Introduction
The Canadian health care system is publicly funded and designed to provide all Canadian residents with reasonable access to medically necessary hospital and physician services without paying out-of-pocket. The Federal government sets and administers the national standards for the health care system through the Canada Health Act. Funds obtained by the Federal government (tax dollars) are transferred to each of the provinces and territories if they fulfill the standards set out in the Canada Health Act. These standards include public administration, comprehensiveness, universality, portability and accessibility. The individual provinces and territories are then responsible for the management, organization and delivery of health care services for their residents.
As each of the ten provinces and three territories manage their own provision of health care for their residents, there is a real possibility of differences between regions in access to health care. The standards outlined in the Canada Health Act, however, require accessibility—all residents must have reasonable access to medically necessary services. What is “reasonable access” and “medically necessary” is not defined and typically relies on a dialog between the government, respective medical colleges and the relevant patient advocacy groups.
The mission of the Canadian Neuromodulation Society is “to promote education and access to neuromodulation therapies across Canada.” To lobby for reasonable access to these therapies, we need to know what is the current access to neuromodulation across the entire country. Once this is known, we can then determine whether regions within Canada are underserved and direct our attention to remedying these local inequities. This study quantifies the rate of deep brain stimulation (DBS) for the entire country of Canada. Analyses were then performed to determine whether there were significant differences in access based on provincial or territorial location, rural or non-rural location or socioeconomic status.
Methods
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors. Ethical approval for this study was obtained through the Clinical Research Ethics Board at the University of British Columbia (H17-00362). A 2-year retrospective review of patients receiving DBS electrodes in all Canadian neurosurgical centers was conducted from January 1, 2015 to December 31, 2016. Patients receiving DBS in research trials were not included. The forward sortation area (FSA) postal code information and age at implantation were obtained from the only two companies licenced to provide DBS electrodes in Canada: Boston Scientific and Medtronic. The study protocol was reviewed and approved by both companies to ensure patient anonymity. No data were provided on gender, diagnosis, wait time for surgery, implantation hospital or surgeon, electrode target or clinical outcome. Patients receiving implantable neural stimulators (INS) but no intracranial electrodes (leads) were not included as they were assumed to be patients who already had DBS in place and were just receiving a “battery replacement.” Patients with the same FSA and age at implantation were considered duplicates (i.e., DBS performed as a staged procedure or a revision). Patients receiving implants funded by research grants were not included. Our data were cross-referenced with Statistics Canada National Census information according to FSA. The province or territory of residence, rural or non-rural (urban) designation, pre-tax total median household income and per capita rate of DBS were determined. 1 , 2
Canadian DBS Location Map
The Google Maps Application Program Interface (Santa Clara, California) was used to transfer the 722 FSA data points into longitude and latitude parameters for subsequent generation of a population density map. The midpoint of each FSA was used as a geographic estimate of patient location. This map was developed using an open-source software called Open Heat Map.
Provincial and Territorial DBS Rate Comparison
The population utilizing DBS surgery is known to be older, and therefore regions with older patients would be expected to have more DBS than those with a similar sized but younger population. To account for this effect, age-standardized rates (with 95% confidence intervals) were calculated for each province using the following age groups at the time of implantation: 0-39, 40-59, 60-69 and 70-90 inclusive. The 2016 Canada census population was used as the standard population for these calculations. 3 Standardized rate ratios (provincial rate/Canada rate) along with the 95% confidence interval on the standardized rate ratios were used to determine whether or not a provincial rate was significantly different from the national rate (i.e., whether or not the 95% confidence interval on the standardized rate ratio for each province excluded 1). To avoid the effect of comparing heavily populated provinces with the rate for Canada (which is itself affected by their contribution), the rate for each province was also compared with the rate in the rest of Canada (e.g., Ontario with Canada minus Ontario). These standardization steps facilitated assessment of statistical differences in age-standardized rates between provinces and territories relative to the overall rates observed across Canada. From the total cohort, 680 patients had age of implantation information and were therefore used in this analysis.
Rural and Non-Rural Access
The 2011 National Census of Population provided by Statistics Canada is the most recent assessment of rural and non-rural-dwelling proportions across provinces and territories. 4 A rural area is defined as a small town or village with less than 1000 people, agricultural land, or a remote wilderness area. A non-rural area, which used to be called an urban area before the 2011 National Census, is essentially everywhere else. The proportion of rural-dwelling individuals within our cohort was determined using FSA information. These data were then compared with provincial and territorial proportions documented by Statistics Canada using the one-sample test for proportions. The level of statistical significance was set at p<0.005 to correct for multiple comparisons. This analysis was repeated for the overall Canadian cohort (n=722) and compared with the Canadian rural proportion.
Median Household Income Analysis
Information provided by Statistics Canada for the 2015 Canadian Economic Census (embedded in the 2016 Census Report) was used to determine the median before-tax household incomes for each FSA. 5 For each province, the mean median income for the study cohort was compared with their respective mean provincial median incomes using a one-sample t-test. The level of statistical significance was set at p<0.005 to correct for multiple comparisons. This analysis was repeated for the overall Canadian cohort (n=722) and compared with national before-tax median household income data.
Results
This 2-year, retrospective review captured 728 patients receiving DBS implantation across Canada. Cases with missing FSA information were excluded (n=6), leaving 722 patients for analysis. The home location (provided by the FSA) for each of these patients is shown in Figure 1. No patient with a residence in the three territories (Yukon, Northwest Territories or Nunavut) was treated.
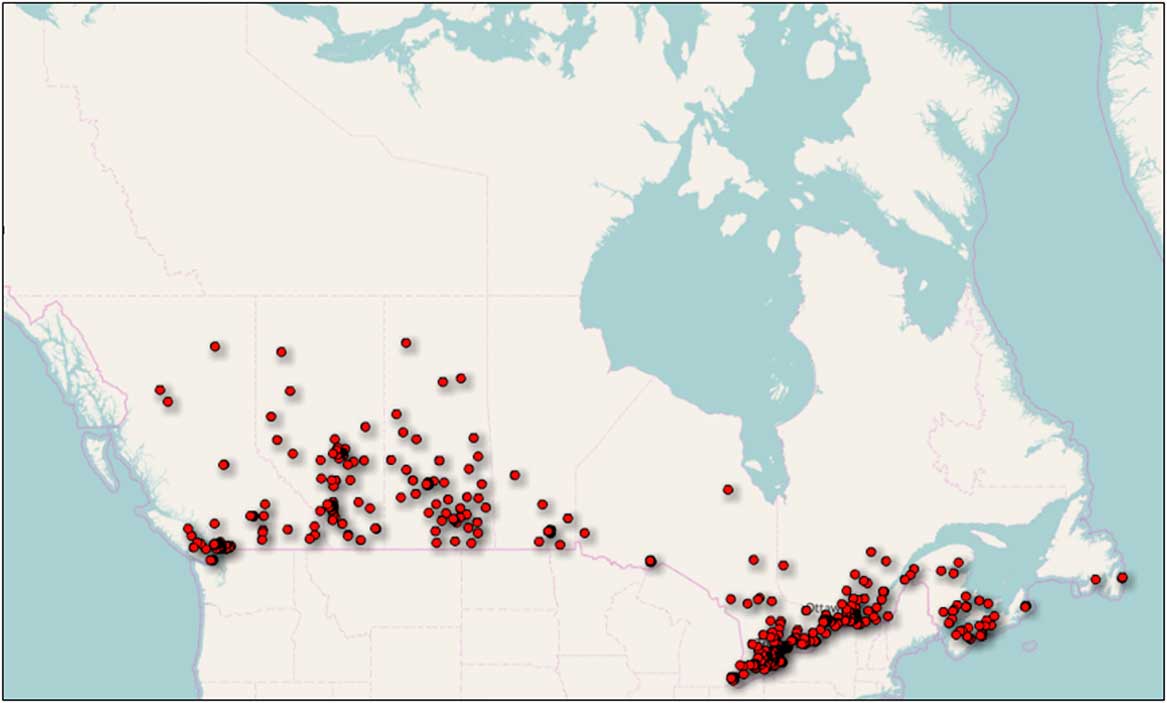
Figure 1 Geographical distribution of patients treated with deep brain stimulation (DBS) in Canada. The location of each patient receiving DBS is represented by a red dot. The dots were placed at the midpoint of their home forward sortation area. Dots are overlapped for multiple entries. No patients were treated in the three Northern Territories.
The age at implantation was available for 692 patients. The distribution of age at surgery is shown in Figure 2 and was skewed toward older patients. The median age at treatment was 61.5 years. Surgery for patients older than 80 years was rarely performed. Using the population of the country at that time, we calculated the rate of DBS surgery in Canada to be 10 per 1,000,000 per year.
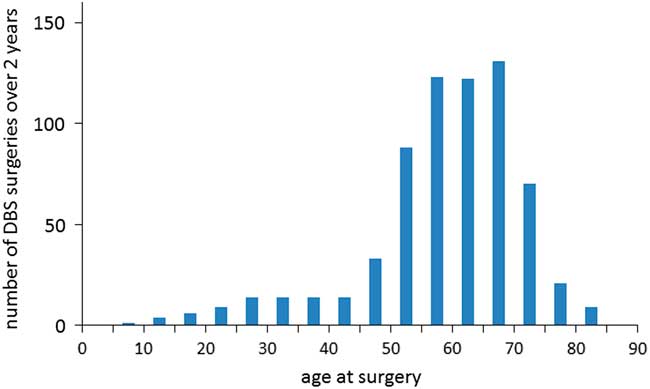
Figure 2 Distribution of age at surgery. The number of patients receiving deep brain stimulation (DBS) in Canada over a 2-year epoch is shown for each 5-year age group. There appears to be a bimodal distribution with peaks around 30-35 and 60-65 years of age (perhaps corresponding to patients with dystonia and Parkinson’s disease).
The number of cases performed within each province is provided in Table 1 along with data on provincial population, rate of surgery compared with the national average, rural proportion, proportion of DBS recipients from rural areas, mean of the median household incomes for the entire province and for the regions within each province where patients received DBS. The provincial rate of DBS surgery was age adjusted and then divided by the national average (i.e., the provincial standardized rate ratio) and shown in Figure 3 along with 95% confidence intervals. The rate of DBS surgery was significantly higher than the national average in Saskatchewan (374%) and significantly below the national average in Quebec (40%) and Newfoundland & Labrador (32%). The results were similar when each province was compared with the national average calculated without that province (i.e., the rate in Ontario divided by the average rate in all provinces and territories except Ontario) and were therefore not shown.

Figure 3 Rate of deep brain stimulation (DBS) surgery in each province compared with the national rate. The age-adjusted rate of DBS for each province was divided by the national average and displayed with 95% confidence intervals. Provincial standardized rate ratios that did not include 1.0 (national average) were statistically different from the national average. AB=Alberta; BC=British Columbia; MB=Manitoba; NB=New Brunswick; NF=Newfoundland & Labrador; NS=Nova Scotia; ON=Ontario; PE=Prince Edward island; QC=Quebec; SK=Saskatchewan.
Table 1 Demographics of deep brain stimulation (DBS) surgery in Canada
AB=Alberta; BC=British Columbia; MB=Manitoba; NB=New Brunswick; NL=Newfoundland and Labrador; NS=Nova Scotia; NT=Northwest Territories; NU=Nunavut; ON=Ontario; PE=Prince Edward island; QC=Quebec; SK=Saskatchewan; YK=Yukon.
The population in millions, number of DBS cases over the 2-year study and rate of DBS surgery divided by the national average (×100) is presented for each Province and Territory.
*=95% confidence interval on standardized rate ratio excludes 1. Within each Province, the percentage of rural population and median pre-tax household income was not significantly different for patients receiving DBS and the entire Provincial population. For the entire country, patients receiving DBS had significantly higher median income.
**≤0.0001.
Within each province, the percentage of patients receiving DBS who lived in a rural area was calculated and compared with the percentage of all people living in a rural area within that province (see Table 1). There was no significant difference between the percentage of patients receiving DBS from rural areas compared with the percentage of the entire provincial population living in rural areas.
The 2016 Canadian Census data provided the pre-tax median household income for each FSA (see Table 1). There was a significant difference (p<0.0001) between the mean of the median household incomes from regions where patients received DBS ($CDN 78,000) and for all Canadians ($CDN 70,000). Similar analyses were performed for each province. The level of statistical significance was set at p<0.005 because ten separate analyses were performed (one for each province). There was no significant difference within any province between the mean of the median household incomes of patients receiving DBS and the entire provincial population.
Discussion
This is the first study to document the rate of DBS surgery for an entire country. During this 2-year study, no patients living in the three Northern Territories received DBS surgery. Although this apparent lack of access to DBS in the Canadian North is strikingly obvious in Figure 1, the small and relatively young population of that region may explain why no one received DBS. The combined population of the Yukon, Northwest Territories and Nunavut is ~100,000 people. Using the national rate of 10 cases per 1,000,000 per year, one might expect only two cases during the study. This estimate should be further reduced because the percentage of people older than 65 years (the age group most likely to receive DBS) in the three territories is only 8% compared with the national average of 17%.
The rate of DBS surgery in Saskatchewan was significantly higher (374%) than the national average. This province has three neurosurgeons performing DBS for 1,098,352 people, which is the highest ratio of neurosurgeons implanting DBS to provincial population (1 per 0.37 million) in Canada. All other provinces have ratios at least five times lower (range: 1 per 2.0-4.6 million). During the study, some patients from Manitoba were also receiving DBS in Saskatchewan because the local neurosurgeon had just retired. Using the combined population of both provinces, the ratio is still more than twice any other province at 1 per 0.8 million. Saskatchewan has dedicated operating room time for DBS and no budgetary restrictions in the number of cases implanted per year. All the other provinces (except Nova Scotia) have some sort of cap on the annual amount of funding available for DBS procedures. Follow-up of patients in Saskatchewan for programming and troubleshooting is facilitated by the use of remote presence robotic technology where patients can be reviewed in their home communities.Reference Mendez, Song, Chiasson and Bustamante 6
The decision to limit DBS funding is beyond the scope of this paper, but numerous studies have shown that DBS provides long-term financial savings for society.Reference Dams, Siebert and Bornschein 7 - Reference Eggington, Valldeoriola, Chaudhuri, Ashkan, Annoni and Deuschl 9 The upfront costs of surgery and implants are more than offset by the long-term savings when (i) a patient returns to work from disability; (ii) a patient becomes safely independent at home, allowing their spouse to return to work; (iii) a patient uses less medications and emergency visits; or (iv) a patient is delayed from entering a nursing home. Unfortunately, our government system is such that the Ministry paying for the surgery (Ministry of Health) is separate and siloed from the Ministry receiving the benefits (Ministry of Finance).
The rate of DBS surgery in Quebec was significantly lower (40%) than the national average. This province has four neurosurgeons performing DBS for 8,160,000 people. Their budget for DBS implants has seriously constrained the number of new cases being performed because an increasing portion of their fixed budget is used for “replacements.” These are INS for patients who already have a DBS system in place but need a new INS because the battery has exhausted. Our study only looked at new cases of DBS and would not have included this growing cohort of patients who require a replacement INS for continued therapy. In an earlier study authored by the team from McGill University in Montréal, resource allocation was identified as a key factor limiting access to care.Reference Bell, Maxwell, McAndrews, Sadikot and Racine 10 Other possible causes for reduced access to DBS surgery in Quebec may include patient preferences, reduced referral rates from neurologists or neuropsychologists, limited resources for multidisciplinary team pre-operative evaluations or inadequate operating room time.
The rate of surgery in Newfoundland & Labrador was also significantly lower (32%) than the national average. Its small population (519,715 people), however, means that small fluctuations in the number of patients receiving surgery could have a large effect. In fact, if two more patients had undergone surgery during the study, the provincial rate would have decreased within the 95% confidence interval of the national average. There are no facilities for DBS surgery in that province but all patients in the Maritime Provinces (New Brunswick, Newfoundland & Labrador, Nova Scotia and Prince Edward island) are treated centrally in Halifax, Nova Scotia. Taken as a whole, the Maritime Provinces do not have reduced access to DBS surgery.
There was no suggestion in our data that patients living in rural areas had significantly less access to DBS than those living in urban areas. The socioeconomic data for the entire country suggested that patients receiving DBS surgery came from regions with a significantly higher median household income than the average for the entire country. The analyses within each province, however, showed no significant difference in access to DBS based on socioeconomic status. The difference across the entire country is likely to reflect the differences in incomes between the provinces (Table 1). Ontario and Alberta have median household incomes above the national average, and therefore DBS patients coming from those provinces would tend to come from regions with a median household income higher than the national average. As a large portion of patients came from those two provinces (n=432, 60% of all patients), the data suggested that patients getting DBS came from more wealthy areas than the average Canadian. There was a trend within Ontario and Alberta toward DBS patients coming from wealthier regions, but this did not withstand a Bonferroni correction for multiple analyses. In the two provinces with significantly reduced access to DBS surgery (Quebec and Newfoundland & Labrador), there was no suggestion that access was biased toward wealthy regions. Our data do not directly reflect the income of the individual patient but rather infers their socioeconomic level based on the average of all individuals living within their FSA region (typically 20,000-40,000 people).
Studies from the United States have reported significant disparities in race and socioeconomic status among patients accessing DBS surgery.Reference Willis, Schootman, Kung, Wang, Perlmutter and Racette 11 , Reference Lad, Kalanithi and Patil 12 Black and Asian Medicare beneficiaries were significantly less likely to receive DBS than White beneficiaries, and high neighborhood socioeconomic status was associated with a 1.4-fold-higher odds of receiving DBS. DBS utilization over a 14-year period from the Nationwide Inpatient Sample data base (representing ~20% of non-federal hospitals in the United States) was reported to show that the age at surgery was skewed toward older patients.Reference Chan, McGovern and Brown 13 This was similar to our results. Women also had lower odds of receiving DBS compared with men. This trend for a gender bias has also been reported beforeReference Setiawan, Kraft and Doig 14 , Reference Hariz, Nakajima and Limousin 15 but could not be studied with our anonymized data. Some studies have reported that the socioeconomic status of the patient also has an impact on their surgical outcome,Reference Genc, Abboud and Oravivattanakul 16 but the outcome of our patients could not be evaluated with our anonymized data.
This study highlighted the current rate of DBS across Canada and did not discuss whether this is an appropriate level of access to this care. No other study has documented the rate of DBS in another country, but estimates are available. The annual rate of DBS surgery in Australia was estimated to be 13-15 cases per million in 2013.Reference Poortvliet, Silburn, Coyne and Chenery 17 The rate in Switzerland was estimated to be approximately ten cases per million in 2012.Reference Christen and Muller 18 The rate in Korea was estimated to be approximately three cases per million in 2015.Reference Lee 19 The rate in the United States was estimated to be approximately eight cases per million per year.Reference Pilitsis, Burrows, Paters, Sargent, Ng and Tseng 20
Limitations
The Canada Study is limited by the resolution of the data presented. The data only followed a 2-year epoch, and thus local, temporary fluctuations due to staffing issues would have more influence than if the data had been collected over a decade. By using FSA postal code designations, the anonymity of patients is protected at the cost of gaining more insight into the race, gender and socioeconomic status of patients accessing DBS services. Furthermore, we cannot determine the indications for DBS, the outcomes of surgery or the distance a patient had to travel to receive surgery. Our data would not capture patients leaving Canada to get their DBS in other countries (e.g., United States or China). Any two patients with the same FSA and age were considered duplicates (i.e., a staged procedure), but it is possible that they were two different people. The retrospective study was also limited by incomplete data sets.
Conclusion
This is the first study to quantify the rate of DBS surgery for an entire country. This rate of 10 DBS cases per 1,000,000 people per year is likely to represent the current “reasonable access” for this therapy within Canada. The Canadian Neuromodulation Society will now be able to use this standard to ensure that all Canadians have reasonable access to this medically necessary therapy “from Coast to Coast to Coast.” This rate can also be compared with other countries once this information becomes available. It did not appear that access to DBS surgery in Canada was limited by socioeconomic status. This is in keeping with the Canada Health Act, which requires reasonable access to medically necessary therapies based on medical need not ability to pay. Finally, it is important to recognize that this current standard is not static. The increasing incidence of diseases currently requiring DBS coupled with the expanding indications for this surgery will mean more patients will need access to this medically necessary therapy in the future.
Acknowledgment
This study was presented in part at the 10th annual meeting of the Canadian Neuromodulation Society, February 5, 2018.
Disclosures
CMH, AKM, MST and IM have nothing to disclose. MP and CRH have received research grants and speaking honoraria from Boston Scientific, Medtronic and St. Jude’s Medical (now Abbott). MP and CRH report grants and personal fees from Boston Scientific, grants and personal fees from Medtronic and grants and personal fees from Abbott (formerly St. Judes Medical), outside the submitted work.
Statement of Authorship
The corresponding author (CMH) was responsible for the idea of the study, collecting the data and writing the manuscript; AKM helped collect and present the data; MSK was responsible for statistical analysis; IM and MP were responsible for discussions about their respective provinces and for reviewing the manuscript; and CRH was responsible for reviewing the manuscript and the requested revisions.






