hippocampus (Figure 1). CSF analysis demonstrated 75×106/L neutrophils, 17×106/L lymphocytes, and 8×106/L monocytes; 16,550×106/L red cells; 6.0 mmol/L glucose; and 1.24 g/L protein. Bacterial gram stain and culture of CSF were negative. PCR of CSF was positive for HSV DNA. On the basis of clinical history and these findings she was diagnosed with HSV encephalitis and continued on IV acyclovir 10 mg/kg/dose q8 hours. All antibiotics were discontinued. Other infectious work up including HIV, Hepatitis B&C, and bacterial cultures were negative.
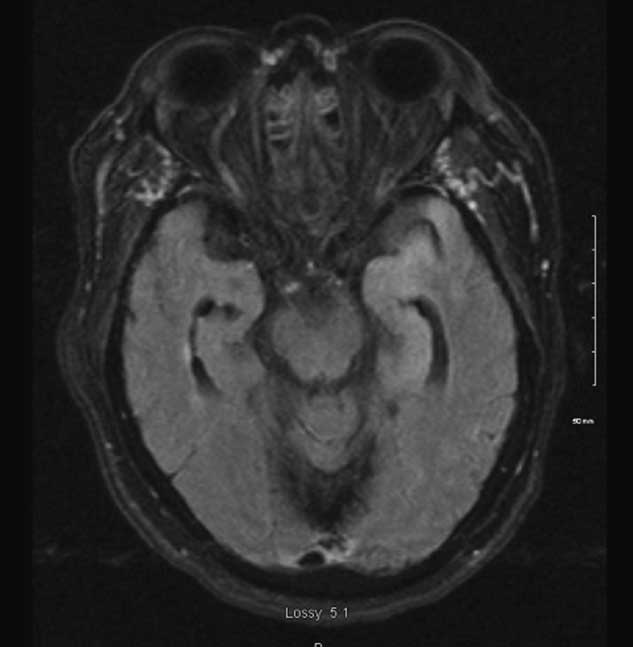
Figure 1 MRI demonstrating mild cortical expansion and increased T2/FLAIR signal intensity of the left anterior temporal lobe and hippocampus.
The patient had a slow neurological recovery with prolonged intubation requiring tracheostomy. Six weeks after admission she was found to be in asystole and died after unsuccessful resuscitation. Autopsy was not performed.
In this report, we document a case of Bell’s palsy treated with a 7-day course of famciclovir and prednisone followed by PCR-confirmed HSV encephalitis in close temporal proximity. Though she was diagnosed with encephalitis 7 weeks after the onset of facial nerve palsy, she had progressive symptoms of somnolence, generalized weakness, and confusion for 4 weeks before this diagnosis.
The etiology of Bell’s palsy has been debated, but current evidence supports reactivation of latent herpes viral infections, primarily HSV-1, in the geniculate ganglia with subsequent facial nerve involvement.Reference Zandian, Osiro and Hudson 1 , Reference Murakami, Mizobuchi, Nakashiro, Doi, Hato and Yanagihara 3 , Reference Schirm and Mulkens 4 The current recommended management includes a course of corticosteroids with or without an antiviral agent.Reference Zandian, Osiro and Hudson 1 , Reference Numthavaj, Thakkinstian, Dejthevaporn and Attia 5
The etiology of HSV encephalitis is less clear. The most likely mechanisms of CNS entry include retrograde transport through the trigeminal or olfactory nerves, or hematogenous dissemination, though the latter is less likely given consistent involvement of orbitofrontal and mesiotemporal lobes.Reference Bradshaw and Venkatesan 2 There is evidence supporting both primary infection and reactivation of latent virus. The reactivation may occur in the cranial nerves as described or within the brain parenchyma itself.Reference Bradshaw and Venkatesan 2 , Reference Steiner 6 IV acyclovir has been the first-line treatment since the mid-1980s.Reference Bradshaw and Venkatesan 2
It was not possible to prove that our patient’s Bell’s palsy was caused by HSV, the same virus that caused her encephalitis. However, these events seemed temporally related and unlikely to be coincidence. Given that the facial weakness and MRI findings were ipsilateral, our proposed mechanism of viral dissemination is retrograde transport through facial neurons gaining access to the CNS. Hematogenous spread is felt to be less likely. It is unlikely that her facial neuropathy was the first sign of primary CNS infection as there were no other symptoms at onset of facial weakness, she remained well for several weeks, and there were no signs of brainstem involvement on MRI. Further study is needed to clarify the relationship between Bell’s palsy and HSV encephalitis, including possible influence of early antiviral medication use.
Disclosure Information
Margaret Moores and Caroline Nott have nothing to disclose.
Statement of Authorship
Literature review, primary manuscript: MM. Literature review, critical revision of manuscript for intellectual content: CN.



