CLINICIAN'S CAPSULE
What is known about the topic?
Legalization of non-medical cannabis may impact the volume of cannabis-related emergency department (ED) visits and may alter historical co-diagnoses patterns.
What did this study ask?
What was the impact of national non-medical cannabis legalization in urban Alberta on cannabis-related ED visit volume and co-diagnoses patterns?
What did this study find?
Urban cannabis-related visits increased 45%, though for individual EDs, average increase was 3.1 visits per ED per month.
Why does this study matter to clinicians?
Clinicians in other provinces and countries considering non-medical cannabis legalization should not expect alarming changes in cannabis-related ED visit volume.
INTRODUCTION
On October 17, 2018, Bill C-45 made non-medical cannabis possession, consumption, and sale legal for Canadian adults. While widespread cannabis use existed among Canadians prior to legalization, there has been concern over whether this policy change may increase health harms, including emergency department (ED) volumes and presentation patterns.Reference Fischer, Rehm and Crépault1,2 Previous research has identified cannabis-related ED visit monitoring important, among many public health impact indicators for non-medical cannabis liberalization.Reference Lake, Kerr and Werb3 To minimize potential negative impacts of legalization on health services and public health, cannabis sales in Canada are strictly regulated both federally and provincially. For example, unlike the United States, advertising and promotions are forbidden in Canada, with cannabis requiring plain packaging and health warning labels. In Alberta, cannabis distribution and online sales are regulated by a provincial government agency, the Alberta Gaming, Liquor, and Cannabis Commission, which also oversees private retail outlet licensing. Alberta provides good context for researching the early impacts of legal cannabis on ED visits, as it has been the first Canadian province to implement and rapidly scale up legal cannabis sales, with 176 of Canada's 407 cannabis stores, and $195 million dollars in sales.4
Although cannabis is often associated with fewer acute harms when compared to substances like alcohol, tobacco, or opiates, short-term use is associated with paranoia, anxiety, suicidal ideation, psychosis, and impairment of memory, motor coordination, and judgement.Reference Volkow, Baler, Compton and Weiss5,Reference Karila, Roux and Rolland6 Cannabis can also induce temporary tachycardia and cannabinoid hyperemesis syndrome, or onset of cyclical emesis in chronic users.Reference Galli, Sawaya and Friedenberg7–Reference Hasin, Saha and Kerridge9 Because cannabis can have differing effects on new and chronic users, it is necessary to examine co-diagnoses alterations in cannabis-involved patients to determine whether patient populations have changed. While Canada remains the first North American country to nationally legalize cannabis, several American states with legalized non-medical cannabis have identified temporary changes in cannabis use associated with co-diagnoses patterns and cannabis-related ED presentations.Reference Hall, Monte and Chang10 Cannabis-related ED visits appear to be increasing across the United States, with the Drug Abuse Warning Network reporting a 49% increase.Reference Zhu and Wu11 Legalization appears to have added a small, additional ED caseload, with Colorado reporting a 23% increase in cannabis-related ED visits on top of nationally reported visitation increase.Reference Kim and Monte12
To answer the overarching question of what impact cannabis legalization has had on EDs, we established two objectives. These were to 1) identify change in cannabis-related ED visit, telehealth, and poison control call volume; and 2) identify changes in cannabis-related co-diagnoses patterns in urban Alberta EDs pre- and post-legalization.
METHODS
Study design and data collection
This study involved analyses of administrative data pre- and post-legalization. Data were extracted from the National Ambulatory Care Reporting System (NACRS), the Alberta Poison and Drug Information Service, and HealthLink provincial databases. NACRS data for Alberta are among the highest-quality in Canada, as Alberta is among two provinces mandating full abstraction of all ED visits, ensuring no patients or their physician-made diagnoses are missed.13 The Alberta Poison and Drug Information Service is the provincial poison control service, available to both physicians and the public, and HealthLink is the public provincial telehealth service. Both provide telephone health advice to Albertans. ED data were obtained from October 1, 2013, to July 31, 2019; poison control data were obtained from May 1, 2016, to July 31, 2019; and HealthLink data were obtained from June 1, 2017, to July 31, 2019. Earlier data were unavailable from HealthLink or poison control. Data were split into annual quarters aligning with population estimates published by the Government of Alberta. Thus, the post-legalization period was defined as presentations from October 1, 2018, to July 31, 2019.
All data were collected from urban Alberta, defined as 14 Calgary and Edmonton area ED, inclusive of St. Albert and Sherwood Park, given their proximity to Edmonton. HealthLink and poison control data were collected province-wide, due to an inability to verify caller location. The study was approved by the University of Calgary research ethics board (REB19-0238).
Population
Eligible patients included those with a cannabis-related International Classification of Disease (ICD) code in primary or secondary diagnostic fields. The database did not allow differentiation between those reportedly using cannabinoids for medicinal use and those using cannabis for non-medicinal use. ICD was used to identify injuries and causes. Results were stratified by age, broken into 0–14 (child), 15–17 (adolescent), 18–24 (young adult), 25–44 (adult), 45–64 (older adult), and 65+ (senior). ICD codes used included all mental and behavioural disorders due to cannabinoid use and cannabinoid poisonings. Hyperemesis was defined as vomiting paired with a cannabinoid code (no ICD code exists for cannabinoid hyperemesis syndrome; thus, it is necessary to combine codes). From patient data, we obtained ED visit date, age, sex, previous cannabis-related presentations, and hospital admission status. Co-ingestants were also identified using ICD codes. A full list of ICD codes used is available in Supplemental Table 1. Cannabis-related calls to HealthLink and poison control were identified by identifying keywords “marijuana,” “cannabis,” or “cannabinoid” in the call or substance description. A co-diagnoses analysis was not conducted on calls due to ICD code absence.
Data analysis and outcomes
To determine whether significant changes occurred in overall volume, we conducted an interrupted time-series analysis via a segmented simple linear regression for volumes pre- and post-legalization within the ED, poison control, and HealthLink data sets. Monthly total call or visit volumes were analysed for all data sources. Due to the relatively short post-legalization period, we did not have enough data to reliably estimate a slope. Therefore, we estimated a common slope in the pre- and post-legalization periods and a level change at the time of legalization. A visual assessment did not reveal serial autocorrelation or seasonal trends in any time series. Secondly, we calculated incidence rate ratios (IRRs) to compare changes in presentation rate and diagnosis patterns for the entire urban Alberta population between the pre-legalization period and post-legalization period. Because interrupted time-series analysis accounts for pre-existing trends, we based conclusions about volume on the interrupted time-series rather than the IRR.
We also calculated relative-risk ratios (RRs) to compare changes in the proportion of cannabis-related ED visits that had different co-diagnoses pre- and post-legalization. The IRR allows for identification of changes in incident rate when compared against the entire Alberta population, whereas the RR allows for identification of changes among individuals who present to the ED. Both the IRR and RR were calculated using Wald confidence intervals (CIs) via the epi2by2 command in R through the epiR package, with the population of urban Alberta and the number of cannabis-related ED visits used as denominators, respectively.
Individuals missing data for a variable were omitted from the analysis of that variable, though only one case of missing data was identified. As the data were from an electronic database, it was difficult to identify whether data were missing elsewhere in the data set. All rates were adjusted to the 2019 third-quarter Alberta population to account for population growth. Ninety-five percent CIs were calculated. Analysis occurred in R version 3.6.1.
RESULTS
Characteristics of cannabis-related ED visits
The sample, described in Table 1, included 14,732 cannabis-related presentations, of which 64.9% were male. Mean age was 28.5 (SD ± 12.2). We observed a mean of 45.1 patients presenting per week to the ED pre-legalization, and 68.9 patients presenting post-legalization. The most common co-ingestants were alcohol, cocaine, and other stimulants (Supplementary Table 1). The most common psychological diagnoses were for anxiety-related, personality and behavioural, affective mood, and non-mood psychotic disorders. Hyperemesis (12.2%) and external injury (18.1%) were also common. Cardiac and respiratory distress was also frequent, including heartbeat and blood pressure abnormalities, cough, and pain in the throat or chest (Supplementary Table 1).
Table 1. Demographics and clinical characteristics of cannabis-related ED visits
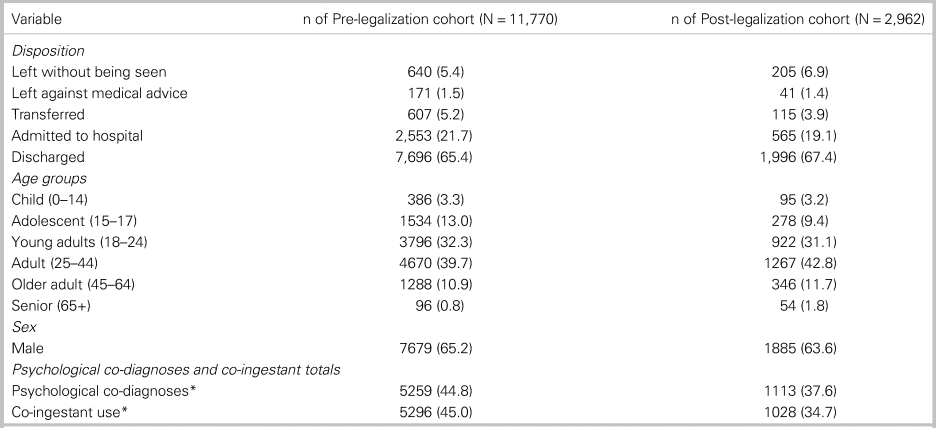
*Expanded upon in Supplemental Table 1.
Volume analysis
Cannabis-related visit volume increased post-legalization within urban EDs (IRR 1.45, 95% CI; 1.39, 1.51) with the interrupted time-series indicating a change of 43.5 visits per month (95% CI; 26.5, 60.4). Calls to poison control also increased (IRR 1.87, 95% CI; 1.55, 2.24), with the interrupted time-series indicating a change of 4.02 calls per month (95% CI; 0.11, 7.94). Changes for individual EDs varied between -11.5 and 12.6 visits per month, with an average of 3.1. HealthLink did not receive a significant increase in cannabis-related calls post-legalization. Interrupted time-series results are within Table 2 and illustrated in Figure 1, Figure 2, and Supplemental Figure 3. As indicated in Table 2, the IRR for cannabis-related presentations was 1.45 (95% CI; 1.39, 1.51) or a 45% increase from 20.7 ED visits per 100,000 person-years to 30.1. Of all cannabis-related visits, 15.1% were due to unintentional exposure. Unintentional exposures grew overall for all groups with the exception of seniors, and grew proportionally for all age groups with the exception of children and seniors.
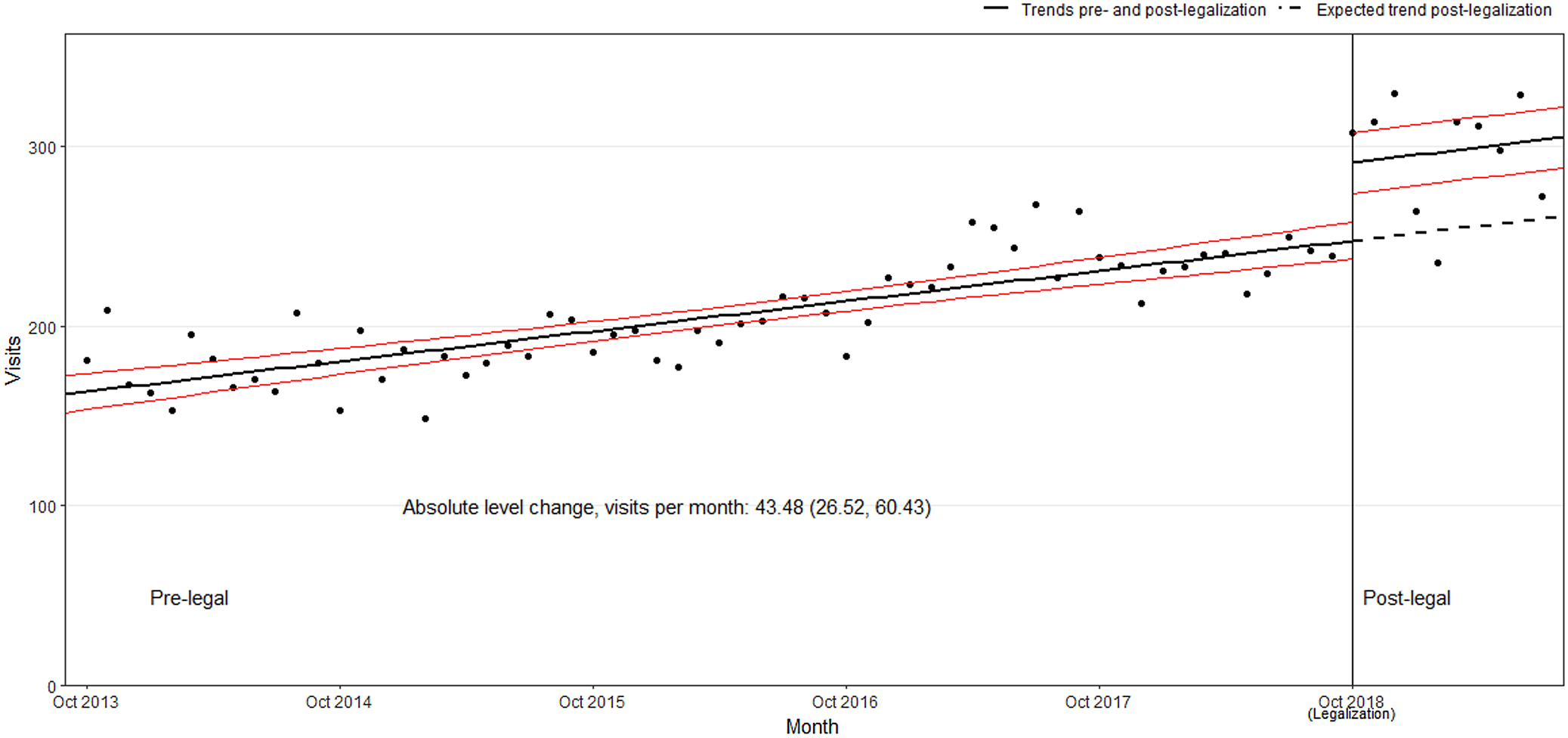
Figure 1. Urban emergency department cannabis-related visits over time.
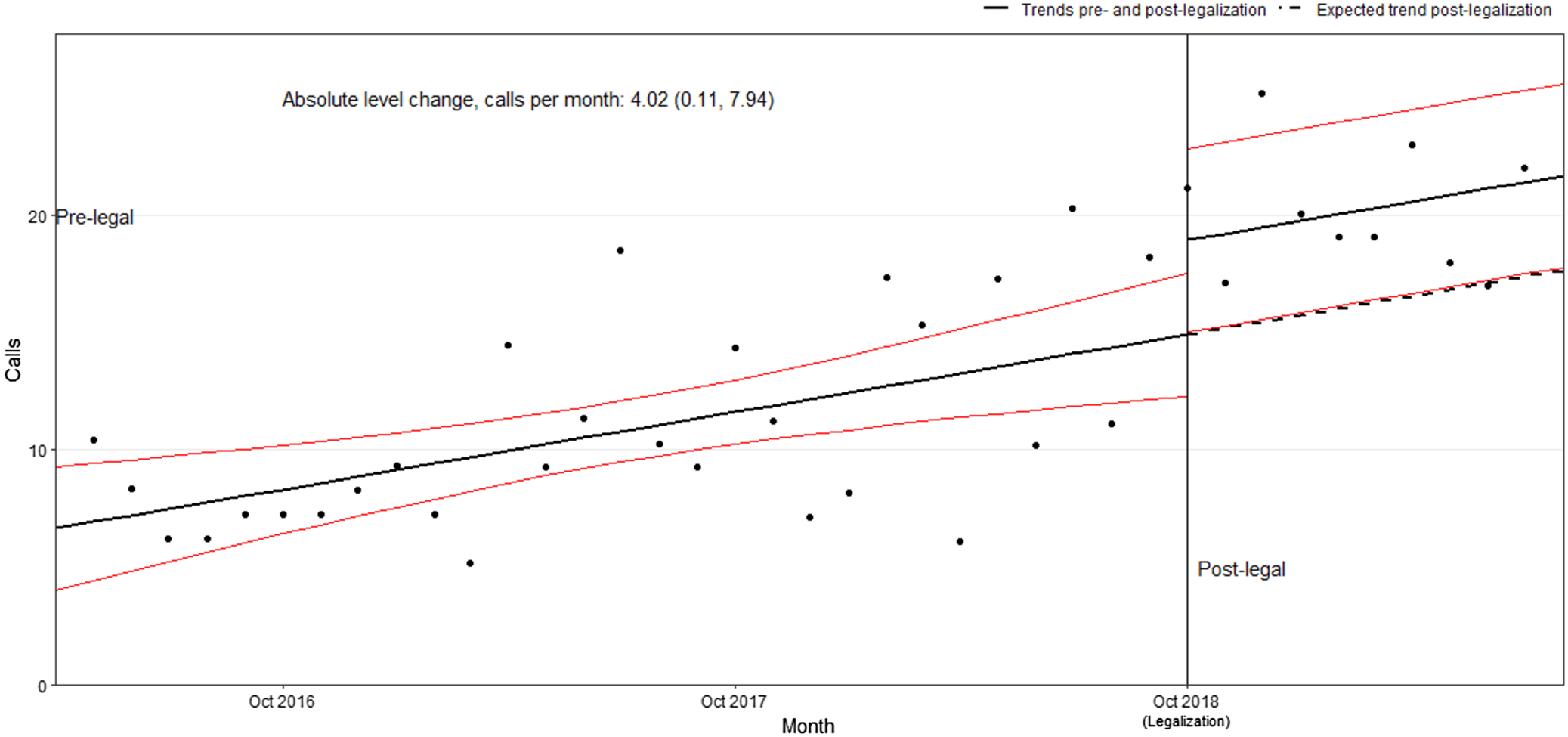
Figure 2. PADIS cannabis-related calls over time.
Table 2. Comparison of volumes pre- and post-legalization via interrupted time series and incidence rate ratio (IRR) analyses
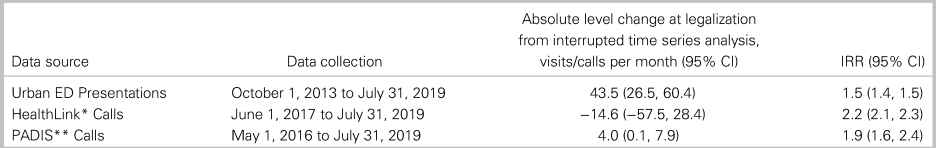
*HealthLink is the public telehealth information service in Alberta.
**PADIS is the public poison control service in Alberta.
Presentation pattern and co-ingestant use analysis
Ratios comparing the number and makeup of pre- and post-legalization cannabis presentations are described in Table 3. When observing the post-legalization period, individuals presenting with cognitive disorder symptoms (32%), cardiac distress (71%), and hyperemesis (23%) increased relative to overall cannabis-related presentations. The increase in cardiac distress-related presentations was led by younger adults (RR 2.7, 95% CI; 1.7, 4.2) and adults (RR 2.4, 95% CI; 1.5, 3.8). An increase was also observed in external injuries associated with cannabis (39%). We found decreases in several psychiatric co-diagnoses, including non-mood psychotic (-21%), mood-related (-30%), personality and adult behavioural (-25%), and anxiety-related disorders (-14%). Patient disposition remained similar throughout the study period, though we noted an increase in the proportion of patients who left the ED prior to treatment (28%), and a decrease in individuals admitted to hospital proportional to the cannabis-related presentation total (-12%).
Table 3. Incidence rate ratios (IRRs) and relative-risk ratios (RRs) comparing pre- and post-legalization ED visits

*Inhalants and nicotine excluded due to low sample size.
With respect to co-ingestants, a decrease in the proportion of individuals reporting co-ingestant consumption overall was found (-23%) with statistical significance identified for cocaine (-42%), alcohol (-24%), stimulants (-16%), opiates (-31%), and unclassified drugs (-32%) (see Table 3).
With respect to age group differences, we identified increased visitation among all age groups, though increased visitation was particularly pronounced in individuals over age 45 (see Table 3). Incident rates climbed overall, as expected, given the 45% increase in patient volume.
DISCUSSION
This is the first study reporting on ED impacts of national cannabis legalization, using a national high-quality standardized database. Our research in a province with rapidly scaled up cannabis sales may help inform future global policies surrounding cannabis legalization, and may help advise the global emergency medicine community on the impacts of cannabis legalization.
Interpretation of findings
Volume analysis of ED visits and calls to telehealth services
Interrupted time-series analyses suggest that, overall, cannabis legalization led to a statistically significant increase in ED visits and poison control calls. The increase in ED visits and poison control calls is similar to changes observed in the United States.Reference Kim and Monte12–16 We hypothesize increased visitation steams from increased cannabis use following legalization and increased social acceptability, leading to more individuals seeking help for cannabis-related health issues or reporting cannabis use. Though it is possible existing cannabis users are now consuming more cannabis than previously, we believe the increase in cannabis-related visits is due to new users. The difference in individuals who have visited the ED for a cannabis-related event in the past 5 years was less than 1% when comparing the pre-legalization and post-legalization periods.
Cannabis-related harm patterns and co-ingestant use analysis
The IRR analysis indicated an increase in the majority of diagnosis categories, likely due to increased overall cannabis-related visits mentioned previously. However, the RRs tell a very different story, with fewer comorbidities identified post-legalization per cannabis-related visit. Per cannabis visit, decreases were observed in all psychological co-diagnoses and in the majority of co-ingestant categories. We hypothesize decreasing co-ingestant and psychological co-diagnoses presentation to stem from a changing patient population involving new users purchasing cannabis due to availability and legality. New users may not be aware of cannabis’ physical effects, increasing the visit proportion for physical co-diagnoses and decreasing the proportion for psychological co-diagnoses. This trend may also be responsible for fewer admittances and more discharges post-legalization. We attribute the lower proportion of individuals reporting co-ingestant use to public health campaigns highlighting poly-substance use dangers and the poor availability of other co-ingestants.
Additionally, we note increases in cannabis-related physical co-diagnoses, including hyperemesis and cardiac distress, in addition to increases in unintentional ingestion and accidental external injury. The increase in cardiac distress symptoms appears to be associated with the increase in new users unfamiliar with the effects of cannabis, particularly among younger adults. Similarly, the increase in unintentional ingestions is led by adults and older adults, though the incidence rate of children and adolescent presentations has also increased. We hypothesize these trends to stem from increased usage among older adults, possibly for self-medication and because of the presence of cannabis belonging to a younger member of the household.
Contextualizing results
Overall, cannabis-related harm remains a very small subset of urban ED visits, with approximately 3 visits per 1,000 attributable to cannabis. Though this figure indicates ED visits related to cannabis may be greater in comparison to some prescription drugs, the substance is associated with fewer ED visits in comparison with other common substances like alcohol and opiates.Reference O'Connor, Grywacheski and Louie14,Reference Myran, Chen, Giesbrecht and Rees15
LIMITATIONS
Inherent to administrative data use is the possibility of miscoded patients. Additionally, it is likely that cannabis legalization has altered stigma and patient fears of legal repercussions. Though cannabis use is likely underreported within administrative data and during ED visitation, particularly pre-legalization, the National Ambulatory Care Reporting System remains the only nationally standardized ED database reflecting an internationally recognized coding scheme for ED visitation.16 Conducting more invasive testing, particularly on past patients, is simply not tenable. Additionally, it is not known how often providers contact poison control for cannabis-related inquiries. Our methodology remains similar to other studies examining ED cannabis impacts.17
Clinical implications
The study has identified significant increase in cannabis-related ED visit volume subsequent to cannabis legalization. However, when considering actual clinical implications for individual sites, the daily impact of cannabis-legalization remains low, with the greatest increase in mean monthly presentation rate for an individual ED at 12.6 visits. Clinicians should remain vigilant of increasing unintentional exposures, particularly among older adults, given potentially more serious harms. Clinicians should also remain vigilant of cannabinoid hyperemesis syndrome, with increasing prevalence within the general population and as a proportion of cannabis-related ED presentations.
Research implications
Given the rapidly changing nature of Canadian cannabis legislation, cannabis-use levels will continue to change. It is important that similar studies and monitoring continue across the country over an extended period. Lastly, our results have indicated an increase in accidental cannabis ingestion in those ages 15–64. Future research and policy may wish to target those populations with educational interventions to reduce harm, like accidental ingestion.
CONCLUSION
Overall, results show that cannabis legalization is associated with an increase in cannabis-related ED presentations, with a marked increase in older adults. However, the overall impact of early stage legalization on ED operation remains low, with limited volume increase for individual sites. Results also indicate that most co-diagnoses patterns have remained stable or declined, as is the case for psychological co-diagnoses. Notably, increases in some physical manifestations were observed. Nonetheless, rising accidental ingestions remain concerning and should be targeted for prevention.
Supplementary material
The supplemental material for this article can be found at https://doi.org/10.1017/cem.2020.384.
Acknowledgements
We would like to thank PADIS and HealthLink data analysts for their assistance in sourcing data from their respective organizations. We would also like to thank analysts with the Alberta Health Services Strategy for Patient Oriented Research data platform for their assistance in retrospective data collection.
Financial support
MEMY was supported through an Alberta Health Services Emergency Strategic Clinical Network summer studentship grant for this research.
Competing interests
None declared.







