Indirect traumatic optic neuropathy (ITON) is a rare but important cause of vision loss in head trauma. Although optic nerve head pallor develops over time as the nerve atrophies, it can sometimes be difficult to identify clinically in the acute period given the associated normal appearance of the visual system. Magnetic resonance imaging (MRI) is often delayed to capture late optic atrophy and confirm the diagnosis, but literature on the acute MR appearance in ITON is scarce. Here, we describe the clinical findings and acute neuroradiographic appearance in a patient with profound vision loss from ITON.
A 64-year-old gentleman tripped while working on his acreage, sustaining a ground-level fall and striking his face squarely against a box. He did not lose consciousness but sustained a scalp laceration that was sutured by the emergency department. However, he stated that his vision rapidly but painlessly “darkened” in his left eye following the incident. Past medical history included prostate cancer on active brachytherapy, right retinal detachment status post-pneumatic retinopexy, and bilateral cataract surgery.
On examination, his Snellen visual acuity was 20/25 in the right eye and light perception in the left eye. Intraocular pressures were 14 and 13 mmHg. There was a grade III left afferent pupillary defect. On slit-lamp examination, the anterior segment exam was unremarkable apart from left subconjunctival hemorrhage. Both optic nerves appeared normal with a cup-to-disc ratio of 0.4 and no disc hemorrhages, edema, pallor, or elevation. The macula was flat in both eyes; there were areas of previous laser retinopexy peripherally in the right eye. Extraocular movements were full and intact. There was no proptosis.
On unenhanced CT of the brain and orbits, no bony impingement of the left optic nerve was seen. No fractures were detected in the orbital bones, and no blood was seen in the orbit or optic canal (Figure 1A-B).
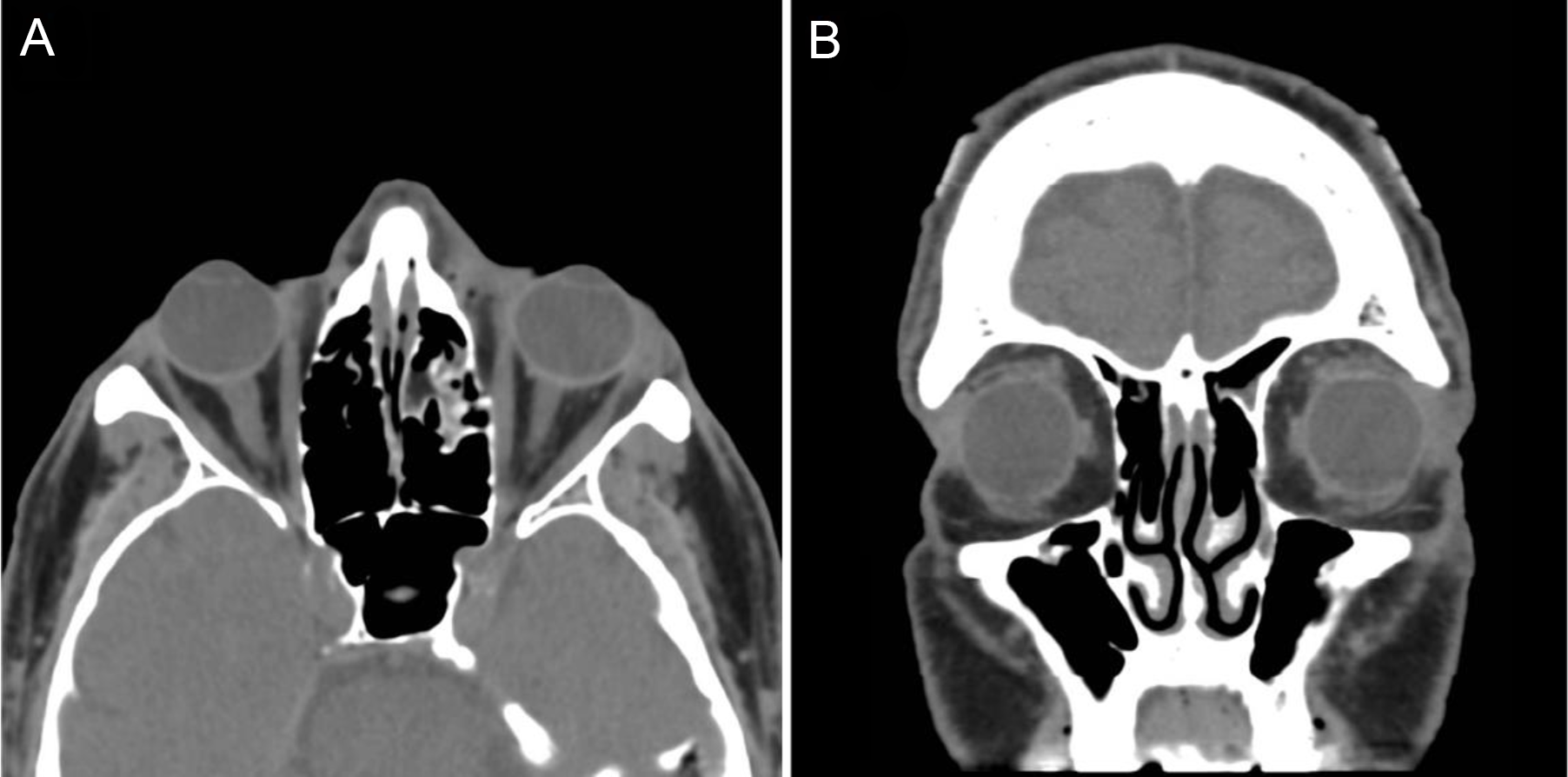
Figure 1: CT Orbits - (A) Axial view (B) Coronal view. Unremarkable appearance aside from mild periorbital edema at left; nerves are normal-appearing bilaterally, and there is no compromise of the optic canal.
MRI of the brain and orbits was performed 3 days following the injury. This revealed a segment of enhancing left prechiasmatic optic nerve injury on T1-GAD sequences (Figure 2A-B) and corresponding increased signal intensity on T2 FLAIR and STIR imaging (Figure 2C-D). In addition, there were nonspecific foci of increased FLAIR signal intensity in the splenium of the corpus callosum on the left and in the right periventricular white matter. Given the patient history, these were suspected to signify foci of traumatic brain injury secondary to rotational shear injury, but are nonspecific.
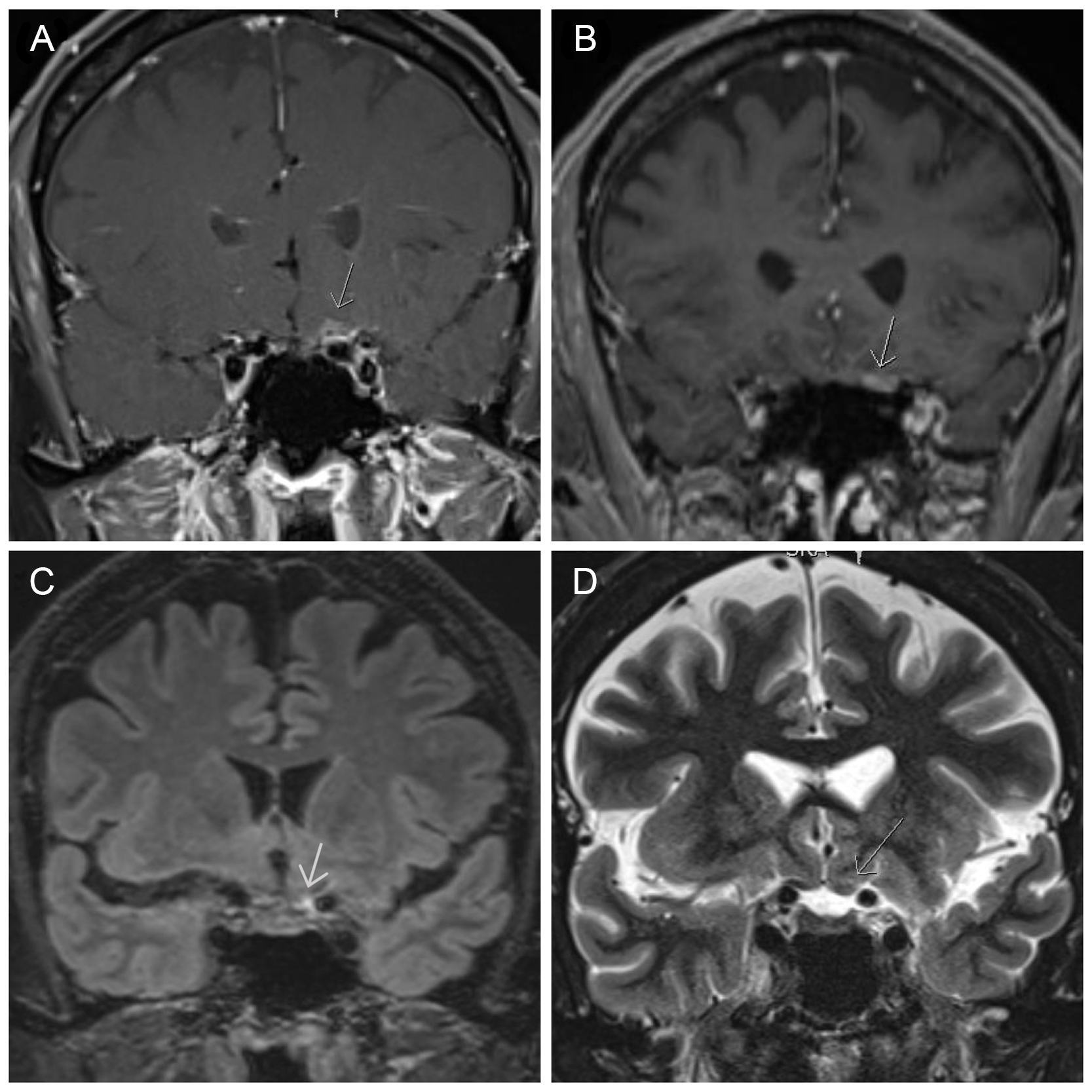
Figure 2: MR Orbits/Brain. Coronal gadolinium-enhanced T1-fat saturated sequences reveal enhancement of the left prechiasmatic optic nerve (A: T1 DIXON, B: T1 VIBE). Increased signal is seen on coronal T2 FLAIR (C) and subtly on STIR (D) sequences in the same distribution (Arrows).
We discussed the poor visual prognosis with the patient: he declined a trial of steroids, was referred to neurology for assessment of his brain injury, and returned to follow-up with his regular ophthalmologist.
Traumatic optic neuropathy (TON) is a form of optic nerve injury rarely seen following head trauma and is divided into two subtypes. Direct traumatic optic neuropathy (DTON) is characterized by axonal damage or vascular compromise from transection by bony fragments or penetrative trauma, mechanical strain (such as in optic nerve avulsion), or compression. ITON is characterized by vision loss following percussive closed-head injury, most commonly from trauma to the forehead, brow, or scalp. ITON is more common than DTON, but its pathophysiology remains poorly understood. It is hypothesized that this injury is likely multifactorial. The delicate blood supply to the intracanalicular optic nerve is likely compromised in inertial trauma, resulting in microinfarction, and diffuse axonal damage from biomechanical stress is thought to contribute as well. Secondary edema may lead to compartment syndrome within the nerve, furthering ischemic and compressive injury. Reference Singman, Daphalapurkar and White1
The diagnosis of indirect TON can be challenging, as the fundus (as in our case) may well appear completely normal at initial assessment in the acute phase. The presence of a relative afferent pupillary defect is an important clinical feature and may be accompanied by decreased visual acuity, color vision loss, and variable field defects. Later in the course of the disease, optic atrophy and pallor may develop. Reference Singman, Daphalapurkar and White1
Neuroimaging is an indispensable tool for the diagnosis and management of TON. CT is an excellent way to assess the anatomy of the orbit and optic canal and identify many of the hallmarks of DTON. It is, however, expected to appear normal in the acute phase of ITON. Although seldom performed in most centers, early MRI may also have a role in supporting the clinical diagnosis of ITON. Short T1 Inversion Recovery (STIR) sequence was first used to demonstrate focal optic nerve edema in acute ITON in 1994, Reference Takehara, Tanaka and Uemura2 but the topic remains largely unexplored. Recently, a small retrospective series demonstrated that diffusion-weighted imaging modalities can be used to calculate an apparent diffusion coefficient for the optic nerve that acts as a specific imaging marker for TON and furthermore corresponds with severity of vision loss. Reference Bodanapally, Shanmuganathan and Shin3 Another group has proposed that diffusion tensor imaging parameters in the acute setting following ITON may correlate with visual outcome measures such as retinal nerve fiber layer thickness and retinal ganglion cell count. Reference Li, Shi and Li4
No treatment for indirect TON has been shown to be effective, and observational studies of indirect TON demonstrate wide variability of recovery, time course, and end-point visual function. The only two large-scale randomized studies examining high-dose IV corticosteroids in indirect TON have failed to identify a benefit in visual outcome over observation. Reference Entezari, Rajavi, Sedighi, Daftarian and Sanagoo5,Reference Kashkouli, Yousefi and Nojomi6 Moreover, the MRC CRASH study concluded high-dose corticosteroids should not be routinely offered to patients suffering a traumatic head injury due to an elevated risk of death or severe disability. Reference Baigent, Bracken and Chadwick7 Levodopa is thought to have possible neuroprotective effects, and some authors have reported a beneficial effect thereof, Reference Razeghinejad, Rahat and Bagheri8 but this has never been explored in a large-scale, randomized controlled fashion.
Other treatments including IV erythropoietin, optic canal decompression, and transcorneal electrical stimulation have been trialed, though none have become routinely adopted clinically. Reference Singman, Daphalapurkar and White1
The normal clinical appearance and CT findings in acute ITON can complicate the confirmation of a diagnosis which has significant medicolegal and prognostic implications. Our case illustrates that MR imaging can be a useful adjunct acutely, even when the CT appears normal.
Acknowledgements
We thank the patient and his family for granting permission to publish this case report.
Funding/Support
None.
Conflicts of Interest/Disclosures
WT: None
MM: None
SS: None
JG: discloses payment or honoraria (Allergan, Bausch, and Lomb) for lectures, presentations, speakers bureaus, manuscript writing or educational events, unrelated to the subject of this article
AK: discloses contracts from external entities, payment, or honoraria for lectures, presentations, speakers, bureaus, manuscript, writing or educational events, payment for expert testimony, support for attending meetings and/or travel, participation on a Data Safety Monitoring Board or Advisory Board, leadership or fiduciary role in other board, society, committee or advocacy group, paid or unpaid, stock or stock options, and other financial or non-financial interests. All are unrelated to the subject of this article.
Statement of Authorship
JG, SS, AK, and MM had direct clinical contact with the patient, documented the case, and completed the background literature review. WT was the primary author of the case report and discussion and oversaw formatting, revision, and submission. JG and SS provided invaluable expertise in the refinement of the discussion, and AK was instrumental in the review process. All authors collaborated on the composition and revision of the manuscript text




