CLINICIAN’S CAPSULE
What is known about the topic?
Little is known about the outcomes of older patients who are classified as “low acuity” at triage.
What did this study ask?
What are the differences in outcome of ED patients ages 65 years and older who received a CTAS score of 4 or 5, compared with patients 40 to 55 years old.
What did this study find?
Older patients were significantly more likely to be admitted; patients aged 85 years and older were particularly at risk.
Why does this study matter to clinicians?
Consideration should be given to triage modifiers for age, given the higher admission and re-presentation rates in older patients.
INTRODUCTION
Older patients, commonly defined in the literature as those who are ages 65 years and older, currently account for 24% of emergency department (ED) visits. 1 This group is expected to alter ED capacity and care because older patients comprise an increasing proportion of the population. 1 , 2 These patients have higher ED visit numbers, longer lengths of stay in the department, and higher hospital admission rates than younger patients.Reference Biber, Bail and Sieber 3 , Reference Lowthian, Curtis and Stoelwinder 4 One-third to one-half of elderly patients will present again to the ED within 90 days of their discharge, and these patients are at a higher risk of functional decline and death following an ED visit.Reference Friedmann, Jin and Karrison 5 , Reference Pines, Mullins and Cooper 6 The national issue of ED overcrowding has led to a number of attempted solutions to improve patient flow through the department, including “fast track” or minor treatment areas for less urgent issues.Reference Affleck, Parks and Drummond 7 Although it is well documented that overall older ED patients are at increased risk of adverse outcomes, there is a paucity of literature addressing the subset of elderly patients triaged to these low acuity areas of the ED.Reference Biber, Bail and Sieber 3 - Reference Pines, Mullins and Cooper 6
The Canadian Triage and Acuity Scale (CTAS) is a widely used five-level scale to rapidly assess and triage ED patients in terms of urgency of their presenting complaint.Reference Murray, Bullard and Grafstein 8 Most research indicates that the CTAS criteria are reliable and predict the need for immediate life-saving intervention, including in elderly patients.Reference Lee, Oh and Peck 9 , Reference Mirhaghi, Heydari, Mazlom and Ebrahimi 10 However, some studies indicate that elderly trauma patients are under-triaged, and authors have suggested that specific geriatric triage criteria are more sensitive than standard triage algorithms.Reference Platts-Mills, Travers and Biese 11 - Reference Lin and Worster 14 Of the frail elderly patients who are labeled on triage as having “failure to cope,” one-half had an acute medical issue and one-quarter were under-triaged.Reference Rutschmann, Chevalley and Zumwald 15 In addition, elderly patients who frequently visit the ED may be assigned less acute triage scores compared with those patients who present less often.Reference Wajnberg, Hwang, Torres and Yang 16 There is no specific age-related modifier in the CTAS or Emergency Severity Index guidelines, although many elderly patients present with problems of proportionately greater urgency than younger patients.Reference Murray, Bullard and Grafstein 8 , Reference Gilboy, Tanabe, Travers and Rosenau 17 , Reference Aminzadeh and Dalziel 18 In two Canadian studies, approximately 5% of elderly patients who received a less urgent CTAS score of 4-5 were admitted to the hospital following their ED visit, whereas another study in South Korea, where admission patterns may differ from Canadian practices, found that nearly 20% of older patients triaged as CTAS 4 were admitted.Reference Lee, Oh and Peck 9 , Reference Latham and Ackroyd-Stolarz 19 , Reference Quinn, Herman and Lin 20 For reference, CTAS guidelines that indicate time to initial patient assessment by a physician should be 1 hour for CTAS 4 patients, whereas CTAS 5 patients should be assessed within 2 hours. CTAS 4 and 5 scores encompass a wide scope of problems such as minor fracture, stable minor head injury, and moderate abdominal pain with normal vital signs.Reference Murray, Bullard and Grafstein 8 Admission rates to Canadian hospitals for patients of all ages with a CTAS score of 4 to 5 range from 1% to 2%. 21
Although the existing literature thus indicates that older ED patients are a high-risk population for adverse outcomes after an ED visit, little is known specifically about older patients who present with issues that are initially classified as less acute. Our study aimed to describe the cohort of older patients who present to the ED with complaints felt to be of low acuity, many of whom are currently triaged to ambulatory care areas, and to assess their outcomes in comparison with a younger cohort. In particular, we wanted to evaluate the characteristics of older patients assigned a CTAS score of 4 to 5, describe their course in the ED, including the extent of workup and management, and assess their disposition and short-term outcomes.
METHODS
Study design and setting
This study was a health records review of patients seen at two large urban Canadian EDs between July and August 2015. These EDs are both academic centres with a combined annual census of nearly 175,000 visits. The single Research Ethics Board for both hospitals reviewed and approved the study protocol prior to the commencement of data collection.
Subjects
Included patients were those with CTAS scores of 4 or 5 at triage. For the older cohort, 350 charts from patients ages 65 years and older within the pre-specified period were provided to the data extractors at random by the hospital’s Data Warehouse, whereas 150 charts of patients ages 40 to 55 years were selected in the same fashion and reviewed as a control group. Patients who were assigned a CTAS score of 4 or 5 but who were never seen by an emergency physician, that is, those who were to be seen by another service directly in the ED or who left without being seen were excluded from a full data collection.
Data collection
Data abstractors were trained in the use of online scanned hospital documentation and familiarized with the use of the data report form, but were not blinded to study objectives. One trained reviewer assessed all charts and abstracted patient information using a standardized data form. Documents examined for an index visit included triage and nursing notes, ED records of treatment, and any consultation or admission notes generated during that ED visit. All documents, including subsequent ED triage notes and records of treatment, consultation notes, and nursing records within the 14-day period after the index ED visit were reviewed to assess 14-day outcomes. Fourteen-day outcomes were chosen as a means to assess short-term outcomes that would be more likely to represent an ED revisit or hospital admission for the same issues as the initial ED visit. To achieve inter-rater reliability, 20% of the total charts (the middle 10% of both the older and control cohorts) were reviewed by a second trained reviewer using the same data form. Five episodes of disagreement occurred due to differences in interpreting handwriting on the records of treatment and were resolved by discussion and consensus.
Outcome measures
Data collected included 1) patient demographics, including presenting complaints, comorbidities, and percentage of patients with a family physician listed; 2) ED visit information, including the location of triage and total length of stay; 3) testing and interventions performed in the ED, consultation rates, and rates of re-triage to a more acute area of the ED; and 4) disposition information following the index visit, as well as revisits and admissions to the hospital within 14 days.
Retrospective CTAS scoring
After a review of the patient’s ED triage documentation only, one physician reviewer who was trained in CTAS scoring assigned a retrospective CTAS score to each patient. When disagreement existed between the nurse-assigned triage CTAS score and the retrospectively applied score, a second trained physician reviewer was consulted to reach consensus based on CTAS guidelines and the available information.
Statistical analysis
Data were analysed descriptively and analytically to evaluate patient demographics, ED visit information, and 14-day outcomes. Means with standard deviations and proportions with confidence intervals (CI) were used for continuous and categorical variables, respectively. The analysis for patients ages 65 years and older also included a pre-planned stratified analysis of patients ages 65 to 74 years, 75 to 84 years, and those ages 85 years and older. Chi-square tests were used to assess differences in testing, treatment, and disposition between controls and older groups, as well as among age strata, with significance being attributed to a p level of<0.05. For retrospective CTAS scoring, comparisons were made between the older patients’ assigned CTAS scores and their retrospectively applied ones, including kappa statistics to evaluate inter-observer reliability.
RESULTS
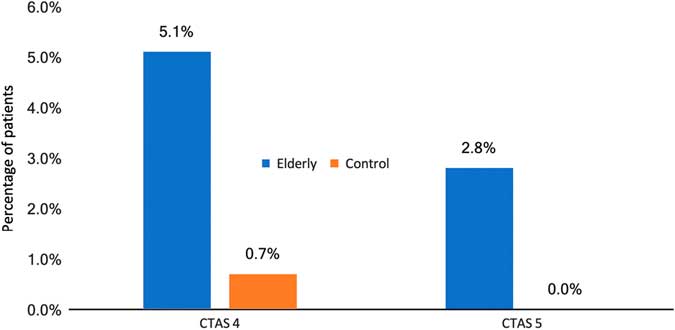
The hospital’s Data Warehouse provided the sample of patients who met the inclusion criteria for either the older or the control cohort groups. Of these, 529 patients were screened and 29 patients were excluded after their charts were reviewed based on reasons outlined in Figure 1, leaving 350 patients in the older cohort and 150 in the control group.
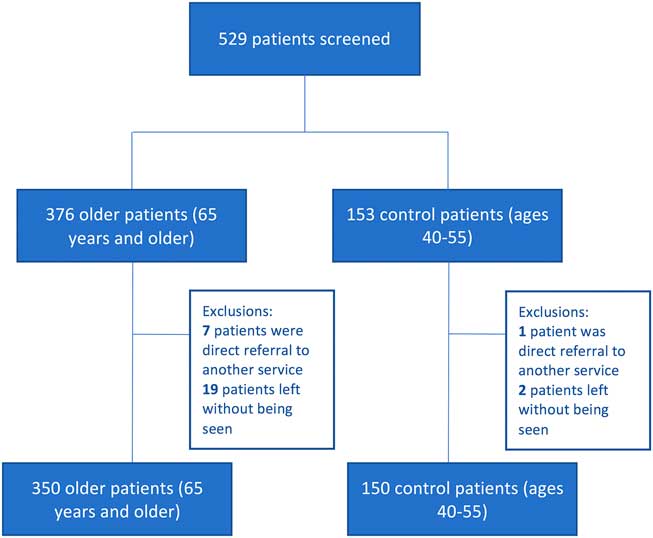
Figure 1 Flow diagram of all patients screened.
The average age of the older cohort was 76.5 years (range 65-100), whereas the control group of 40- to 55-year-olds had a mean age of 47.3 years (Table 1). The most common reasons for an ED visit in both groups were extremity injury or pain, rashes, and lacerations or bites. The majority of both groups received CTAS scores of 4 on arrival (89.7% older, 96% control). Most patients were triaged to the ambulatory care area of the ED (88.6% older, 99.3% control). In the older cohort, 11% of patients were triaged to a non-monitored stretcher area. One older patient was brought to the acute monitored area in the department because he was on a backboard from emergency medical services (EMS) after a fall. Abnormal triage vitals in both populations were rare, with the most common abnormality being tachycardia (2.9% older v. 6.7% controls).
Table 1 Characteristics of the older versus control cohorts

Table 2 describes investigations performed and patient management in the ED. Consulting services were involved in the management of 13.4% of the older group and 6.7% of the controls. The Geriatric Emergency Management team, a specialized nursing team designed to assess elderly patients whose disposition plan is to home, saw 26 (7.4%) of the older patients. Six patients (1.7%) in the older group were re-triaged to a more acute area of the ED from the ambulatory care area during their ED encounter: four to facilitate pain management and consultation in the ED, and two for a monitored bed. Most discharge diagnoses in both groups were soft tissue injuries (22.3% older v. 24.7% control), fractures (8.6% older v. 6.7% control), and cellulitis or abscess (12.0% older v. 12.7% control).
Table 2 ED data for the older and younger cohorts
CCAC=Community Care Access Centre (organizes outpatient intravenous antibiotic therapy and medications, as well as home care supports); GEM=Geriatric Emergency Medicine nursing (provides an in-depth assessment and recommendations for those patients who are felt to be safe for discharge home but could benefit from a review of geriatric-specific issues [e.g., falls, memory, mobility]); NYD=not yet diagnosed; URTI=upper respiratory tract infection
Table 3 outlines patient disposition and 14-day outcomes. The older cohort was significantly more likely to be admitted to the hospital (5.1% v. 0.6%, p=0.016). Discharge home from the ED occurred in 94.9% of the older group (84.3% to home, and 10.6% to retirement or nursing home) versus 99.3% of the younger controls. One patient in the older cohort was admitted to an acute monitored setting for congestive heart failure; the remainder of admitted patients went to non-monitored ward beds. In the older group, more CTAS 4 patients (5.4%) than CTAS 5 patients (2.8%) were admitted, but this was not significant (p=0.46, Figure 2). There was a non-significant trend towards increased ED revisit rates in the older group at 14 days (13.7% v. 8.7%, p=0.11). Among the older population, the presenting complaint on ED revisit was the same as the initial visit in 60.4% of cases, with 79.2% of revisits being related to the initial ED visit. The most common reasons for an ED revisit in the older group were skin complaints such as cellulitis, rash or laceration (37.5%), soft tissue injury (10.4%), and falls or weakness (12.5%). In the younger group, most re-presentations to the ED were for skin conditions (30.8%), mental health (15.4%), and extremity pain (15.4%). Fourteen-day hospital admission rates were significantly higher in the older cohort (4.0% v. 0.7%, p=0.045; Figure 3). The unweighted kappa value for inter-rater reliability of CTAS in the older group was 0.79 (95% CI, 0.68-0.89). One patient who was admitted to the hospital on an index visit and received a nurse-assigned triage score of 5 was retrospectively assigned a CTAS score of 4; in all other cases, the patients (94.4%) for whom there was disagreement on CTAS scores were discharged.
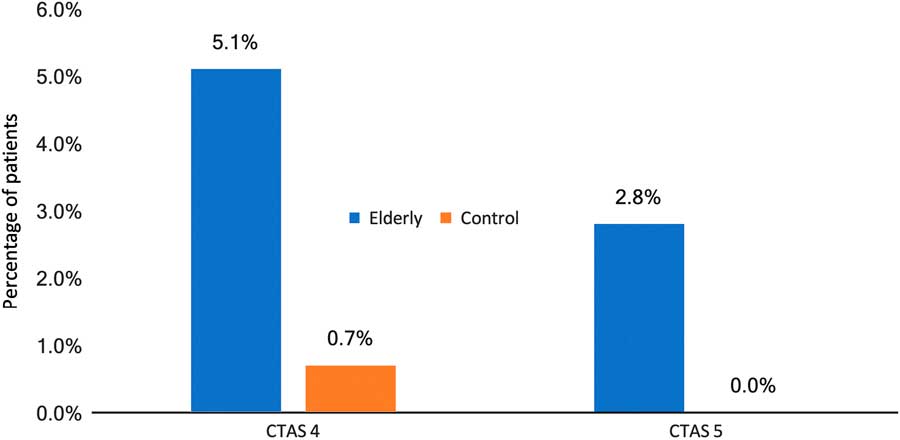
Figure 2 Admission rates on the index visit by CTAS score.
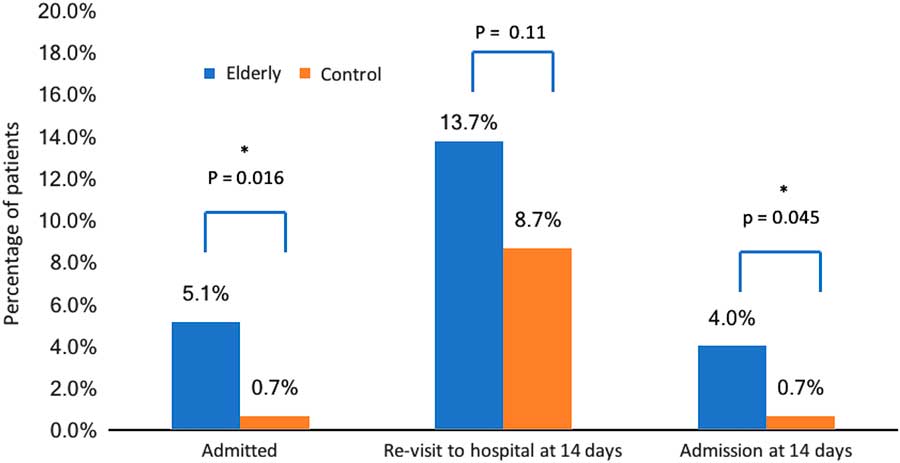
Figure 3 Disposition data of elderly versus control patients.
Table 3 Disposition and 14-day follow-up outcomes of older and younger cohorts
AMA=acute monitoring area; ICU=intensive care unit; NH/RH=nursing/retirement home.
In the subgroup analysis of the older cohort, 23% of patients were ages 85 years or older, and 65% of this “very elderly” group were female. Table 4 demonstrates that the very elderly group was more likely to arrive by ambulance (32.0% v. 6.8% for ages 65-74 and 11.0% for ages 75-84, p<0.001). This group (35.4%) had more bloodwork performed than those ages 65-74 (19.8%) or 75-84 (25.7%, p=0.03) and was more likely to undergo a computed tomography (CT) scan (19.0% v. 6.8% for ages 65-74 years, v. 8.3% for ages 75-84 years, p=0.02). They were also more likely to be admitted to the hospital (8.9%) than those ages 65 to 74 (1.85%) or 75 to 84 years (7.3%, p=0.03). Finally, although 14-day ED revisit rates were not significantly different by age strata (13.0%, 65-74; 11.0%, 75-84; 19.0%, 85 and over; p=0.29), admission rates at 14 days were higher again in the very elderly group (11.4% v. 0.6%, 65-74 v. 3.7%, 75-84, p<0.001).
Table 4 Subgroup comparison of older patient workup and outcomes
CT=computed tomography; ED=emergency department; EMS=emergency medical services; GEM=Geriatric Emergency Medicine.
DISCUSSION
This study assessed the outcomes of older patients who were assigned a “less urgent” ED triage score and compared them with younger control patients. The older patients had a higher number of medical comorbidities, but most of this older group still was living independently and ambulatory prior to presentation. Both groups presented with similar, seemingly low acuity triage complaints such as dermatologic and musculoskeletal issues, and most were triaged to an ambulatory care area. However, the intensity of workup and admission rates was higher in the older cohort. The older group was also more likely to revisit the ED for the same reason as index presentation and be admitted to the hospital within 14 days. The primary driver of this increased admission rate and revisit rate was the very elderly group ages 85 years and older.
The admission rate in our study of 5.1% for all older patients and 8.9% for the very elderly subgroup is much higher than national average for CTAS 4-5 patients, which estimates a 1% to 2% admission rate overall. 21 Other Canadian studies of older patients, although they did not specifically assess only low acuity triage patients, have also found that admission rates for older CTAS 4-5 patients are 4% to 6%.Reference Latham and Ackroyd-Stolarz 19 , Reference Quinn, Herman and Lin 20 One Korean study found a 19% admission rate among elderly patients assigned a CTAS 4 triage score.Reference Lee, Oh and Peck 9 A recent Canadian study found that age over 65 years was a strong predictor of admission to the hospital among CTAS 5 patients.Reference Lin and Worster 14 Collectively, these studies support our finding that admission rates to the hospital, even among low acuity older patients with benign-sounding presenting complaints, far exceed admissions for younger patients.
Strengths of our study include its specific focus on older patients assigned a low acuity triage score and its comparison with a younger control cohort. Previous studies have assessed CTAS validity and outcomes among older patients with CTAS scores of 1-5, but our research question directly addresses those older patients with CTAS scores of 4-5, many of whom are triaged to an ambulatory care area. Our pre-specified analysis of outcomes based on age strata provided the important information that the very elderly group of age 85 years and older require more resources in ED workup, are admitted more frequently to the hospital, and are at higher risk of ED re-presentation and subsequent admission within 14 days. Finally, we retrospectively assigned CTAS scores to the older cohort and compared them with the nurse-assigned CTAS scores in a similar fashion to other papers.Reference Mirhaghi, Heydari, Mazlom and Ebrahimi 10 , Reference Lin and Worster 14 , Reference Beveridge, Ducharme and Janes 22 We found good inter-rater reliability, indicating that these patients were likely appropriately triaged as “low acuity,” based on the existing triage tools.
The primary limitations of our study include its health records review design and its limited sample size. A health records review can introduce subjectivity in interpreting the information recorded, and reviewers were not blinded to study objectives. To mitigate potential bias, we measured largely objective outcomes (i.e., admission, hospital revisit) and had two reviewers collect data on 20% of the total charts to ensure consistent recording. We based our data collection on ED records and consultations performed in the department only; therefore, it is possible that some information about patients’ past medical history or social situation was missed without a review of the entire patient record. We did not access other hospital databases or follow up by telephone with patients to ascertain whether they re-presented to other hospitals within 14 days of their ED visit at our centre; thus, revisit rates may have been higher than we calculated in our data set. Lastly, this study was performed at two high-volume centres in the same city, with access to allied healthcare providers such as Geriatric Emergency Management Nurses and Social Work. In smaller centres with less support, one might hypothesize that revisit rates and potentially admissions for older patients could be even higher than we found.
It must be acknowledged that the primary goal of triage is to decide which patients require more urgent access to care, rather than to predict admission rates to the hospital.Reference Manos, Petrie and Beveridge 23 Nevertheless, the CTAS has been shown in several studies to predict resource utilization and patient outcomes.Reference Murray, Bullard and Grafstein 8 , Reference Lee, Oh and Peck 9 , Reference Worster, Fernandes, Eva and Upadhye 24 , Reference Jiménez, Murray and Beveridge 25 There is no other test that has yet been shown to reliably predict poor outcome in older ED patients.Reference Yao, Fang, Lou and Anderson 26 , Reference Fan, Worster and Fernandes 27 The finding in our study that very elderly patients ages 85 and older have the highest admission rates, both on the initial ED visit and at 14 days, indicates that this group is particularly high-risk despite their low acuity CTAS score. As has been suggested by Worster et al., we would suggest that consideration be given to a CTAS modifier for age.Reference Lin and Worster 14 An escalated triage score based on age could alter the perceived acuity of these very elderly patients from the time of their arrival in the ED. It would appropriately reflect the greater ED resources used in the workup of these patients and their increased likelihood of admission.
Future research should focus on the outcomes of this very elderly group and assess whether there are specific factors that contribute to their high admission rates. If possible, studies should assess time to assessment, which is expected to increase with CTAS score, and any adverse outcomes in this population, because this would be the strongest evidence to support CTAS modifier for age.
There is abundant literature to indicate that older patients are at increased risk for adverse outcomes after ED discharge. Our study contributes to this body of knowledge, demonstrating that older patients with seemingly low acuity triage complaints have increased rates of admission to the hospital, both on their index visits and at 14 days compared to younger controls. The very elderly in this low acuity group are nearly twice as likely to be admitted to the hospital than those ages 65 to 84 years. This very elderly group warrants further study and consideration regarding potential modifications to triage scores.
Acknowledgements: The authors would like to thank My-Linh Tran for her assistance with the statistical analysis as well as Angela Marcantonio for her help with the administrative aspects of this study.
Competing interests: None declared.