CLINICIAN'S CAPSULE
What is known about the topic?
Air-medical transport of cardiac patients is common; however, there is little evidence to guide selection of patients at low risk for clinical deterioration during flight.
What did this study ask?
Can a consensus-derived screening tool identify low risk cardiac patients who can be transported safely with primary care flight paramedics (PCP(f)).
What did this study find?
In patients identified as low risk and transported by PCP(f), adverse events are rare at 0.3%.
Why does this study matter to clinicians?
Cardiac patients screened as low risk by this tool can be transported safely with PCP(f) crews, potentially leading to resource and cost savings to health care systems.
INTRODUCTION
Regionalized cardiac care has been shown to result in improved patient outcomes.Reference Topol and Kereiakes1,Reference Singh and MacDonald2 These patients often require transport to tertiary care centers for definitive management, which can include reperfusion therapy, valve replacement, or pacemaker insertion.Reference O'Connor, Al Ali and Brady3 Air-medical services are often used for transport of these patients, given the large distances that may be required to access these centers.Reference Werman, Falcone and Shaner4 This transport, however, is not without risk, and selection of the level of expertise of air-medical crew for these patients can present a challenge.Reference Mitchell, Dionne and Maloney5
Cardiac patients, especially those with acute coronary syndrome (ACS), are at risk for clinical deterioration during flight.Reference Essebag, Halabi, Churchill-Smith and Lutchmedial6 Adverse event (AE) rates from 5.6% to 41.0% for these patients have been reported in the literature.Reference Trojanowski and MacDonald7,Reference Schneider, Borok, Heller, Paris and Stewart8 Moreover, transport from remote locations using fixed wing aircraft has been independently associated with a risk of AEs.Reference Singh, MacDonald, Bronskill and Schull9 In Ontario, it has been reported that 88.5% of patients with ACS are transported by crews composed of either two advanced care flight paramedics (ACP(f)) or critical care flight paramedics (CCP(f)).Reference Trojanowski and MacDonald7 However, for low risk cardiac patients (e.g., non-ST segment elevation myocardial infarction awaiting angiography), the incidence of AEs is not well described, and the optimal crew configuration is unclear. Recently, it has been reported that a crew composed of a single PCP(f) providing basic life support skill can transport safely low acuity patients by means of air-medical transport.Reference Tien, Sawadsky and Lewell10 This is advantageous for rural communities where there are often challenges retaining qualified medical personnel, and definitive care would be accessed more quickly if a single primary care provider was sent versus waiting to coordinate two advanced care providers.
To date, there is a gap in the literature to guide air-medical services in selecting cardiac patients at low risk for AEs during flight. Identification of these patients may allow for transport with PCP(f) crews with potential for significant resource and cost savings. In 2012, Ornge (the air ambulance service in Ontario, Canada) implemented a consensus-derived screening tool to select for stable low risk cardiac patients.
The primary objective of this study was to determine the incidence of AEs in cardiac patients selected for transport with this screening tool and transported by a PCP(f) crew.
METHODS
Study design
We conducted a health records review of cardiac patients transported by Ornge PCP(f) crews since implementation of the screening tool on January 1, 2012, until December 31, 2017.
Study setting
Ontario is the second largest province in Canada, with a landmass of 1.1 million km2 or 424,600 milesReference Singh and MacDonald2. The health care system is publicly funded and services a population of approximately 14 million people. Established in 2006, Ornge is a nonprofit company that is responsible for the provision of air ambulance and critical care land ambulance services for the province. Ornge conducts more than 20,000 transports annually, using rotary wing, fixed wing, and ground resources. Approximately 6% of the transport volume is for scene calls, with the remainder being interfacility transports.11
Northern Ontario constitutes 87% of the land area of the province but contains less than 7% of the population. Ornge coordinates transport services to these rural areas mostly through contracted standing agreement carriers. These carriers use fixed-wing aircraft and PCP(f) crews to service transports.
Flight paramedics are the sole providers of medical care during air ambulance transport. There are three levels of flight paramedics in Ontario, including PCP(f), ACP(f), and CCP(f). PCP(f) level of care is consistent with basic life support, and includes the provision of basic medications, semi-automatic external defibrillation, insertion of supraglottic airways (King LT™), and obtaining and interpreting 12-lead electrocardiograms. ACP(f) crews provide care at an advanced life support (ALS) level, while CCP(f) crews represent the highest designation and can perform rapid sequence intubation, mechanical ventilation, use of inotropes and vasopressors, and administration of fibrinolytic agents. To be qualified for air-medical transport in Ontario, paramedics must pass a government issued Aeromedical Theory Course and are then designated a flight paramedic.
Medical oversight is provided by Transport Medicine Physicians (TMP), who provide full-time online medical control. Flight paramedics provide care using standard orders and medical directives developed by the Ornge Medical Advisory Committee and can patch to TMPs for advice when the level of care exceeds these directives. TMPs have an active role in determining the mode of transportation and level of care required for transport based on the patient's condition.
Screening tool
To assist with identifying low risk cardiac patients, a screening tool was developed at Ornge in 2012 through consensus between TMPs and cardiologists (Figure 1). The tool is completed by the sending physician and all criteria must be met in order for the patient to be classified as “low risk” and transported by PCP(f). If any of the criteria are not satisfied, the sending physician must consult the TMP, who would then use their clinical discretion to determine the appropriate level of care for the patient. The screening tool was not previously tested or validated before its use.
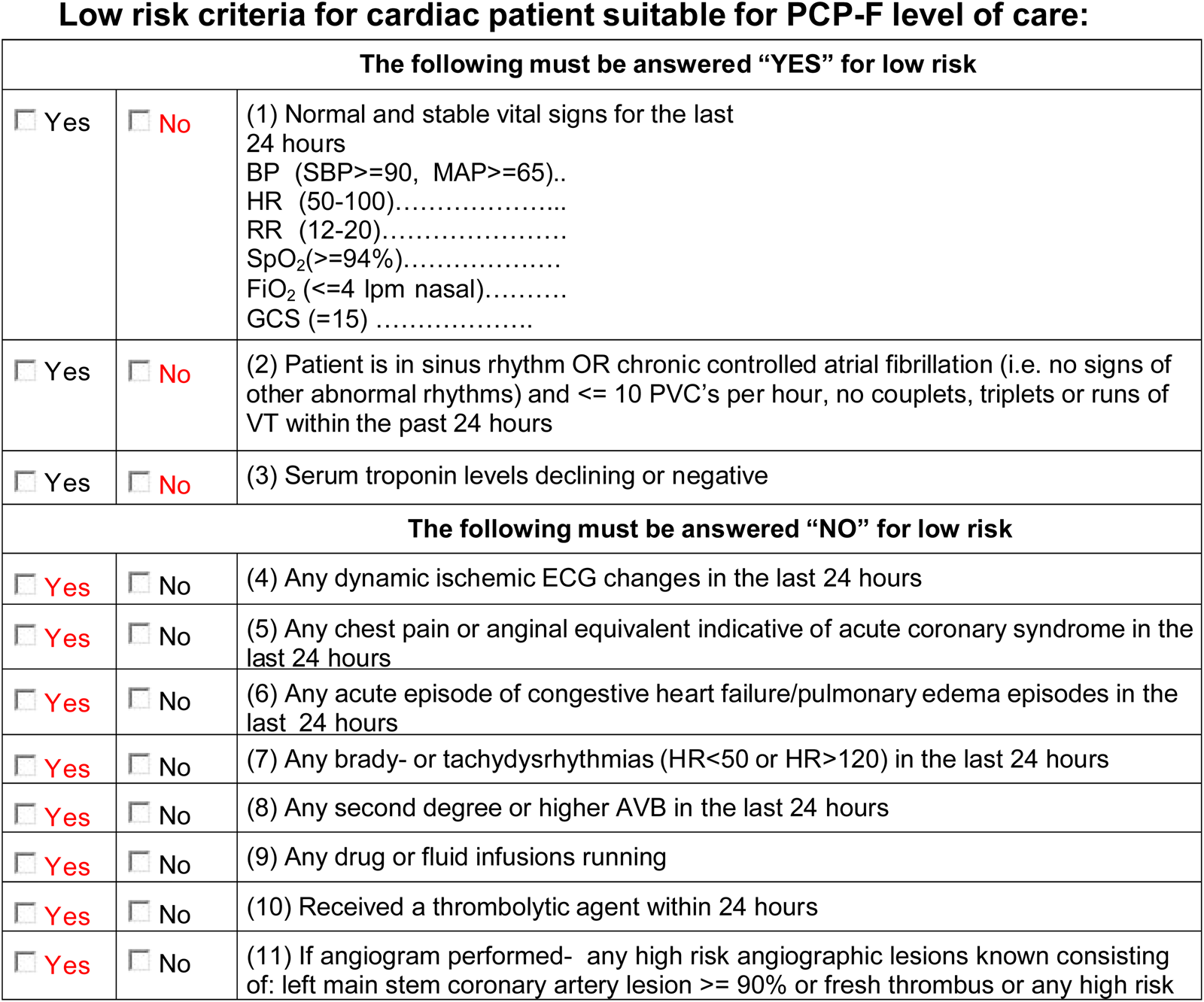
Figure 1. Ornge low risk cardiac screening tool.
Population
Ornge electronic patient care records (ePCRs) were reviewed to identify potentially eligible patients. Patients were included if the low risk cardiac screening tool was applied, transport was provided by PCP(f) level of care, a cardiac-related diagnosis was established (ICD10 range I20–I25; I30–I50), age ≥ 18 years old, and transport was by fixed-wing. Patients were excluded if they were <18 years old, transport was by ACP(f) or CCP(f) level of care, they were accompanied by hospital-based staff, or transport was from a scene call or by rotary wing or ground vehicles. This study was approved by the Ottawa Health Science Network Research Ethics Board.
Case identification and data collection
Our case identification strategy used Flight Vector™ dispatch software to identify all transports where the low risk cardiac screening tool was applied and transport was provided with PCP(f) level of care. Scanned copies of the completed screening tool by the sending physician were obtained from this software.
Ornge uses ePCRs for most of its patient documentation; however, contracted service agreement carriers use paper ambulance call records. These records were obtained, deidentified, and scanned into electronic copies. Information was abstracted from the ambulance call records using a standardized, piloted data collection form by a single trained data extractor. A second reviewer abstracted data from a random 10% of patient records, with any disagreements discussed until resolution. All abstracted data collection forms were subsequently entered into a spreadsheet (Microsoft Excel; Microsoft Corporation, Redmond, WA, USA) for further analysis.
Outcome measures
Our primary outcome was AEs that occurred during patient transport. We used the Institute of Medicine definition of AE, described as, “unintended physical injury resulting from or contributed to by medical care (including the absence of indicated medical treatment), that requires additional monitoring, treatment, or hospitalization, or that results in death.”Reference Kohn, Corrigan and Donaldson12 To identify our primary outcome of AEs, we used a two-step process. First, study investigators created a list of AE triggers derived by group consensus, which we defined as events that have been flagged to represent potential AEs. Our AE triggers included: TMP patch call, hypotension (systolic blood pressure < 90 or mean arterial pressure < 65), bradycardia (heart rate < 50), tachycardia (HR > 100), decreased level of consciousness (Glasgow Coma Scale [GCS] < 15 or decrease in GCS from baseline), ACP(f)/CCP(f) intercept during transport for higher level of care, nitroglycerin administration, chest pain, hypoxemia (oxygen saturation < 90%), arrythmias (supraventricular tachycardia, ventricular tachycardia, atrial fibrillation with rapid ventricular response), high grade atrioventricular block (Mobitz type 2 or third degree), and cardiac arrest. The clinical narratives surrounding these AE trigger events were reviewed by committee of two TMPs external to the study (including one external to Ornge) and blinded to study outcomes to determine which satisfied our Institute of Medicine definition of a true AE. A third TMP was used if consensus could not be reached by unanimous agreement. Secondary outcomes included patient and transport characteristics.
Data analysis
We used simple descriptive statistics and report means with standard deviations. Interrater reliability was determined using the Cohen's kappa statistic.
Sample size
The sample size for this health record review was determined by the number of patients selected for PCP(f) transport by the low risk cardiac screening tool during the 6-year study period, starting when the screening tool was first used.
RESULTS
During the 6-year study period from January 1, 2012, to December 31, 2017, PCP(f) crews transported 402 cardiac patients selected as low risk by the screening tool. Of these, 2 patients were excluded due to missing data, leaving 400 patients included in the study (Figure 2).
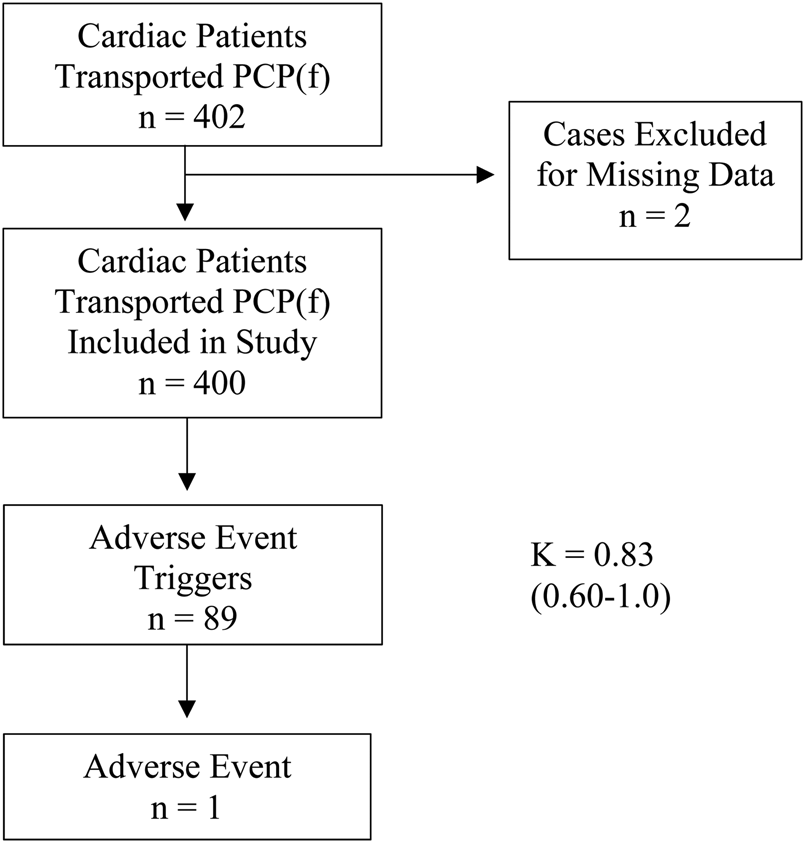
Figure 2. Study flow diagram.
Patient and transfer characteristics are depicted in Table 1. Overall, 66.5% of patients were male. Most patients had cardiac risk factors, with hypertension being the most common (50.3%), followed by coronary artery disease (39.5%). The most common reason for transport was for cardiac catheterization (61.8%), followed by coronary artery bypass grafting (26.8%), valve replacement (4.3%), and repatriation (3.5%).
Table 1. Patient and transfer characteristics (n = 400)
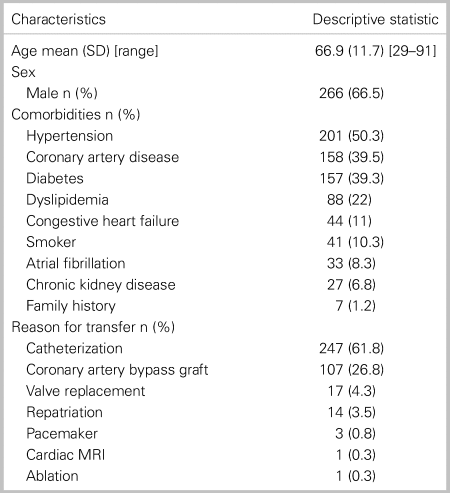
SD = standard deviation; MRI = magnetic resonance imaging.
The mean transport duration was 136.2 (74.9) minutes (Table 2). Dispatch priority of patients, described here in decreasing level of acuity, was assigned as “Prompt” (12.3%), “Scheduled” (78.3%), and “Deferrable” (9.5%). Most patient transports occurred in Northern Ontario, with the most common sending locations being Thunder Bay (37.5%), Kenora (23.5%), Sioux Lookout (9.8%), and Fort Frances (7.3%).
Table 2. Transport characteristics

SD = standard deviation.
Of the 400 patient transports, 89 AE triggers were identified (Table 3). The most common was bradycardia (n = 24), patch call (n = 16), hypoxemia (n = 14), chest pain (n = 12), tachycardia (n = 10), and hypotension (n = 8). There were no cases of ventricular tachycardia, high degree atrioventricular block, cardiac arrest, or death. There was very good interrater agreement (K = 0.83) for identification of AE triggers.
Table 3. AE triggers
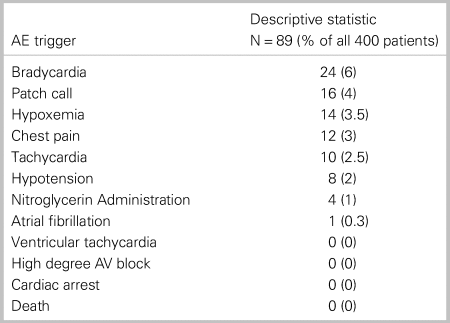
AV = atrioventricular.
The 89 AE triggers were reviewed by a committee of two TMPs external to the study to determine which trigger events constituted true clinically important AEs. This committee used the Institute of Medicine definition of AE defined previously herein. After review of the 89 AE triggers, the consensus committee identified only one clinically important AE, with an overall AE rate of 0.3% overall. A narrative of the AE is as follows. The patient was being transported for an implantable cardioverter-defibrillator device. During transport, the PCP(f) crew documented an “extreme tachycardia” alarm on their monitor, with no intervention performed. The patient subsequently had a 2-minute syncopal episode while unloading the aircraft.
In addition, we identified a subgroup of 10.5% of patients who did not pass the screening tool (i.e., patient high risk); however, transport was approved by PCP(f) by the TMP. In these higher risk patients, 40.5% of them were identified to have an AE trigger, compared with 15.7% of patients who passed the screening tool and were deemed low risk. The patient identified to have the true AE was screened as high risk by the tool but transported by PCP(f).
DISCUSSION
In this health records review, we determined the frequency of AEs in low risk cardiac patients selected for PCP(f) transport by a screening tool. We found the incidence of AEs to be very low (0.3% overall), with no serious events such as cardiac arrest, death, or airway intervention. Based on these results, we suggest that a consensus-derived screening tool used by Ornge can reliably select for low risk cardiac patients who can be transported safely by PCP(f) crews.
In our study, we looked specifically at AEs in a subgroup of low-risk cardiac patients selected by a screening tool. A previous study looking at patients with ACS or cardiogenic shock transported by air ambulance in Ontario identified an AE rate of 5.6% among 2,258 transfers.Reference Trojanowski and MacDonald7 This, however, was across all levels of paramedic crew skills (PCP(f), ACP(f), and CCP(f)), and did not involve the use of a screening tool to preselect patients. In their subgroup of patients transported by PCP(f) only, there was an AE rate of 0.3% which is consistent with our study results. A large study of 3,767 transports of ST-elevation myocardial infarction (STEMI) patients by Youngquist et al. found a rate of clinical decompensation of 4.8%.Reference Youngquist, McIntosh, Swanson and Barton13 They found that pretransport cardiac arrest or requirement for a critical ALS intervention were the two most important predictors of AE during transport. Kaplan et al. found that 12% of acute myocardial infarction (AMI) patients transported by air had complications requiring treatment; however, no death occurred.Reference Kaplan, Walsh and Burney14 Bellinger et al. studied patients with AMI transported after thrombolytic therapy and found in-flight complications to be rare, with transient hypotension responding to fluid boluses the most common complication.Reference Bellinger, Califf and Mark15 In contrast, Schneider et al. found that serious AEs occurred in 41% of air-medical transports of patients with myocardial infarction or unstable angina, with events including arrythmia, chest pain, hypotension, and cardiac arrest.Reference Schneider, Borok, Heller, Paris and Stewart8 This difference in AE rates is likely due to the significant heterogeneity between illness severity reported in the literature, selection bias, as well as differences in AE definitions in prehospital literature.
The clinical performance of this low risk cardiac screening tool developed and used by Ornge was never previously reported. Other scoring systems, such as the prehospital National Early Warning Score, have been implemented in prehospital medicine and found to predict patient mortality within 1 day of emergency medical services dispatch with good diagnostic accuracy, but are not specific to patients with cardiac disease.Reference Pirneskoski, Kuisma, Olkkola and Nurmi16 A study by Tien et al. found that a single PCP(f) crew configuration could transport safely low acuity patients by air ambulance with a medical deterioration rate of 0.6%.Reference Tien, Sawadsky and Lewell10 However, this study included all patient presentations and was not specific to those with cardiac disease. Finally, Mitchell et al. demonstrated the safety of a PCP-initiated STEMI bypass program.Reference Mitchell, Dionne and Maloney5 However, this study involved ground ambulances and short mean transport times.
LIMITATIONS
This study is subject to some limitations. First, we encountered two instances of missing patient care records; however, this represented only 0.5% of eligible cases and was unlikely to influence our results. Second, the study was likely subject to reporting bias in the documentation of AEs by paramedics; however, any serious AEs are unlikely to have been missed given their required care. Third, due to resource constraints, we were unable to compare the AE rate with cases where the screening tool identified the patient as high risk and where transport was provided by ACP(f)/CCP(f) crews. Fourth, our selection criteria were only able to identify cases where the screening tool was used and transport was provided PCP(f); we did not look at cases where only TMP judgment was used to send patients PCP(f), which may have had a different incidence of AEs.
CONCLUSION
A screening tool can identify cardiac patients at low risk for clinical deterioration during air-medical transport, with an AE rate of 0.3%. In 400 transports over a 6-year period, no serious event such as airway intervention, cardiac arrest, or death occurred. We believe patients screened with this tool can be transported safely with PCP(f) crews. Future research should look at prospective validation and refinement of the tool, and evaluate potential savings in resource usage.
Financial support
This study was supported by a grant from the Department of Emergency Medicine, University of Ottawa.
Competing interests
None.







