BACKGROUND
ACLS management of ventricular fibrillation consists of defibrillation, epinephrine, and amiodarone as standard of care.Reference Link, Berkow and Kudenchuk2 Although no formal definition has been established, when ventricular fibrillation persists despite the administration of at least 3 mg of epinephrine, 300 mg of amiodarone, and three attempts at defibrillation, some consider it to be refractory ventricular fibrillation.Reference Lee, Lee and Min3 The best management of these rare cases has not been clearly established. Evidence has emerged for the use of higher energy levels for defibrillation through the use of two defibrillators with two sets of pads discharged at once, known as dual-sequential defibrillation. Herein, we describe the successful termination of refractory ventricular fibrillation that did not respond to standard ACLS, esmolol, or dual-sequential defibrillation. We describe three defibrillators delivering energy simultaneously to the patient. To our knowledge, this is the first account of triple-sequential defibrillation used in refractory ventricular fibrillation.
CASE PRESENTATION
A 24-year-old male, with a previous history of seizure disorder and a history of substance-use disorder, was driving in a rural community, with his friends when he developed chest pain radiating to his arms. He was diaphoretic, and witnesses stated, “I am going to have a heart attack.” After pulling over, he went unresponsive and collapsed. His friends started CPR and called emergency medical services (EMS). Thirteen minutes later, paramedics arrived at the scene and encountered the patient, with vital signs absent and bystander CPR in progress. The initial rhythm assessment showed ventricular fibrillation (Supplemental material Figure 1). Defibrillation was first attempted with 200 J. He remained in ventricular fibrillation despite three subsequent shocks at 200 J until 22 minutes at which point ROSC was achieved (Supplemental material Table 1).
During transport, the patient reverted to ventricular fibrillation and remained in this rhythm until arrival at the hospital. Despite management per ACLS, the patient remained in ventricular fibrillation 45 minutes post-arrest. Dual-sequential defibrillation was attempted at 48 minutes post-arrest (Figure 1). This was unsuccessful at terminating the arrhythmia. At 51 minutes, there was a short duration of torsade de point on the monitor, and 5 g of MgSO4 was infused. Along with ongoing ACLS management at 56 minutes post-arrest, the patient received intralipid, as a toxic ingestion of a lipophilic substance was considered possible. His ventricular fibrillation persisted despite five further attempts of dual-sequential defibrillation.
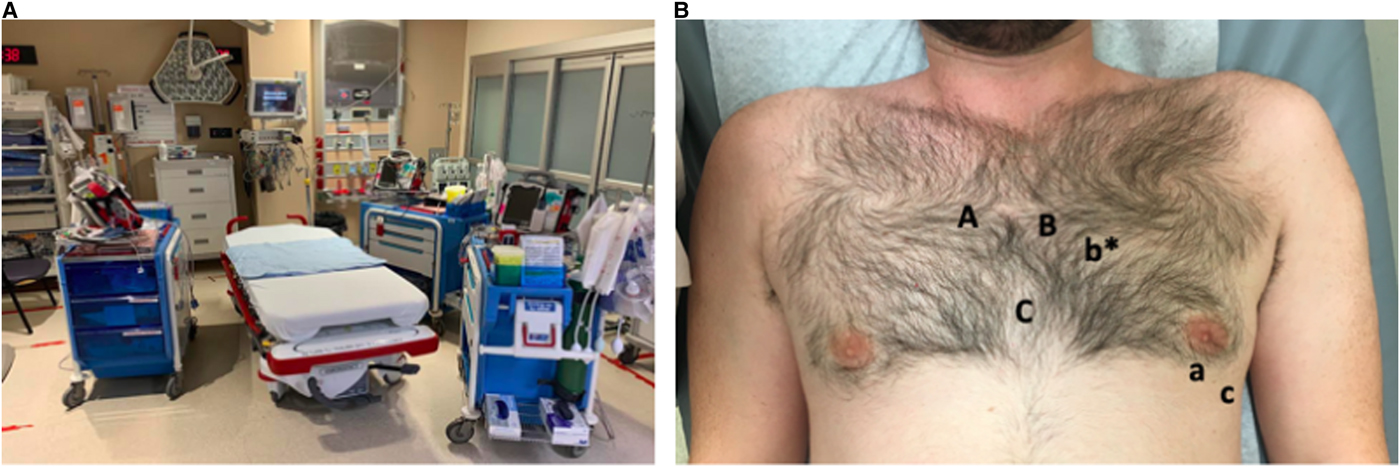
Figure 1. A) Figure 1A demonstrates the location of the defibrillators in the resuscitation room with regards to the patient's bed. There were two defibrillators on the patient's left, one at the head and one at the feet of the bed, as well as a third defibrillator on the patient's right. B) Figure 1B demonstrates the defibrillator pad placement on the patient's chest wall. The first set of pads (Set A-a) were placed in the Front-Apex position. The second set of pads (B-b*) were placed in the anterior-posterior positions (note that b* pad was placed on the patient's back). Finally, a third set of pads (Set C-c) was applied just below set A on the anterior chest and lateral to the a pad at the apex of the heart. The defibrillators used were three identical Philips Heartstart MRx.
At 67 minutes, a 30 mg bolus of esmolol was administered, along with a repeat attempt of dual-sequential defibrillation at 400 J. At this point, the team was considering terminating the resuscitation but decided to attempt triple-sequential defibrillation by attaching a third set of pads to the patient (Figure 1). Three different operators coordinated the delivery of shock simultaneously at the direction of the team. He received a total simultaneous dose of 600 J at 70 minutes post-arrest and went into a pulseless electrical activity (PEA) rhythm after a prolonged pause in electrical activity (approximately 10 seconds). After a further five minutes of CPR, ROSC was achieved. However, after three minutes, he reverted to ventricular fibrillation. At 80 minutes after the initial arrest, he received a second triple-sequential defibrillation shock, and ROSC was achieved. A post-ROSC ECG was obtained (Supplemental material Figure 2) showing an anterior ST-elevation MI. He was brought to the angiography suite where a complete left anterior descending artery occlusion was identified and stented (Supplemental material Figure 3); overall left ventricular systolic function was severely compromised (Grade 4 ventricle). He walked out of the hospital upon his discharge home 16 days later and was neurologically intact.
DISCUSSION
In this case, we report on a 24-year-old male who had out-of-hospital cardiac arrest. This patient was resuscitated over 82 minutes using standard ACLS algorithms, and non-ACLS interventions including esmolol and dual- and triple-sequential defibrillation.
Esmolol was attempted as case reports have demonstrated a potential role for esmolol in the treatment of refractory ventricular fibrillation.Reference Lee, Lee and Min3 The proposed mechanism is decreasing sympathetic surge that increases myocardial demand/ischemia, and, therefore, raising the threshold for ventricular fibrillation.
Dual-sequential defibrillation is a novel intervention for refractory ventricular fibrillation that has a small but growing body of evidence. When attempting defibrillation, the BIPHASIC trial showed that increasing the amount of energy corresponds to a better chance of defibrillation.Reference Stiell, Walker and Nesbitt4 As many defibrillators have a maximum deliverable energy of 200 J, dual-sequential defibrillation offers the opportunity to overcome the defibrillation threshold by increasing the amount of energy delivered to the myocardium. In addition, the vector of delivered energy during shocks may influence the efficacy of defibrillation that may explain why dual-sequential defibrillation may be beneficial in refractory ventricular fibrillation.Reference Davis, Schappert and Van Aarsen5 Triple-sequential defibrillation was attempted to address a potential vector issue and/or energy threshold that was preventing termination of ventricular fibrillation with dual-sequential defibrillation.
It is important to acknowledge that the multiple medications (esmolol, lidocaine, and amiodarone) given are potential confounders that may have contributed to the termination of the ventricular fibrillation. Note should also be made of potential harms that could occur with increased energy use for defibrillation: harm to those performing CPR with an accidental discharge, or harm to the defibrillators. In addition, higher energy use for defibrillation is associated with myocardial stunning. In our case, it is difficult to know if the left ventricular function (grade 4) immediately after ROSC was secondary to ischemia or was worsened by high-energy defibrillation.
This is a single case of triple-sequential defibrillation and, such, does not constitute evidence of efficacy or safety. However, it is another potential tool that could be employed in a difficult case of refractory ventricular fibrillation.
KEY POINTS
• In the event of cardiac arrest, high-quality CPR remains the priority as per the ACLS guidelines
• As highlighted by the neurologically intact state of this patient following over 80 minutes of downtime, efforts should be undertaken to resuscitate patients in refractor ventricular fibrillation receiving high-quality CPR.
• In refractory ventricular fibrillation, consider the use of multiple defibrillators to deliver sequential shocks when other interventions have failed.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/cem.2019.415.
Competing interests
None declared.



