INTRODUCTION
Background
Eighty-five percent of sudden cardiac arrests happen at home,Reference Vaillancourt and Stiell 1 where most victims are aged in their sixties, and where the most likely bystander to witness the event is a similarly aged spouse.Reference Vaillancourt, Verma and Trickett 2 A victim is three to four times more likely to survive if they receive bystander cardiopulmonary resuscitation (CPR) before emergency medical services arrive.Reference Stiell, Wells and DeMaio 3 CPR is one of only a few modifiable factors associated with increased survival for out-of-hospital cardiac arrest (OHCA),Reference Sasson, Rogers and Dahl 4 and good quality CPR has been the focus of recent resuscitation guidelines.Reference Travers, Perkins and Berg 5
Importance
In 2010, the International Liaison Committee on Resuscitation changed their treatment recommendation from using a 30:2 compression to ventilation ratio to using a continuous chest compressions strategy. This was meant to minimize chest compression interruptions, increase the number of compressions delivered, and increase bystander CPR rates by addressing technical difficulty and bystander reluctance associated with rescue breathing.Reference Travers, Rea and Bobrow 6 - Reference Cunningham, Mattu and O’Connor 8 However, the ability of bystanders aged 55 years or older (the population most likely to witness OHCA) to sustain the increased effort necessary to provide continuous chest compressions and the resulting consequences on the quality of CPR provided requires further evaluation.
Goals of this investigation
Our study sought to measure bystander fatigue and CPR quality after five minutes of CPR performed using the 2010 continuous chest compression (CCC) treatment recommendation compared to five minutes of CPR performed using the 2005 standard of 30 compressions to two ventilations (30:2) in a population aged 55 years or older.
METHODS
Study design
We used a randomized crossover trial design comparing bystander fatigue and CPR quality when performing CCC versus a 30:2 compression to ventilation ratio method of CPR. This study protocol was registered with the U.S. National Institutes of Health www.ClinicalTrials.gov NCT [NCT01397656].
Setting
We set up study booths in four busy public areas located in Ottawa, Canada. Three of these booths were located in three large city hospitals; the other was set up within a suburban community seniors’ center.
Selection of participants
Participants were eligible for inclusion in the study if they were aged 55 years or older, whether they had previous CPR training or not. They also had to score three or better on the validated Clinical Frailty Scale (three being: “With well-controlled treated comorbid disease.”),Reference Rockwood, Song and MacKnight 9 be able to follow instructions in English or French, and be able to understand and provide informed consent. Potential participants could not take part in the study if they met any of the following exclusion conditions: 1) any musculoskeletal conditions precluding their ability to kneel down and perform CPR; 2) any cardiovascular conditions precluding their ability to perform a moderate effort; 3) presence of an active communicable disease; or 4) inability to perform chest compressions at appropriate rate and depth despite positive feedback during a 1-2 minute practice session.
This study was approved by the Ottawa Health Science Network Research Ethics Board and participants were asked to provide written informed consent. We offered free refreshments during study participation, and the possibility to enter a drawing for one of two bookstore gift certificates.
Study intervention and methods of measurement
After a brief CPR demonstration, each participant was given one to two minutes to become familiar with the Actar Manikin (Armstrong Medical, Lincolnshire, IL) and practice CPR under supervision. Study investigators provided participants with verbal feedback on their CPR technique during the practice session, but not during the study intervention. A metronome was set at 100 beats per minute to encourage the same chest compression rate for all participants during the practice session and the study intervention.
We asked participants to perform two 5-minute sessions of CPR on a manikin attached to a Zoll R-Series Monitor (Chelmsford, MA) that recorded the CPR quality process data without providing automated CPR quality feedback to the participants. The 5-minute length of CPR was chosen to simulate the expected elapsed time between a 9-1-1 call and the arrival of an ambulance during a real cardiac arrest situation.Reference Vaillancourt and Stiell 1 Participants started with either the CCC method or the 30:2 compression to ventilation ratio as determined by the random allocation. They had as much time as they required to recover to their baseline fatigue level between the practice and the start of the study, as well as between each of the two 5-minute CPR sessions (measured using the Borg Scale).Reference Borg 10 After performing the two CPR techniques, participants completed a brief survey. Each participant was expected to complete this study within approximately 30 minutes.
Participant allocation
We randomly assigned participants to the first CPR method (CCC or 30:2) using randomly permuted blocks with length of four. We concealed participant assignments in sealed opaque envelopes.
Outcome measures
We measured the following baseline characteristics: age, gender, heart rate, and blood pressure (using Smart Logic Life Brand blood pressure monitor Model 5534), Clinical Frailty Scale (range from 1-7 where a score of one is associated with the least frailty),Reference Rockwood, Song and MacKnight 9 and Borg Rating of Perceived Exertion scale (range from 6-20 where a score of 6 is associated with the least fatigue).Reference Borg 10 We measured baseline heart rate, blood pressure, and Borg scale measurements before each CPR session.
We measured participant fatigue before and after each CPR session using changes in heart rate, blood pressure, and Borg Rating of Perceived Exertion. Participants also completed a brief survey immediately after each CPR session, asking them how much longer (in minutes) they perceived being able to perform CPR using each method. At the end of the second CPR session, participants were also asked if they felt more tired at the beginning of the second 5-minute CPR session compared to the first 5-minute CPR session, and which CPR method they liked the best.
We assessed CPR quality using the Zoll R-series Monitors attached to each manikin. Using the Zoll RescueNet Code Review Software (version 5.2, Chelmsford, MA), we analyzed the frequency and number of chest compressions attempted during each 5-minute CPR session, and the number of adequate chest compressions of at least 5 cm in depth performed during the same period.
Data analysis
We described and compared baseline characteristics of participants between the randomized groups using mean and standard deviation for continuous variables and frequencies and proportions for categorical variables. We used descriptive statistics to summarize the subjective measures of fatigue reported in the brief survey. We investigated the normality of the distributions for all outcome measures.
To compare measures of fatigue and CPR quality at the end of each 5-minute session between the two CPR techniques, we used intention-to-treat statistical methods appropriate for the analyses of cross-over trials, taking into account any possible period and carry-over effect of fatigue from one CPR session to the next. For outcomes where the assumption of normality was clearly satisfied, we used a General Linear Model (GLM) that included both a period and a carryover effect.Reference Kenward and Roger 11 The treatment effect (difference between the two CPR groups) was estimated from the model, together with 95% confidence interval (CI). For outcomes that had a skewed distribution or for which the assumption of normality appeared questionable, we additionally conducted a non-parametric analysis. For the non-parametric analysis, we used the Wilcoxon two-sample test for both the period and treatment effects.
To analyze the number of adequately performed chest compressions per minute, we used a random coefficient model. The dependent variable in these analyses was the number of chest compressions performed during each consecutive minute (five minute duration). The independent variables were time (minute), CPR group, interaction between CPR group and time, as well as period and carry-over effects. The intercept and time were specified as random effects to account for correlations among the repeated measures on each subject. The model was estimated using the SAS procedure “Mixed” with Restricted Maximum Likelihood Estimation and degrees of freedom estimated by the Kenward and Roger method.Reference Kenward and Roger 11 We obtained the estimated population mean slope for the two compression groups, as well as the difference between the slopes, together with 95% confidence intervals. The slopes represent the average rate of change in number of adequately performed chest compressions per minute between the two methods.
The required number of paired data was calculated using the standard formula for a cross-over design, namely Nd=[(Zα+Zβ)2 σd 2]/δd 2; where Nd=required number of participants, Zα=1.960 (using two-sided α =0.05), Zβ=1.282 (power of 90%), σd 2=estimated variance of the paired difference, and δd=minimally important mean difference between experiments.Reference Jones and Kenward 12 Guided by previous work published by Lucia on the importance of physical fitness in the performance of adequate cardiopulmonary resuscitation, we used an estimated variance of σd 2=2 cm and a minimally important difference of δd=1 cm in compression depth.Reference Lucia, de las Heras and Perez 13 Based on these estimates, 60 participants were required to detect a significant difference in the number of adequately performed chest compressions. We completed all statistical analyses using the SAS software (Cary, NC, USA; version 9.2).
RESULTS
Characteristics of study participants
We assessed 69 volunteers between July and August 2010 for participation in the study, and excluded six who did not meet all entry criteria (Figure 1). Of the 63 participants enrolled in the study, four were too tired to complete the full 5-minutes of CPR using both methods and one using the CCC method. Baseline characteristics for our 63 participants (13 recruited at the seniors’ center, 50 recruited at the three city hospitals) are presented in Table 1. The average rest time required by participants between CPR sessions was 8:59 minutes and ranged between six and 16 minutes.
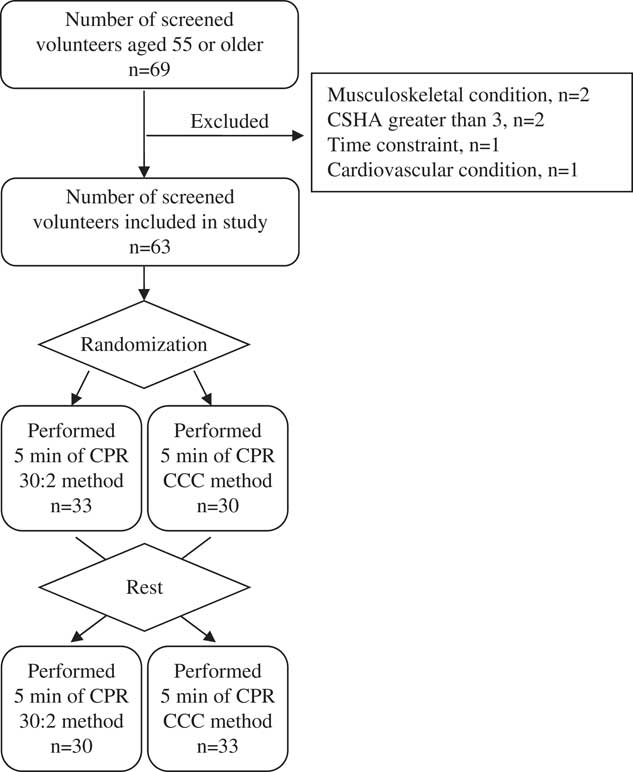
Figure 1 Study participants’ CONSORT flow diagram CSHA, Canadian Study of Health and Aging score; CPR, cardiopulmonary resuscitation; CCC, continuous chest compressions
Table 1 Characteristics of the 63 volunteers at the beginning of the study

CCC, continuous chest compressions; CPR, cardiopulmonary resuscitation; MAP, mean arterial pressure; SD, standard deviation.
Survey data
When asked after each CPR session, 71% of participants said they could continue to perform the 30:2 method of CPR for two or more minutes, compared to only 63% when performing the CCC method of CPR. When asked immediately following the completion of the second CPR session, 66% of participants reported having felt the same level of energy immediately before each CPR session. In the end, 69% of participants said they preferred the 30:2 method of CPR over the CCC method.
Main results
Measures of fatigue at the end of each session are presented in Table 2. The results from the GLM analysis of bystander heart rate, accounting for the period and fatigue carry-over effects, showed no statistically significant carry-over (p=0.9268) and no significant difference between the CPR groups (CCC v. 30:2 mean difference: −0.59, 95% CI −3.51-2.33, p=0.6879). However, the analysis of MAP revealed a significant carry-over (p=0.0111) and a mean difference of 1.64 (95% CI −0.23-3.50, p=0.0845). The GLM analysis of the BORG scores also revealed a significant carry-over effect (p=0.0317) and a mean difference of 0.46 (95% CI 0.0-70.84, p=0.0206). To investigate the carry-over effect for MAP and BORG scores, we calculated the mean difference (CCC minus 30:2) when the CCC method was used in the first period (4.1 for MAP, and 0.03 for BORG scores) versus when it was used in the second period (−0.8 for MAP, and 0.88 for BORG scores). When we discarded the second period data (as it was possibly contaminated due to carry-over), we found no significant difference between the CPR groups (mean difference for MAP =0.16, 95% CI −5.3-5.6, p=0.9526, and mean difference=0.97, 95% CI −0.48-2.4, p=0.1859 for BORG scores).
Table 2 Comparison of fatigue measures using the CCC method versus the 30:2 compression to ventilation ratios

CCC, continuous chest compressions; CI, confidence interval; SD, standard deviation; BPM, beats per minute;
MAP, mean arterial pressure
Measures of CPR quality are presented in Table 3. Participants were able to maintain the recommended frequency of 100 chest compressions per minute during each CPR session. However, when they used the CCC method, participants performed more chest compressions (480 v. 376). The results from the GLM analysis of number of chest compressions accounting for the period and fatigue carry-over effects showed no carry-over effect (p=0.0720) and a mean difference between the CPR groups of 108 (95% CI 89-127, p<0.0001). Since there was some evidence of skewness, we also conducted a non-parametric analysis. In this analysis, the p-value for the period effect was 0.1792 and the difference between CCC and 30:2 was statistically significant (p<0.0001).
Table 3 Comparison of CPR quality measures using the CCC method v. the 30:2 compression to ventilation ratios.
CCC = continuous chest compressions; SD = standard deviation; CI = confidence interval; cc = chest compressions
* difference in slopes (rate of change per minute)
When participants used the CCC method, they performed more chest compressions of adequate depth (382 v. 325). The results from the GLM analysis showed no significant carry-over (p=0.9799) and a statistically significant treatment difference of 62 (95% CI 33-91, p=0.0001). In the non-parametric analyses, the p-value for the period effect was 0.8004 and the treatment effect was statistically significant (p=0.0002).
The number of adequately performed chest compressions during each minute is presented in Figure 2. The number of adequately performed chest compressions decreased significantly over time for the CCC method, but not for the 30:2 method. Slope estimates for the CCC method and the 30:2 method were −4.08 (95% CI −5.78 to −2.38; p<0.0001) and −0.27 (95%CI −1.96 to 1.42; p=0.75) respectively. In other words, the rate of decline was an average of 4.1 compressions per minute in the CCC method compared to 0.27 when using the 30:2 method. The rate of decline for the CCC method was significantly greater compared to the 30:2 method (difference in slopes 3.81; p=0.0002), both statistically and clinically. The carry-over effect was not significant (p=0.3637).

Figure 2 Count of adequate chest compressions per minute for each method (with minimum depth of 5 cm). Slope CCC =−4.1, Slope 30:2=−0.3 Difference between slopes =3.8, p=0.0002 CCC, Continuous Chest Compressions
DISCUSSION
We performed a randomized cross-over trial comparing bystander fatigue and CPR quality after five minutes of CPR using the CCC versus the 30:2 method in a population most likely to witness a cardiac arrest, those aged 55 years and older. There were no differences attributable to group assignment. There were no differences in physiological measures of fatigue between methods. However, participants preferred the 30:2 method. Over a 5-minute span, the CCC method resulted in more compressions completed compared to the 30:2 method. Despite a faster decline in CPR quality in the CCC group, the number of adequate compressions per minute still remained higher in this group compared to the 30:2 method. The CCC method appeared potentially superior in our population age group when CPR is performed for a limited number of minutes before EMS arrival.
There have been a few studies comparing the 2010 standard to the 2005 standard of CPR. Nishiyama et al. performed a randomized control trial comparing CCC to 30:2 CPR in two separate groups of non-health care workers aged 18 and older.Reference Nishiyama, Iwami and Kawamura 14 They computed a CPR quality index consisting of the proportion of chest compressions with adequate depth among total chest compressions given, comparing the two groups every 20 seconds over a 2-minute time period. They found the CPR index was significantly lower when the CCC method was used compared to the 30:2 method. In contrast to our study, they compared their CPR index score looking at the proportion of adequate to non-adequate depth of compressions, not the total compressions of adequate depth. Inherently, the 30:2 CPR technique introduces pauses for ventilation during which no compressions are being provided. We wanted to compare the total number of adequate chest compressions being provided to cardiac arrest victims in addition to their proportional quality.
Neset et al. performed a randomized control study comparing CCC to 30:2 CPR with participants aged 50 years and older.Reference Neset, Birkenes and Myklebust 15 In their study, they found that all participants from both CPR groups could perform 10 minutes of CPR. Average compression depth was similar using both methods. They did not, however, look at compressions of adequate depth. Heart rate measurements were similar for both groups, as was subjective physical strain following CPR performance. This is not surprising as participants tend to exert themselves equally regardless of CPR method.Reference Vaillancourt, Midzic and Taljaard 16 , Reference Pierce, Eastman and McGowan 17 Odegaard et al. compared CCC to 30:2 and 15:2 CPR with volunteers between the ages of 15 and 87.Reference Odegaard, Saether and Steen 18 They also found that CCC resulted in more compressions per minute than 30:2, but the quality of compressions in the CCC group was significantly less compared to those using the 30:2 method. This is inconsistent with our findings. However, they only looked at average compression depth, not the number of compressions of adequate depth. Their findings showed that compression depth for CCC decreased over time whereas the compression depth for 30:2 remained stable, which is also consistent with our findings.
Unlike our previous study comparing 15:2 to 30:2 compressions to ventilations, where doing more chest compressions was associated with increased reports of fatigue,Reference Vaillancourt, Midzic and Taljaard 16 reported fatigue was equal in both groups following CCC versus 30:2 compressions to ventilations in the current study. Pierce et al. suggest that physiological changes may underestimate the actual or perceived demands of performing CPR, which could explain the lack of measured fatigue by participants.Reference Pierce, Eastman and McGowan 17 Therefore, although participants may not have been reporting feeling more tired following one method of CPR versus the other, they may have been underestimating how fatigued they really were. In our study, we also controlled the rate of compressions by having participants follow a metronome timed at 100 beats per minute. Monsieurs et al. observed excessive compression rate using the CCC method results in insufficient compression depth.Reference Monsieurs, De Regge and Vansteelandt 19 Had we not controlled compression rate, participants may have been more fatigued following the CCC method, and produced even fewer good quality compressions.
Of course, all these studies compare the advantages of one CPR method over another using manikins and simulated cardiac arrest situations. Nichol et al. recently published a very large cluster-randomized cross-over trial comparing 30:2 CPR to CCC in 26,148 OHCA victims and found no advantage favoring one method or the other regarding survival to hospital discharge or favorable neurologic function.Reference Nichol, Leroux and Wang 20
LIMITATIONS
This study has its limitations. First, although the majority of participants said they subjectively felt as rested as they were at baseline prior to starting their second session of CPR, objective measures of fatigue were higher than baseline in 33.1% of participants. Second, the software we used to measure compression characteristics did not measure if each compression was fully decompressed or not. However, in our previous study, we noted that compressions were increasingly less likely to be fully decompressed with each subsequent minute of CPR.Reference Vaillancourt, Midzic and Taljaard 16 Third, our study participants were required to be healthy or have well-controlled comorbid diseases. This may not be representative of a similarly-aged population witnessing cardiac arrest at home. Finally, we used manikins to simulate a cardiac arrest victim. Although this may not entirely reproduce the stress or physical sensation associated with providing CPR to a loved one, we intentionally conducted our study in a public place to reproduce some of this anxiety.
CONCLUSION
In a population of bystanders aged 55 years or older most likely to perform CPR on a cardiac arrest victim, CPR quality decreased significantly faster when performing CCC compared to 30:2. However, performing CCC produced more adequate compressions over a 5-minute period than the 30:2 method, despite similar levels of fatigue.
Acknowledgements
We are grateful to the volunteer participants in our study for their time and effort. Without their enthusiasm and contributions, our study would not have been possible. We would also like to extend our thanks to Mrs. Natalie McRae (Babony) and the Zoll Medical Corporation for providing us with unrestricted use of their defibrillators and software. We would finally like to thank Mrs. Angela Marcantonio for all her help processing the submission of this manuscript.
Competing Interest: Funding from the Department of Emergency Medicine Academic Practice Plan, and University of Ottawa’s Undergraduate Research Opportunity Program (UROP). No other potential conflicts of interest declared.







