BACKGROUND
The opioid epidemic in Canada remains a key focus of the federal government in its recent Opioid Action Plan to curb the public health crisis in overdoses and deaths nationwide. 1 Previous work by the Canadian Centre on Substance Abuse advocates for a multi-pronged strategy by national organizations to develop evidence-informed guidelines and policies for prescribing opioids in their clinical settings. 2 These national initiatives, in conjunction with Canadian and international clinical practice guidelines, all advocate thorough patient assessments, risk stratification, and ongoing safety monitoring of patients using opioids to ensure proper benefits and reduced harms. The emergency department (ED), however, is a challenging environment in which many of these recommendations cannot be practically met.
One specific area of concern remains the possibility of long-term use or addiction in patients receiving their first opioid prescription in the ED. There is limited research exploring the risk of long-term opioid use/dependence with prescriptions initiated in the ED. Recent studies have shown a steadily increasing rate of opioid prescribing in the ED, and that receiving an opioid prescription in the ED can lead to a significant increase in long-term opioid use.Reference Mazer-Amirshahi, Mullins, Rasooly, van den Anker and Pines 3 - Reference Butler, Ancona, Beauchamp, Yamin, Winstanley, Hart, Ruffner, Ryan, Ryan, Lindsell and Lyons 5 This study elaborates the growing risk of initiating opioids in the ED and the risk of long term use.Reference Barnett, Olenski and Jena 6
METHODS
The authors performed a retrospective analysis of a U.S. national Medicare and Medicaid beneficiary database examining ED visits from 2008 to 2011 (n=377,629 patients), where an opioid was prescribed to ED-discharged patients (captured from the Medicare Part D Event file) who had not received an opioid prescription in the preceding 6 months. Only one visit per recipient was included, and any ED visits resulting in hospital admission were excluded. Patients with cancer or with hospice claims were also excluded. Physicians with less than five ED visits or hospitals with less than five ED physician billings per ED were also excluded. Admitting diagnoses were obtained from the 2008-2012 MedPAR (Medicare Provider Analysis and Review) files. Opioid prescriptions were linked to emergency physicians who were divided into quartiles of prescribing “intensity.” In-hospital and between-hospital variations in prescribing physician groups were assessed in a logistic regression model designed to predict the probability of being treated by a “high intensity” versus “low intensity” physician prescriber, adjusting for patient clinical and sociodemographic variables, as well as an initial ED visit diagnostic code. Patients treated by high-intensity prescribers were then matched 1:1 with low intensity controls with the closest propensity score within the same hospital for comparison purposes. Propensity scores were used to reduce the bias of the outcome estimate by adjusting for multiple potential confounding variables.
The main exposure was defined as treatment by a high-intensity or low-intensity ED opioid prescriber based on in-hospital quartiles. The alternate exposure classified physicians based on total morphine equivalent (MEQ) doses prescribed.
The primary outcome was long-term opioid use, defined as 180 days or more of opioids supplied to the patient within 12 months after the initial ED visit, excluding prescriptions in the 30 days following that visit (due to the correlation with the main initial exposure). Secondary outcomes included rates of hospital encounters related to opioid exposures in the 12 months after the initial ED visit, as well as ED visits 14 to 30 days after the initial visit with a low-intensity provider, to assess for possible under-treatment of pain conditions.
RESULTS
Outcomes for opioid prescribing and dependence are summarized along baseline factors in Table 1. Patients treated by high-intensity prescribers (n=215,678) were not demographically different from those treated by low-intensity providers (n=161,951) with respect to age, gender, race, pain diagnoses, disability level, chronic comorbidities, or census region in the United States.
Table 1 Opioid prescribing and long-term opioid use (select baseline factors, n=377,629 patients).

ED=emergency department; HIP=high-intensity prescriber; LIP=low-intensity prescriber.
Patients seen by high- versus low-intensity prescribers received opioid scripts at a rate of 24.1% and 7.3%, respectively (overall average rate of 14.7% for whole cohort and a variance factor of 3.3). Rates of subsequent long-term use for the high-intensity versus low-intensity prescribers were 1.51% and 1.16%, respectively (odds ratio [OR] 1.31, 95% confidence interval [CI] 1.23-1.37; number needed to harm=48 to create 1 long-term opioid user).
Differences in long-term use between prescribers were consistent across all subgroups, with minimal changes after multivariate adjustments. Rates of prescribing for patients with injury (falls, fracture) were statistically higher in the high-intensity group (OR 1.07, 95% CI 1.03-1.11, p<0.001). Return visits in the 14- to 30-day period for under-treated pain were similar in both groups, as were hospital encounters for any reason at 12 months after the index ED visit. Opioid dosing (total MEQ prescribed) was not different between high-intensity and low-intensity prescribers.
Validity of results
This was a retrospective observational study of administrative data of U.S. Medicaid/Medicare patients, analysing prescribing patterns based on ED-level physician quartiles within hospitals. U.S. Medicare/Medicaid patients are generally seniors>65 years of age, younger patients with disabilities, or families with lower incomes or other health-adverse circumstances. As such, these patients may not be representative of all U.S. or Canadian ED patients (i.e., limited generalizability of these results). This study cohort was also older (age 68 years) and had multiple comorbidities (3.6), which may also not be representative of all North American ED opioid recipients.
As an observational study, it shows potential associations between exposures and outcomes but not necessarily causality. The authors did note, however, a step-wise increase in long-term opioid use through each physician prescribing frequency quartile, suggesting a dose-response relationship. The authors outline their best efforts to minimize potential selection bias. They acknowledge their inability to capture appropriateness of opioid indications, to quantify overuse of opioids, to limit use of administrative Medicare data (not generalizable to other ED patients), and to unequivocally attribute specific prescriptions to individual ED physicians. The authors did comment on the possibility of “clinical inertia,” where subsequent prescribers continued ED-initiated opioids in outpatient settings, although this was not formally analysed. Authors did not comment on opioid use prior to the 6-month pre-index ED visit, which may confound the risk of dependence reported in this retrospective study. Finally, using administrative data with such large numbers (n>370,000) inevitably leads to statistically significant results, although the clinical significance of such differences may not be as relevant (e.g., higher risk of opioid use in high-intensity prescribers for falls/fracture OR 1.07 [95% CI 1.03-1.11], p<0.001, which is highly statistically significant but not likely clinically significant).
Implications of the results
These results suggest that starting patients on opioids in the ED in an otherwise opioid-naïve patient could lead to long-term use (NNH 48). This mirrors recent work demonstrating an increased adjusted OR of 1.8 for opioid-naïve patients becoming long-term opioid users at 1 year,Reference Hoppe, Kim and Heard 4 and the development of opioid addiction after initial ED opioid script.Reference Butler, Ancona, Beauchamp, Yamin, Winstanley, Hart, Ruffner, Ryan, Ryan, Lindsell and Lyons 5 A 49% relative increase (10% absolute) in adult ED opioid prescribing in the United States has been demonstrated from 2001 to 2010.Reference Mazer-Amirshahi, Mullins, Rasooly, van den Anker and Pines 3 Volkow et al. (2011) showed that U.S. ED physicians were the third most common opioid prescribers for outpatients<40 years of age, in a nationwide sample of 79.5 million scripts written in 2009, ranging from 7% to 14%, depending on age strata.Reference Volkow, McLellan and Cotto 7 Coincidentally (but not causally), the Drug Abuse Warning Network (DAWN) report has shown a 134% increase in ED opioid-related visits from 2004 to 2010. 8
FUTURE CANADIAN DIRECTIONS
There is a significant lack of accurate information regarding Canadian ED opioid prescribing patterns, and resultant risk of long-term opioid use (or other harms) in our patients. It is not clear whether provincial monitoring databases can be easily accessed and interrogated by ED investigators to answer these questions. Also, there is a lack of high-quality guidelines that address ED-specific issues in prescribing opioids, although an ACEP 2012 clinical policy does provide a limited number of weak recommendations based on low-quality evidence.Reference Cantrill, Brown, Carlisle, Delaney, Hays, Nelson, O’Connor, Papa, Sporer, Todd and Whitson 9 , Reference Ducharme 10
There is an urgent need for ED-specific guidelines to address unique issues around opioid prescribing for Canadian ED physicians, as outlined in Box 1. International opioid guidelines are essentially silent on ED-prescribing issues (Upadhye et al., manuscript in preparation). There has been an explosion of local ED- or city-specific ED opioid guidelines in North America, although it is not clear whether any of these are evidence-based or peer-reviewed. A recent institutional ED guideline implementation did demonstrate a reduction in opioid prescribing from 52.7% to 29.8% immediately after introduction, and a sustained reduction at 33.8% after 12 to 18 months.Reference Del Portal, Healy, Satz and McNamara 11 The diversity of Canadian ED physician practitioners would likely benefit from a provincially or nationally standardized approach to opioid use, adapted for local realities.
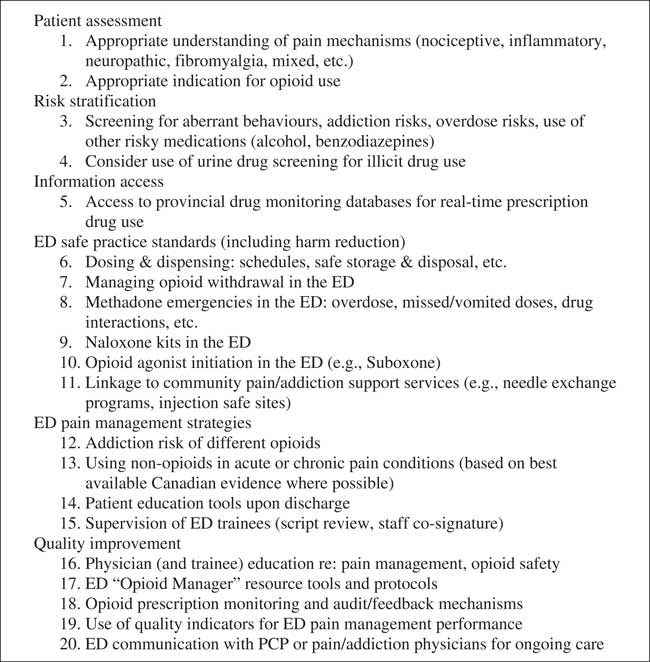
Box 1 Potential topic areas for new Canadian ED opioid guideline. ED=emergency department; PCP=primary care physician.
Finally, it is imperative for Canadian ED physicians to avoid a “no opioids” stance in their practices. Health Canada has recently unveiled its Action on Opioid Misuse plan, advocating for non-opioid and safer opioid-prescribing practices for various pain conditions. 12 There is a lack of high-quality evidence regarding the use of opioids in treating ED outpatients, which does not mean that they do not work (i.e., absence of evidence of effect is not equal to evidence of absence of effect). A balanced approach is needed to prescribing opioids in the ED to adequately treat pain yet respect public health concerns.
Competing interests: None declared.




