INTRODUCTION
Sternal fracture is usually the result of significant blunt thoracic trauma and occurs more frequently in drivers wearing three-point restraint who are involved in a motor vehicle crash.Reference Knobloch, Wagner and Haasper 1 Its reported incidence varies between 0.33% of trauma patientsReference Recinos, Inaba and Dubose 2 and 3.7% of patients admitted after a motor vehicle crashReference Yeh, Hwabejire and DeMoya 3 and increases with age. It can be present in up to 27.7% of thoracic injuries associated with motor vehicle crashes in the extreme elderly population (>80 years of age).Reference Bansal, Conroy and Chang 4 Sternal fractures are often associated with other injuries, most commonly soft tissue contusions (56%) and rib fractures (49.6%).Reference Recinos, Inaba and Dubose 2 When isolated, they are associated with a reported mortality rate of between 0.7% and 3.5%. Poor outcomes are associated with the severity of other injuries, complications, and pre-existing comorbidity.Reference Yeh, Hwabejire and DeMoya 3 , Reference Brookes, Dunn and Rogers 5
Knowledge regarding the clinical significance of isolated sternal fracture has evolved, and many studies have demonstrated that patients with this injury can safely be discharged from the emergency department (ED) after investigation.Reference Hossain 6 - Reference Kouritas, Zisis and Vahlas 9 A retrospective cohort study found that cardiac complications were present in 0.8% of isolated sternal fracture cases.Reference Brookes, Dunn and Rogers 5 Clinically significant cardiac complications associated with isolated sternal fracture have been shown to be essentially nonexistent when an initial electrocardiogram and cardiac biomarker levels are normal.Reference Dua, McMaster and Desai 7 Current literature suggests that routine admission is no longer required for isolated sternal fractureReference Kouritas, Zisis and Vahlas 9 , Reference Velissaris, Tang and Patel 10 ; however, this practice remains widespread.Reference Hossain, Ramavath and Kulangara 11
Delayed hemothorax has been reported as an important complication with patients with minor thoracic injuries discharged from the ED, with an incidence of 7.4% of blunt thoracic injuries reported in EuropeReference Misthos, Kakaris and Sepsas 12 and 11.8% in North America.Reference Plourde, Émond and Lavoie 13 However, the only published prospective studies addressing delayed complications of minor thoracic injuries did not specifically assess isolated sternal fractures.Reference Misthos, Kakaris and Sepsas 12 - Reference Émond, Sirois and Guimont 14 Moreover, very few authors have studied functional outcome or pain experienced by patients with minor thoracic injuries or sternal fracture after ED discharge.Reference Émond, Sirois and Guimont 14 - Reference Daoust, Emond and Bergeron 17
The purpose of this study was to determine and compare complications and outcomes of patients with isolated sternal fracture discharged from the ED to those with other minor thoracic injury.
METHODS
Study setting and population
This prospective observational cohort study was conducted in four Canadian university-affiliated EDs (Hôpitaux l’Enfant-Jésus and CHUL of the CHU de Québec, Centre Hospitalier du Sacré-Cœur de Montréal, Centre hospitalier Charles-Lemoyne), between March 25, 2006 and November 2, 2010 and was a preplanned subanalysis of a larger project with prior publications involving the follow-up of patients with minor thoracic injury.Reference Plourde, Émond and Lavoie 13 , Reference Émond, Sirois and Guimont 14 , Reference Daoust, Emond and Bergeron 17 Patients ages 16 years and over who presented to the ED with a minor thoracic injury were screened for eligibility. Minor thoracic injury was defined by the presence of chest abrasion or contusion, or suspected or radiographically confirmed rib fracture. All participants were discharged from the ED after receiving care by the attending physician (primary care physician, emergency physician, or other specialist). Patients were excluded if 1) they had a hemothorax, pneumothorax, lung contusion, or any significant cerebral, thoracic, abdominal, or extremity injury diagnosed on their initial ED visit; or 2) a follow-up was not possible due to geographic or social circumstances; or 3) there was a delay greater than 3 days between the injury and the ED visit (a cut-off based on a previous publication showed that 90% of patients seeking medical attention in an acute care setting do so within 72 hours of injury).Reference Shields, Emond and Guimont 18 The study was approved by the Research Ethics Board of all four involved institutions, and written consent was obtained from study participants.
Study protocol
Initial ED care, evaluation, and data collection were left to the discretion of the attending physicians, who were blinded to the research protocol and study outcomes. Participants thus received usual care and standard discharge instructions. Participants then returned for standardized medical outpatient evaluations at 7 and 14 days post-injury. Assessment at these visits included pain severity, clinical examination, and an upright chest X-ray. There was no specific protocol regarding pain regimen, and this, too, was left to the discretion of the physician involved. Information on potentially significant delayed complications, including hemothorax, pneumothorax, atelectasis, and lung contusion, were obtained from the radiology report. Research nurses performed subject telephone interviews at 30 and 90 days post-injury, during which they captured data on severity of pain, functional status, and complications.
Primary outcomes
Delayed hemothorax was deemed present if pleural fluid was identified on the follow-up chest X-ray. A blinded radiologist made the final interpretation of these radiographs, and the size of hemothorax was not assessed. The decision on whether to treat a hemothorax was left to the discretion of the attending physician.
Functional status was assessed at 30 and 90 days, using the Medical Outcome Short-Form Health Survey (SF-12), a validated instrument derived from the more extensive SF-36 health survey.Reference Ware and Kosinski 19 It contains 12 questions that address 8 health elements: physical functioning in daily activities, role limitations due to physical health problems, overall bodily pain limiting usual activities, physical and mental health summary score, energy/fatigue, social functioning, and role limitation due to emotional health problems. Scores for each element range on a scale of 0-100, where 0 is the worst outcome and 100 is the best. Two aggregated summary scores (0-100) can also be derived: a global physical health summary (PHS) score and a global mental health summary (MHS) score. PHS, MHS, role limitations, physical functioning, and overall bodily pain were retained for analysis in our cohort and are presented in the results section. In order to make the interpretation of the outcome easier, disability was defined according to PHS and MHS scores that were normalized for age and gender of a North American population and categorized into none/mild (>40), moderate (25-40), and severe disability (<25), according to previous publications.Reference Andrew, Gabbe and Wolfe 20 , Reference Jenkinson, Chandola and Coulter 21
Data analysis
Clinical and demographic characteristics were described using univariate methods. We used the chi-square test for categorical variables and student t-test for continuous variables to assess primary and secondary outcomes. Comparisons of mean differences of the PHS scores adjusted for age, gender, and mechanism of injury, and presence of pulmonary comorbidities between categories at 90 days was performed using analysis of variance, also known as ANOVA. Correlation adjustment and Scheffé’s multiple test comparisons methods were included. Data analyses were performed using SAS 9.2 for Windows (SAS Institute, Gary, NC, USA).
RESULTS
A total of 2866 patients were screened for eligibility during the study period, and 969 were retained for analysis, as shown in Figure 1. Table 1 provides demographic and clinical characteristics of the study groups and illustrates the mean age of our study population—52.9 (±16.7) years old ranging from 16 to 95. Participants were slightly younger in the group of patients with minor thoracic injuries without fracture than in other groups, 50.9 (±17.5) versus 55.2 (±16.2) for sternal fracture group and 56.3 (±14.4) for rib fracture(s) group (p<0.001). Fifteen patients (46.9%) with isolated sternal fracture were age 65 or more. There were more males in the rib fracture(s) and thoracic injury without fracture groups than in the sternal fracture group (69.4% v. 60.2% v. 46.9%). Motor vehicle crash was the principal mechanism of injury (78%) in the sternal fracture group in contrast to falls in both of the other groups. One patient presenting with a sternal fracture associated with at least one rib fracture and was excluded from the analysis. This patient did not have delayed hemothorax identified at follow-up. Thirty-two patients (3%) had an isolated sternal fracture.

Figure 1 Flow diagram.
Table 1 Demographic and clinical characteristics of study groups

ASA=Aspirin; COPD=chronic obstructive pulmonary disease; SD=standard deviation.
Chi-square test for categorical variables, and test of student for continuous variables.
a Because of missing data, the number of patients does not always add to the total.
b One patient presented with a sternal fracture and at least one rib fracture and was excluded from primary outcomes analysis and thus not included.
*Fisher exact test.
Mean values of pulse, oxygen saturation, blood pressure, and respiratory rate were similar across groups. Missing data exist for mechanism of injury (n=1), smoking status (n=169), severe chest pain (n=200).
Table 2 provides information on delayed complication in the study population. Overall, 112 patients presented with a hemothorax within 14 days post-injury. The incidence of delayed hemothorax was 12.5% in the sternal fracture group (n=4), 23% in the rib fracture(s) group (n=70), and 6% in the minor thoracic injury without fracture(s) group (n=38), (p<0.05). All delayed hemothoraces in the sternal fracture group were detected before day 7, as were the majority of delayed hemothoraces in both of the other groups. One delayed hemothorax in the rib fracture group was detected after 14 days but kept for analysis in that group. None of the delayed hemothoraces in the isolated sternal fracture and thoracic injury without fracture groups required drainage. Three of the delayed hemothoraces in the rib fracture group were managed with drainage. The four participants in the sternal fracture group who developed delayed hemothorax were aged 53, 71, 73, and 75 years. One of those patients was taking aspirin, and none were on other antiplatelet or anticoagulant medications. Atelectasis was the only other delayed complication observed on follow-up radiographs in the sternal fracture group. No cases of pneumonia or pneumothorax were detected in the sternal fracture group, and few were present in both of the other groups. There were no cardiac complications listed, because patients were assessed and excluded at initial evaluation if such complications were present. No mortality was found in any participants at the 90-day follow-up.
Table 2 Delayed Complications

Chi-square test for categorical variables, and test of student for continuous variables.
*Fisher exact test.
a The percentages of patients do not add to the total for delayed hemothorax because one patient presented a delayed hemothorax after 14 days but was still included in the analysis.
Isolated sternal fracture patients had more important physical disability on SF-12 testing at 30 days (mean, SD: 30.6±11.2) compared to 35.2±10.5 and 39.6±12.6 for both of the other groups, respectively (p<0.001), as shown in Figure 2, A. At 90 days, only 42.9% of patients with sternal fracture had little to no disability, in comparison to 74.6% and 78.8% of patients from other groups (p<0.01), as shown in Figure 2, B. Of sternal fracture patients, 57.1% had moderate to severe disability compared to 25.4% and 21.2%, respectively, for both of the other groups (p<0.001). When taken separately, severe functional impairment was not statistically significant between groups. No significant difference was found between groups regarding the psychological disability. The incidence of a severe mental disability was low in all three groups at 90 days (0.0% for sternal fracture v. 3.2% for rib fracture(s) v. 4.2% for minor thoracic injury without fracture (p=0.8)). A comparison of mean PHS score differences at 90 days is presented in Table 3 and shows that sternal fracture was associated with overall significantly lower global mean PHS scores. The sternal fracture group had a lower score when compared with both the rib fracture(s) and the no fracture group.

Figure 2 Functional outcomes according to SF-12 physical score. A) Functional outcomes at 30 days according to SF-12 physical score. B) Functional outcomes at 90 days according to SF-12 physical score.
Table 3 Comparison of mean physical health summary (PHS) score differences at 90 days

¥ The p value was obtained with Scheffe multiple test comparisons
COPD=chronic obstructive pulmonary disease
Mean scores for physical functioning in daily activities at 30 days were significantly lower for the sternal fracture group (38.1±12.4 v. 44.5±11.8 v. 46.5±11.6, p<0.01), as shown in Figure 3, A. A similar non-statistically significant trend was seen at 90 days. At 30 and 90 days, role limitations due to physical health problems mean scores were also significantly lower in patients with sternal fractures, as shown in Figure 3, B. Scores at 30 and 90 days for overall bodily pain limiting usual activities were significantly lower for this group of patients. At 30 days, mean bodily pain score was 31.5±11.5 for sternal fracture in comparison to 36.7±10.9 and 40.1±12.7 (p<0.001) for both of the other groups. Following the same pattern, at 90 days, mean bodily pain score was 41.0±15.3 for sternal fracture in contrast to 48.9±10.7 and 50.9±10.3 (p<0.001) for both of the other groups.
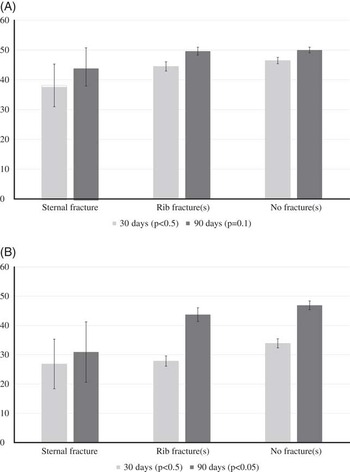
Figure 3 Physical functioning in daily activities and role limitations due to physical health problems at 30 and 90 days. A) Physical functioning in daily activities at 30 and 90 days. B) Role limitations due to physical health problems at 30 and 90 days.
Participants were deemed lost to follow-up if they had no visit within 14 days of initial assessment. Of the 969 initial participants, 79 (8.1%) were lost to follow-up. Those participants were younger (44.4±17.5), included a higher proportion of smokers, and presented with less severe dyspnea at rest at the initial evaluation compared to our participants. No other significant difference was found between patients lost to follow-up and the fully studied cohort. Data were available for 746 (83.7%) and 624 (70.0%) for the 30- and 90-day follow-up interviews, respectively. The number of participants followed at 30 days was approximately the same for each group (90.9% for sternal fracture v. 94.1% for rib fracture(s) v. 95.7% for minor thoracic injury without fracture(s) [p=0.4]). Although the proportion of complete data at 90 days was lower in the sternal fracture group than in the other groups (50% v. 79.7% and 79.9%, p<0.05), characteristics of the patients with missing data were similar in all three groups. No significant difference was found between participants with available data at 90 days and those with missing data in the sternal fracture group.
DISCUSSION
To our knowledge, this is the first prospective study to comparatively evaluate the complications and functional outcomes of isolated sternal fracture in trauma patients discharged from the ED.Reference Misthos, Kakaris and Sepsas 12 - Reference Émond, Sirois and Guimont 14 Current evidence suggests patients with isolated sternal fracture should not be admitted to the hospital,Reference Hossain, Ramavath and Kulangara 11 hence the relevance of our comparison of patients with isolated sternal fracture with those with minor thoracic injuries. The 3.2% incidence of sternal fracture in our study population is similar to that reported for blunt thoracic injuries.Reference Recinos, Inaba and Dubose 2 , Reference Yeh, Hwabejire and DeMoya 3 We found that approximately one out of eight patients with an isolated sternal fracture developed a delayed hemothorax. This incidence was less than in the rib fracture(s) group, an injury known to be associated with delayed pulmonary complications, including hemothorax.Reference Plourde, Émond and Lavoie 13 None of the delayed hemothoraces in the sternal fracture group were managed with drainage, raising questions about the clinical significance of these radiologic findings. This situation could arise from the small number of isolated sternal fracture presenting with delayed hemothorax (n=4) in our cohort, or could be that significant delayed hemothorax is rarely associated with isolated sternal fracture. Because the 11.6% incidence of all delayed hemothorax was slightly higher than previously reported,Reference Misthos, Kakaris and Sepsas 12 , Reference Plourde, Émond and Lavoie 13 the latter possibility seems more likely; however, further research would be required to answer this question definitively.
No previous study has reported on the functional impact of isolated sternal fracture on activities of daily living. It has been previously established that pain persists for a mean of 10.9 weeks and is significantly prolonged in patients over 50 years of age with isolated sternal fracture.Reference de Oliveira, Hassan and Sebewufu 16 , Reference Daoust, Emond and Bergeron 17 Our results suggest that this pain can contribute to a major physical impairment. Indeed, when considering specific items of the SF-12 scale, such as physical functioning, role limitation, and overall bodily pain, patients with isolated sternal fracture were found to have more limitations than patients from other groups. It is possible that the functional limitations engendered by an isolated sternal fracture originated from the pain, delayed hemothorax,Reference Émond, Sirois and Guimont 14 and global limitations in daily activities and roles. This possibility raises a concern of sufficient analgesia at discharge and emphasizes the importance of follow-up. It also corroborates some of our collaborators’ conclusions that raised the importance of a better follow-up of patients with minor thoracic trauma,Reference Shields, Emond and Guimont 18 especially when delayed hemothorax is detected.Reference Émond, Sirois and Guimont 14 Because sternal fractures do not seem to generate more psychological disability than other minor thoracic injuries, it seems logical that efforts should focus on the prevention of physical disability, which itself appears to lead to global functional impairment. Future studies should focus on factors that may increase the risk of developing a significant disability, analgesia at discharge, and the use of follow-up resources by patients with isolated sternal fracture.
The principal limitations of our study arise from missing data, in particular, in the sternal fracture group at 90 days, and limits the scope of our functional outcomes results at that time point. We found that participants with missing data had similar baseline characteristics to those with fully available data, potentially limiting the impact of these losses on the results at 90 days. We feel that, as a result of our study protocol and logistics, it remains unlikely that patients lost to follow-up had major problems. Another limitation is that our participants’ pre-injury functional status was not evaluated at their initial visit. This is known to be an important factor for the post-injury functional outcome and should be considered in the interpretation of our results. For this reason, our statistical analysis SF-12 scores were normalized for age and sex to minimize confounding from these factors. The fact that any visible pleural fluid on the chest X-rays was deemed to be hemothorax is also a limitation that should be considered. There was no way, except drainage, to differentiate hemothorax from another effusion in our study. However, given the traumatic context, we felt it was reasonable to assume that any acute pleural fluid represented a delayed hemothorax. Finally, the fact that medical initial care and follow-up management were not standardized may also appear to some to be a limitation. However, our protocol that arose from this pragmatic design was intended to reflect as much as possible the actual care given in our EDs. The evaluation of the clinical importance of complications was left to the discretion of the treating physician and was not reported in our study for the same reason.
CONCLUSIONS
In this prospective study, we found that 12.5% of patients with sternal fracture developed a delayed hemothorax, but the clinical significance of this remains questionable. The proportion of patients with sternal fracture who had moderate to severe disability was significantly higher than that of patients with other minor thoracic trauma.
CLINICAL IMPLICATIONS
As a result of this new information that sternal fracture patients have more disability than patients with other minor thoracic traumas at 90 days, we feel clinicians should ensure that patients discharged from the ED with isolated sternal fracture have adequate analgesia and easy access to physician follow-up. Clinicians should also investigate for complications when assessing these patients during follow-up visits.
Acknowledgements: The results of this work were presented as a poster at the 31st Annual Meeting of the Association de Médecine d’Urgence du Québec and at the 9th Conference of the Département de médecine familiale et médecine d’urgence de l’Université Laval. We acknowledge Valérie Boucher from the CHU de Québec Research Center for editing and reviewing the manuscript and Brice Lionel Batomen Kuimi, MSc, who was in charge of the statistical analysis. We also thank Cong Tran, Marilyne Dufresne, Patricia Chabot, and Julie Lessard who have worked on data collection and day-to-day management, as well as the emergency physicians who participated in the recruitment of patients. SR was in charge of the literature review, data analysis and interpretation, and writing of the manuscript. Marcel Émond had full access to all of the data and takes responsibility for the integrity of the data and the accuracy of the data analysis. He was responsible for the design and conduct of the study. J-SA-C was involved in the literature search, review, and approved the manuscript. CG, LM, J-MC, NLS, EB, and LV were responsible for recruitment, and reviewed and approved the manuscript. This work was supported by a grant from Fonds de la Recherche en Santé du Québec (FRSQ 14056). This study has been approved by the Comité d’éthique de la recherche du CHU de Québec (institutional review board) (2012-1323).
Competing interests: None declared.








