Introduction
Heart failure and chronic obstructive pulmonary disease (COPD) are two serious conditions that result in high rates of morbidity and mortality across Canada. 1 - Reference Tsuyuki, Shibata and Nilsson 3 Respiratory distress, often associated with the decompensation of these conditions, is a common clinical presentation faced by Canadian emergency physicians. Many patients presenting to the emergency department (ED) with acute shortness of breath will respond to ED therapy and are discharged home.Reference Stiell, Clement and Brison 4 Nevertheless, a small but important proportion of such patients will require hospital admission. Making the appropriate disposition decision for such patients is often a challenging task. Physicians in the Unites States resolve this problem by admitting 80% of patients who present to the ED with decompensated heart failure.Reference Stiell, Clement and Brison 4 This is not a feasible approach in Canada where there is a notable hospital bed shortage and significant pressure to discharge. A recent study performed by our group found that only 38% of patients with acute decompensated heart failure were admitted to Canadian hospitals.Reference Stiell, Clement and Brison 4 Moreover, of the 65 serious adverse events reported in this study, 48% occurred in the cohort of patients who were discharged from the ED.Reference Stiell, Clement and Brison 4 In another recent study addressing COPD, it was found that 35% of COPD patients discharged from Canadian academic EDs returned to hospital within 30 days because of worsening respiratory symptoms.Reference Aaron, Vandemheen and Hebert 5 Taken together, these studies suggest that a need exists for a set of evidence-based decision tools to assist clinicians with making safe disposition decisions in these patient groups.
The Ottawa Heart Failure Risk Scale (OHFRS) and the Ottawa COPD Risk Scale (OCRS) were developed in order to fill this gap in clinical practice (Figures 1 and 2). The risk scales consist of seven and 10 items respectively, and include elements from a patient’s history, physical examination, and laboratory investigations. Patients are risk stratified based on their overall score to assist physicians in identifying the likelihood of patients experiencing a serious adverse event, with the ultimate goal of helping to guide physician disposition decisions. Each scale was developed through large multi-centre prospective cohort studies that analyzed dozens of different patient variables.Reference Stiell, Clement and Brison 4 , Reference Stiell, Clement and Aaron 6 The scales were then further refined by rigorous prospective validation studies, ultimately resulting in two unique decision tools that are both simple and predictive. The purpose of these risk scales was not to replace physician judgment or to serve as a threshold at which a clinician must act. Rather, it was to provide physicians with an accurate means of identifying which patients are at greatest risk for serious adverse events. This information can then be applied in the context of the greater clinical picture in order to facilitate safe patient disposition.
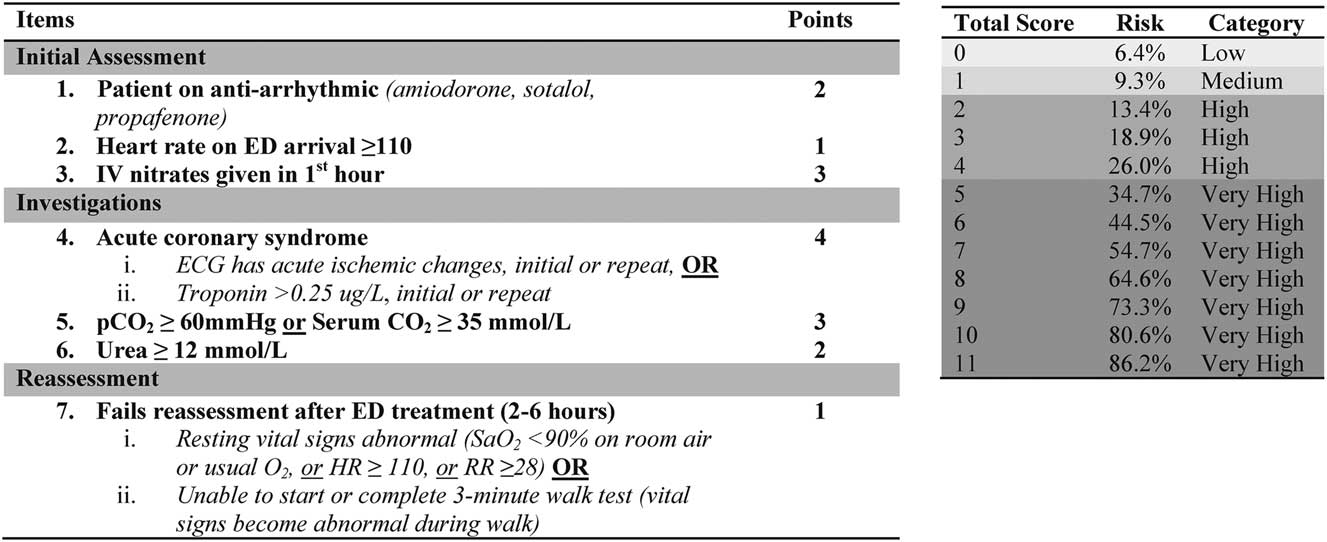
Figure 1 The Revised Ottawa Heart Failure Risk Scale.
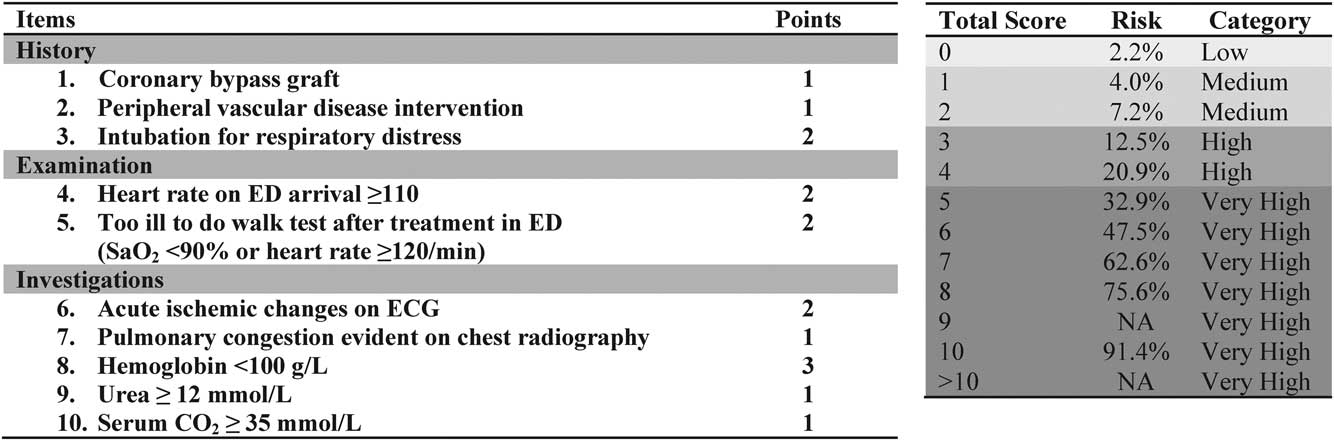
Figure 2 The Revised Ottawa COPD Risk Scale.
The primary objectives of the present study were to determine emergency physicians’ attitudes towards the OHFRS and OCRS and as to identify any barriers that may delay their implementation in Canadian EDs. Secondarily, we were interested in learning about what additional factors Canadian emergency physicians currently rely on to make disposition decisions in these patient groups. The data obtained from this study were anticipated to assist in the process of improving the OHFRS and OCRS so that they are clinically sensible and acceptable to physicians. This, in turn, should help ensure widespread uptake and implementation of these decision tools, improving patient outcomes in EDs across the country.
Methods
Study design and population
In this cross-sectional study, two self-administered online surveys were distributed to all 1,110 physician members of the Canadian Association of Emergency Physicians (CAEP) who had granted the organization permission to contact them with prospective research. Residents and medical students were excluded. On our behalf, CAEP randomly assigned half of the study population to receive the heart failure survey and the other half to receive the COPD survey. The surveys were distributed using the modified Dillman’s tailored design method,Reference Dillman 7 which consisted of a pre-notification email informing respondents about the goals of the study, a subsequent email containing the survey link, and three follow-up emails. Each email was spaced by a one-week time interval. This research was conducted by the University of Ottawa’s Department of Emergency Medicine and the Clinical Epidemiology Program of the Ottawa Hospital Research Institute between May and September of 2014. Approval was obtained from the Ottawa Health Science Network Research Ethics Board.
Survey design
The content of our surveys was informed through conducting individual interviews with five emergency physicians from the Ottawa Hospital with backgrounds in clinical research. Qualitative responses were recorded and analyzed. Themes were identified and ultimately used to develop the questions for our online surveys. In their final versions, each survey consisted of 16 questions that contained both open and closed-ended elements. The closed-ended questions were displayed in the format of a five-point Likert scale that required participants to rate the usefulness of the respective risk scales and their component criteria. These were mandatory fields. The open-ended questions were not mandatory and sought to identify potential barriers to risk scale implementation. They also attempted to determine what additional disposition factors respondents believed to be important when deciding upon patient disposition.
Outcome measures
The primary outcome measures were the overall participant ratings of the two risk scales and their component criteria in terms of their usefulness at helping to predict serious adverse events in patients with heart failure and COPD. Secondary outcomes included the likelihood of risk scale implementation into Canadian EDs, as well as the perceived barriers to such implementation.
Data analysis
Standard descriptive statistics were applied. Microsoft Excel (2011) was used for all calculations as well as for the creation of tables and graphical figures.
Results
In total, 403 of the 1,092 sampled Canadian EPs responded to our surveys, resulting in an aggregate response rate of 36.9%. The numerator represents all completed surveys, while the denominator represents all surveys sent, less those returned because surveys were undeliverable (n=18). Of the 403 completed surveys, 195 addressed the OHFRS and 208 addressed the OCRS.
Physician demographic, professional, and practice setting characteristics are summarized in Table 1. For both surveys, the majority of respondents were male, had at least one emergency medicine credential, and worked at either a community teaching hospital or major academic centre. The median years of practice was 15 and the majority of respondents worked in large-volume EDs that saw over 60,000 patients per year.
Table 1 Demographic and work characteristics of the 403 responding emergency physicians
* Fellow of the Royal College of Physicians
** Canadian College of Family Physicians Emergency Medicine certificate
*** Canadian College of Family Physicians
Table 2 provides disposition factors not included in the risk scales that respondents identified as being important. Patient’s cognitive status, comorbidities, and current living situation were the disposition factors most frequently identified in both surveys.
Table 2 Physician-identified disposition factors not included in risk scales
Table 3 provides physician-identified barriers that could potentially prevent the risk scales from being implemented into Canadian EDs. Issues with individual criteria or point allocation, and issues with scale complexity/accessibility were the two most frequently reported barriers in both surveys.
Table 3 Physician-identified barriers to risk scale implementation into Canadian EDs
Figure 3 illustrates physician approval of the OHFRS and its component criteria, as well as the perceived likelihood of risk scale implementation into Canadian EDs. Overall, 74.4% of respondents rated the scale as being “useful” or “somewhat useful.” The only component criteria that did not achieve an approval rating of above 70% were patient use of anti-arrhythmics (54.9%) and urea ≥12 mmol/L (51.3%). Based on a Likert scale rating of four or five, 66.7% of respondents believed that the risk scale would be implemented into Canadian EDs.
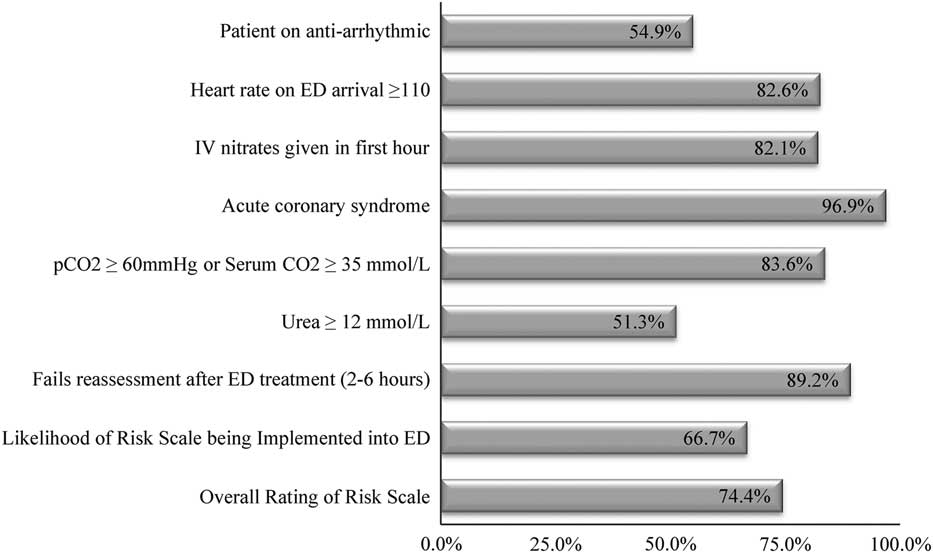
Figure 3 Overall approval of the Ottawa Heart Failure Risk Scale and component criteria (n=195).
Figure 4 illustrates physician approval of the OCRS and its component criteria, as well as the perceived likelihood of risk scale implementation into Canadian EDs. Overall, 76.9% of respondents rated the scale as being “useful” or “somewhat useful.” The component criteria that were rated the highest include history of intubation for respiratory distress (99.5%), acute ischemic changes on ECG (96.6%), heart rate ≥110 (90.9%), failure to perform walk test (97.6%), and pulmonary congestion on chest x-ray (93.3%). The only criteria that achieved an approval rating of below 70% were history of coronary bypass graft (51.4%), history of peripheral vascular disease intervention (45.7%), and again, urea ≥12 mmol/L (51.9%). Based on a Likert scale rating of four or five, 70.2% of respondents believed that the risk scale would be implemented into Canadian EDs.
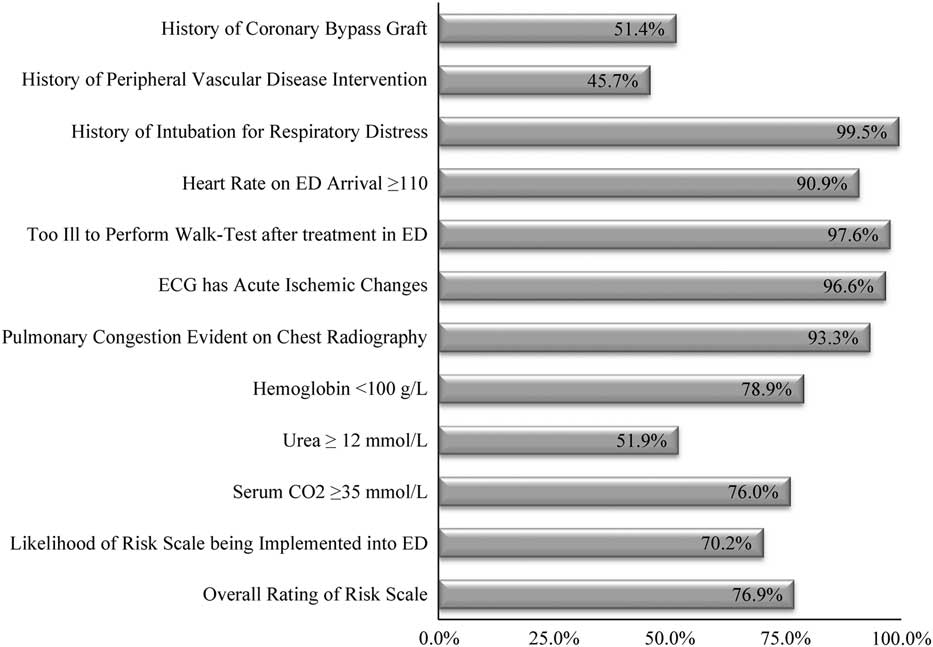
Figure 4 Overall approval of the Ottawa COPD Risk Scale and component criteria (n=208).
Figure 5 provides physicians’ response to a request to rate the importance of three specific disposition factors that were identified to be important in pre-survey qualitative data collection, but that were not included in the risk scales. Respondents in both survey groups strongly agreed that these factors were important when deciding upon patient disposition.
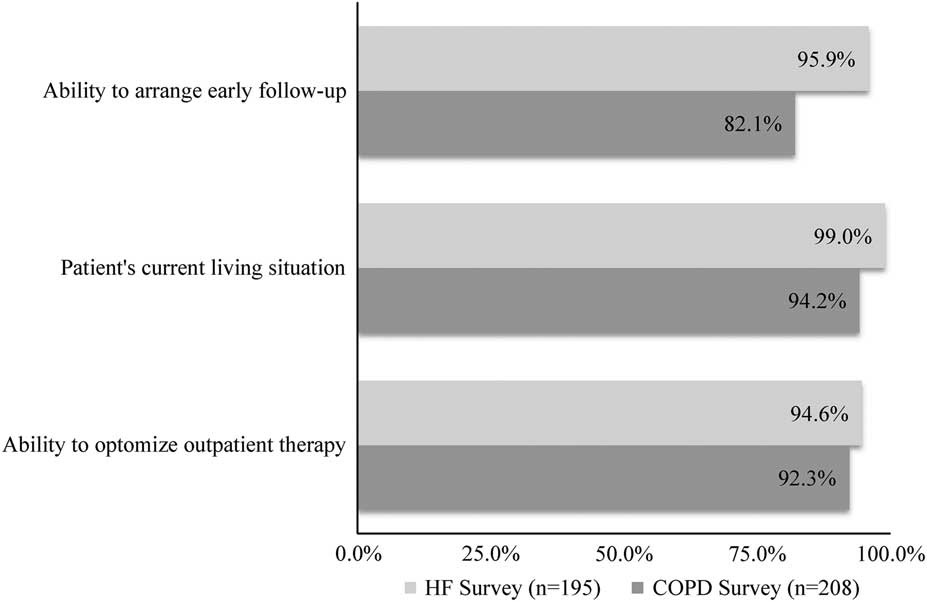
Figure 5 Physician rating of select disposition factors omitted from risk scales.
Discussion
Interpretation of results
Emergency physicians were very accepting of the new OHFRS and OCRS, which received comparable overall approval ratings of 74.4% and 76.9%, respectively. Many respondents felt that the risk scales fulfilled an important clinical need by providing an evidence-based decision tool that effectively minimizes uncertainty. Others felt that the scales’ main strength was that they provided a common language with which to discuss patient disposition with admitting services. Although physician response was generally positive, the newness of the risk scales potentially prevented an even more favourable outcome. As the scales are less than a year old, supporting literature has not yet fully permeated the emergency medicine community.Reference Stiell, Clement and Brison 4 ,6 This led to several concerns about risk scale validity and may have hindered a potentially more conclusive response.
Our secondary purpose was to identify any barriers that could prevent or delay risk scale implementation into Canadian EDs. While some respondents raised issues with individual criteria, others felt that there were some important disposition factors missing from the risk scales. With regard to the latter, patient comorbidities, ability to comply with management, access to home supports, ability to return to hospital, access to follow-up, and baseline functional status were all identified as important factors that were not addressed by the risk scales. Although each of these factors is arguably important when deciding upon definitive management, it is impossible for each of a patient’s personal factors to be included into a succinct bedside decision tool. To date, most successful bedside decision tools, including the Ottawa Ankle Rules and the Canadian C-Spine Rule,Reference Stiell, Wells and Vandemheen 8 - Reference Stiell and Bennett 10 have aimed to provide concrete answers to straightforward clinical presentations with dichotomous problems. With the new OHFRS and OCRS, however, we are attempting to address much more complex clinical issues where the answers are not binary. As such, the ultimate goal of these risk scales is not to make a decision for a clinician, but rather to help them assess a concise set of clinical variables that have been proven to be most predictive of poor patient outcomes. It is then up to the clinician to take this new information and apply it to the overall clinical situation, including the social variables mentioned above, in order to make the safest possible disposition decision for the patient.
Uncertainty regarding risk scale superiority over physician gestalt was another potential barrier identified by respondents. Each of the respective risk scales contain criteria that are relatively intuitive and other criteria that are less so. The intuitive criteria, such as acute coronary syndrome or vital sign abnormalities, are undoubtedly very important when deciding on patient disposition, but there would be no need for a decision tool if all of the criteria of importance were this overtly obvious, as physician gestalt would be more than adequate. We believe one of the main strengths of the OHFRS and OCRS is that they include criteria that are not immediately obvious to most emergency physicians. For instance, in a prospective cohort study of 945 patients, it was found that for acute exacerbations of COPD, a hemoglobin value of below 100 g/L was the factor most predictive of a subsequent serious adverse event.Reference Stiell, Clement and Aaron 6 As it turns out, a low hemoglobin value was as important as both a significantly elevated heart rate and acute ischemic changes on electrocardiogram (ECG) combined.Reference Stiell, Clement and Aaron 6 The latter was of great surprise to us when developing the risk scales, and we can only assume that the same would hold true for most emergency physicians. Interestingly, it was the criteria that were the least intuitive that fared the poorest when physicians were asked to rate the respective risk scales. The reasons likely relate to another reported barrier to implementation: risk scale complexity. Respondents felt that because certain criteria were not intuitive, the scales were too difficult to memorize. Others felt that the accessibility of the decision tools would be an issue in a fast-paced ED. To address both of these issues, it is our intention to develop a user-friendly mobile application that will provide easy access to both risk scales.
Strengths and Limitations
We achieved an overall response rate of 36.9%, which is very reasonable for a physician survey. Our open-ended questions became saturated well before achieving this value and, as such, we do not feel that additional responses would have yielded any incremental value. This being said, a potential limitation to our study is sampling bias. It is possible that the EPs who decided to respond to our surveys were more interested or motivated by the topic. Risk scale approval may therefore have been inflated. Further, our findings are based on Canadian data and the results are not necessarily generalizable to other countries. For instance, the usefulness of the risk scales may be limited in the United States, as emergency physicians there are not faced with the same bed pressure and can readily admit a higher proportion of patients. Our scales may have more applicability in countries with medical systems more similar to our own, such as the UK or Australia, and physician acceptance in these regions may be an interesting area of future research. Finally, how we decided to code our open-ended questions could have influenced our results. Because we took multi-faceted ideas and placed them into discrete categories, certain responses could be weighted more or less heavily based on our subjective interpretation of the data.
Study implications
The OHFRS and OCRS are the first decision tools to address the important presentations of decompensated heart failure and COPD and have the potential to change clinical practice. The results of this study allow us to take another step towards achieving this goal. Despite the rigorous research that went into developing these risk scales, including both prospective cohort and validation studies, it is often difficult to predict how the finished products will resonate with intended users. The strong approval ratings found in this study give us confidence that emergency physicians are ready for a tool that will help guide disposition decisions for these two important conditions. By highlighting potential barriers, we will be able to make adjustments that will make the tools more clinically applicable. The information gained from this study will help set the stage for larger implementation studies that will act as the ultimate benchmark for the effectiveness of the OHFRS and OCRS risk scales.
Conclusion
Canadian emergency physicians are supportive of the new OHFRS and OCRS. Unlike previous decision rules, the goal of these new risk scales is not to provide dichotomous answers to complex clinical issues, but rather to help physicians assess a succinct list of evidence-based clinical variables to assist them with patient risk-stratification. Beyond this, it will remain up to the physician to use all of the information at their disposal to make safe disposition decisions. It is our belief that if utilized effectively, these new risk scales will help fill a gap in clinical practice and improve outcomes for patients suffering from heart failure and COPD.
Competing Interests: None declared.










