CLINICIAN'S CAPSULE
What is known about the topic?
Ontario is experiencing an increase in invasive group A streptococcal infections, with the highest incidence of cases in Northwestern Ontario.
What did this study ask?
What are the clinical and laboratory characteristics of patients presenting to the ED with invasive group A streptococcal infections?
What did this study find?
Patients with invasive group A Streptococcus present with mild tachycardia and tachypnea at triage, and a consistently elevated C-reactive protein (CRP).
Why does this study matter to clinicians?
The CRP should be measured in suspected infections, but clinical judgment should override reassuring vital signs and laboratory values.
INTRODUCTION
Group A Streptococcus, or Streptococcus pyogenes, is an aerobic gram-positive coccus capable of producing infection ranging from uncomplicated pharyngitis to life-threatening necrotizing soft tissue infections.Reference Cole, Barnett, Nizet and Walker1–Reference Terao5 Invasive group A streptococcal disease is defined as “laboratory confirmation of infection with or without clinical evidence of invasive disease” and “requires the isolation of group A Streptococcus from a normally sterile site”.6 In Canada, invasive group A streptococcal infections have been nationally reportable in every province and territory since 2000. Evidence from this reporting system suggests that the rate of invasive group A streptococcal infections has more than doubled since data collection began.7
Group A streptococcal infections have the potential to present insidiously early in the disease process, with severity ranging from mild (e.g., cellulitis, streptococcal pharyngitis) to life-threatening (e.g., necrotizing soft tissue infection, streptococcal toxic shock syndrome).Reference Lancerotto, Tocco, Salmaso, Vindigni and Bassetto8,Reference Walker, Barnett and McArthur9 Necrotizing soft tissue infections are one type of invasive group A streptococcal infection that involve tissue destruction at the level of the fascia, muscle, or skin.Reference Stevens and Baddour10 The Laboratory Risk Indicator for Necrotizing Fasciitis (LRINEC) score was published in 2004 as a laboratory-based scoring system to help clinicians distinguish between necrotizing fasciitis and non-necrotizing soft tissue infections.Reference Wong, Khin, Heng, Tan and Low11 The importance of early diagnosis in invasive group A streptococcal disease cannot be overstated, as these infections can rapidly progress, even in healthy individuals, to severe sepsis with accompanying multi-organ system failure.Reference Lappin and Ferguson12 Public Health Ontario reports that 10.1% of invasive group A streptococcal infections in 2016–2017 were fatal.13
Prior studiesReference Davies, McGeer and Schwartz14–Reference Ben-Abraham, Keller, Vered, Harel, Barzilay and Paret16 have described population demographics and risk factors associated with invasive group A Streptococcus; however, there is a relative paucity of data describing the clinical features of these patients when they present to the emergency department (ED). The purpose of this study was to describe the clinical and laboratory characteristics of patients presenting with invasive group A streptococcal infections to a tertiary care center ED in a geographic area with a relatively high volume of cases.
METHODS
Study design and time period
We conducted an electronic health records review of all patients presenting to our hospital from January 2016 to December 2017 inclusively with a final diagnosis of an invasive group A streptococcal infection. The primary author (K.D.) objectively extracted the data using a standardized Microsoft Excel spreadsheet with free text and drop down lists, and was not blinded to the outcome. A second data abstractor (M.G.) verified the accuracy of the data recorded when questions arose, particularly regarding the number of separate culture sites and ensuring the case definition of invasive group A streptococcal infection was met.
Study setting
Patients were eligible to be included in the study if they presented to the Thunder Bay Regional Health Sciences Centre (TBRHSC) ED. TBRHSC is the regional referral center for Northwestern Ontario and the closest hospital for just over half of its citizens. Northwestern Ontario comprises approximately 47% of the land mass in Ontario, but only 2% of its population (231,000 people).17 Patients transferred from other centers who were not first seen in our ED were excluded from the study as their triage information was not accessible electronically. This study was approved by the TBRHSC Research Ethics Board.
Population
We included all adult and pediatric patients, regardless of age, with a visit to our ED for invasive group A streptococcal infection. Medical records were eligible to be reviewed if they contained one of the ICD-10 codes listed in Online Appendix 1, based on the Public Health Agency of Canada's (PHAC) national case definition of invasive group A streptococcal disease.18 A normally sterile site was defined as blood, cerebrospinal fluid, pleural fluid, peritoneal fluid, pericardial fluid, deep tissue specimen taken during surgery, bone, or synovial fluid.6 ED visits for streptococcal pharyngitis (e.g., J02.0, J03.0) were excluded from the study as they did not meet the case definition for invasive disease. Patients were also excluded if they had a superficial group A Streptococcus wound culture or a non-necrotizing skin or soft tissue infection.
Outcome measures
Our primary objective was to obtain demographic, clinical, and laboratory characteristics of patients presenting to the ED with invasive group A Streptococcus. Demographic data included date of birth, sex, and dwelling type. Information regarding the visit, including date of presentation, hospital length of stay, preceding ED visits or hospitalizations, disposition, and death was collected. Host characteristics such as immunization status, methicillin-resistant Staphylococcus aureus (MRSA) colonization, pregnancy, diabetes mellitus, active cancer, transplant recipient, human immunodeficiency virus (HIV) status, alcohol abuse, and intravenous drug use (IVDU) were gathered. We recorded the triage vital signs, Canadian Triage Acuity Scale (CTAS) score, and site(s) of group A Streptococcus culture. Finally, extracted laboratory values were selected based on the LRINEC score, which is comprised of the white blood cell (WBC) count, hemoglobin (Hgb), sodium (Na), blood glucose (BG), creatinine (Cr), and C-reactive protein (CRP).Reference Wong, Khin, Heng, Tan and Low11
Data analysis
Summary statistics were calculated for all observed variables, including mean, standard deviation (SD), median, interquartile range (IQR), and range, where appropriate. Analysis of variance and cross-tabulations were calculated to determine whether LRINEC score or the socio-demographic characteristics of age and sex could predict hospital length of stay. Missing data were dropped from analysis. Data analysis was conducted using STATA 14 software.
RESULTS
Health characteristics
A total of 45 adult and pediatric cases were identified over the 2-year period. There was only one pediatric case in this sample, which was removed, leaving 44 adult cases for analysis. The median age of the adult sample was 44 years, and ranged from 21 to 92 years old, with an IQR of 35 to 52 years. Thirty (68%) of the cases were male. The relevant patient characteristics and past medical history are listed in Table 1. The prevalence of diabetes mellitus and alcohol abuse in our sample was substantially higher than in the population of Northwestern Ontario.19 Two-thirds of the cases presented in the fall and winter months. All but one case was admitted to hospital, and of those 13 (30%) were admitted to the intensive care unit (ICU). Six (14%) died before hospital discharge. One-third of all cases had an ED visit in the 7 days preceding their hospital admission for invasive group A streptococcal disease. The national incidence of invasive group A streptococcal infections in Canada was 6.0 per 100,000 in 2016 and 6.8 per 100,000 in 2017.7 Based on our adult and pediatric identified cases, the incidence of invasive group A streptococcal disease in the Thunder Bay region was 11.5 per 100,000 in 2016 and 25.5 per 100,000 in 2017.20
Table 1. Characteristics of the 44 adult patients with invasive group A streptococcal infections

*MRSA colonization at the time of admission was missing in 18 cases.
Triage
The average adult patient in this sample presented as a CTAS 2 with tachycardia and tachypnea, but was afebrile, normotensive, and saturating well on room air (Table 2). The mean presenting heart rate was 111 beats per minute (bpm), and median respiratory rate was 20 breaths per minute. Thirty-two (73%) patients were tachycardic with a heart rate ≥ 100 bpm, and 27 (63%) were tachypnic with a respiratory rate ≥ 20 breaths per minute. Only 14 (32%) patients had a temperature ≥ 38°C tympanic, and there was one hypothermic patient with a temperature < 35°C. Three (7%) patients had a systolic blood pressure < 100 mmHg.
Table 2. Triage vital signs and CTAS score of the 44 adult patients presenting with invasive group A streptococcal infections
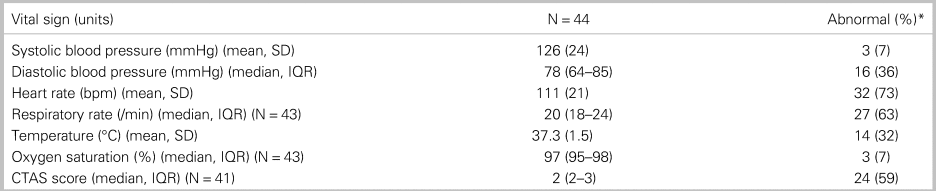
* Systolic blood pressure < 100, diastolic blood pressure < 70, heart rate ≥ 100, respiratory rate ≥ 20, temperature ≥ 38°C, oxygen saturation ≤ 92%, CTAS 1-2.
Laboratory values and microbiological cultures
The mean and median laboratory values are listed in Table 3. Most notably, the CRP was elevated in all patients in whom it was measured, with a mean of 249 mg/L (SD 143) and range of 17–596 mg/L. There were 55 microbiological cultures in 44 patients that were positive for invasive group A Streptococcus (Table 4). Thirteen patients (30%) had more than one positive culture site. The majority of the cultures originated from the soft tissues and blood; in other words, necrotizing soft tissue infections and sepsis were the two most common invasive group A Streptococcus presentations. Other diagnoses included septic joints, pneumonia, urinary tract infections, and Fournier's gangrene.
Table 3. Laboratory characteristics of the 44 adult patients presenting with invasive group A streptococcal infections
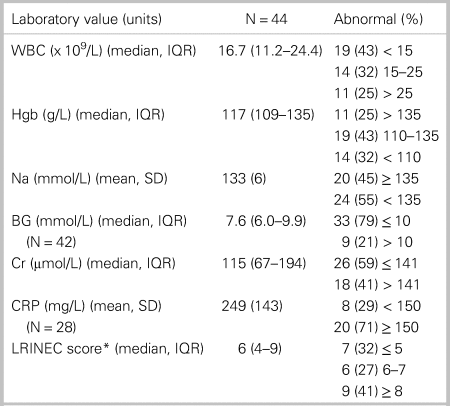
*LRINEC score was only calculated for the 22 patients with a necrotizing soft tissue infection.
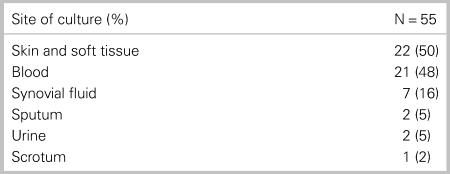
Table 4. Sites of the 55 cultures positive for group A Streptococcus
LRINEC score
There were 22 cases of necrotizing soft tissue infections. In these culture-confirmed cases, seven (32%) had a low risk LRINEC score, six (27%) had a moderate risk score, and nine (41%) had a high risk score for necrotizing soft tissue infection. There was a statistically significant positive correlation between the patient's LRINEC score and hospital length of stay (r = 0.46; p < 0.01) (Figure 1). All other comparisons of association between patient characteristics and outcomes were not statistically significant at an alpha level of 0.05.
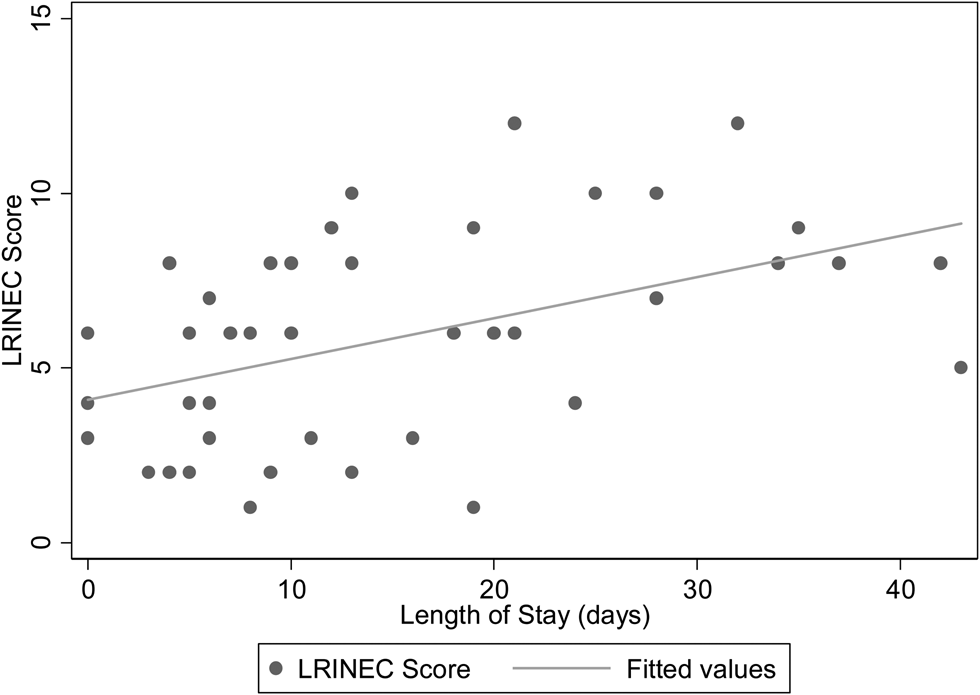
Figure 1. Correlation between LRINEC score and hospital length of stay.
DISCUSSION
This study demonstrates the variable and oftentimes insidious presentation of invasive group A streptococcal disease to the ED. The nonspecific clinical picture of early invasive group A streptococcal infections potentially explains why one third of patients in our sample had visited the ED in the week preceding the diagnosis, challenging conventional thinking that these infections are too rapidly progressive for ED visits to be separated over a matter of days.
The most consistently abnormal triage vital signs were heart rate and respiratory rate, but only at 73% and 63%, respectively. Fewer patients in this study presented with fever or hypotension, which are often considered the classic features of bacterial infection and sepsis. The absence of fever at triage may falsely reassure clinicians about the probability of infection. Particular attention should be paid to older adults, who have more difficulty mounting a fever response, and may even present with hypothermia in the context of infection.Reference Mody, Schmader and Givens21 The quick sequential organ failure assessment (qSOFA) score,Reference Seymour, Liu and Iwashyna22 a more recent tool introduced in 2016 to screen for sepsis outside of the ICU, highlights the utility of tachypnea in detecting serious infections.
As with the vital signs, laboratory results were also highly variable among patients in this study; however, the CRP was consistently elevated in all patients in whom it was measured. In our ED, the CRP is the only laboratory value in the LRINEC score that is not listed in a checkbox on the order sheet, which explains its less frequent measurement. It is possible that the high mean CRP of 243 mg/L is inflated by the fact that it was ordered in individuals who appeared sicker.
We chose to extract the laboratory values comprising the LRINEC score, as, to the best of our knowledge, there are not more robust scoring systems for detecting invasive group A streptococcal infections, and we wanted an evidence-based rationale for the laboratory values studied. LRINEC scores were not consistently high risk in our sample of patients with confirmed necrotizing soft tissue infections, which is consistent with prior validation studies.Reference Liao, Lee, Su, Chuang and Wong23,Reference Neeki, Dong and Au24 The significant positive correlation between the LRINEC score and hospital length of stay more likely reflects the score's ability to detect advanced infections or patients with poorer baseline health status (e.g., pre-existing chronic kidney disease or anemia) who will naturally experience a longer recovery time, rather than a sensitive tool to detect all cases.
The observed incidence of invasive group A streptococcal infections in our sample was 2–4 times greater than the national rate. This is consistent with Public Health Ontario's Invasive Group A Streptococcal Disease in Ontario, 2016–2017 Seasonal Summary, which showed that Northwestern Ontario had the highest rate in the province, with an incidence of 60.1 and 41.7 per 100,000 in Northwestern Ontario and Thunder Bay, respectively.13 The mortality rate in our study (14%) was also higher than the provincial rate (10%) over the same time period. Our study showed an association between invasive group A streptococcal infections and diabetes mellitus and alcohol abuse, which is consistent with a large population-based surveillance study in Ontario.Reference Davies, McGeer and Schwartz14 It is crucial for ED clinicians to recognize these risk factors, given that the rates of these medical conditions are significantly higher in Northwestern Ontario compared with the provincial average. From a public health standpoint, Northwestern Ontario would benefit from improved access to primary health care and more robust upstream preventative strategies, particularly for diabetes and alcohol abuse.25
Future research should focus on developing a more sensitive clinical tool for identifying invasive group A streptococcal infections early, whether it be through a clinical decision rule that takes into account patients’ risk factors or the bacteria's virulence factors. Regions with a high incidence of invasive group A streptococcal disease should consider a follow-up appointment the next day for high-risk patients who are suspected to only have a simple infection at the time of discharge, a mandatory call-back for any wound cultures that grow Streptococcus pyogenes, and other center-dependent methods of close follow-up. Once a necrotizing soft tissue infection is suspected, emergency physicians should forego imaging and focus on obtaining surgical intervention with the same expediency as they do for obtaining angioplasty for ST-elevation myocardial infarctions and thrombolytic therapy for acute ischemic strokes.
There were several limitations to this study. The biggest limitation was a lack of a comparison group, thus limiting the conclusions that can be drawn about this sample relative to the general population. Median LRINEC scores in our cohort did not suggest a high risk for necrotizing fasciitis in the majority of patients with culture-proven invasive disease; however, eight of these patients were missing a CRP. The data were retrospectively gathered and identified using ICD-10 codes; it is possible that some cases were missed due to improper coding or concomitant diagnoses. We also likely missed cases where cultures were taken after antibiotic administration or not done at all. We excluded cases that first presented to another hospital, even if they were transferred to our center, as we did not have electronic access to all the details of their initial presentation. Some of the data that we wanted to extract, particularly immunization status and MRSA colonization, was unknown in many patients. Regretfully, we did not collect data on imaging rates or operating room visits. The triage respiratory rate and oxygen saturation were not recorded in one very sick patient, and CTAS score was missing in three patients, which may have skewed our analysis in this small sample.
The overall clinical implication from this study is that the clinician's assessment must override objective values such as triage vital signs, laboratory values, and scoring systems when invasive group A streptococcal infections are suspected. The heart rate and respiratory rate were the most commonly abnormal triage vital signs, but only in 73% and 63% of cases, respectively. The CRP was the only laboratory value that was consistently, yet variably, elevated when measured in this small sample size. The LRINEC score was moderate or high-risk in 68% of culture-confirmed necrotizing soft tissue infections. Emergency physicians should be aware of the risk factors for invasive group A streptococcal infections, including diabetes mellitus and alcohol and drug misuse, and promptly obtain surgical consultation when there is clinical suspicion of a necrotizing soft tissue infection.
CONCLUSION
Despite its morbidity and mortality, invasive group A streptococcal infections often present insidiously in adult patients with only mild tachycardia and tachypnea at triage. The CRP was the most consistently abnormal laboratory investigation in patients with invasive group A Streptococcus, and should be ordered when this disease process is suspected. Emergency physicians should be vigilant about the possibility of this disease in high-risk populations such as patients with diabetes mellitus and those who misuse alcohol and drugs.
Supplemental material
The supplemental material for this article can be found at https://doi.org/10.1017/cem.2019.457.
Acknowledgements
The authors thank Dr. Holly Ann Garnett for the statistical analysis and Dr. David Savage for his feedback on the manuscript.
Competing interests
None declared.







