CLINICIAN'S CAPSULE
What is known about the topic?
Early blood product administration to patients with hemorrhagic shock has a positive impact on morbidity and mortality.
What did this study ask?
What is the need for blood products in patients undergoing time-sensitive air medical transport?
What did this study find?
This study found that 2.5% of patients undergoing time-sensitive air medical transport have indications for blood product administration.
Why does this study matter to clinicians?
Air medical services can enhance access to potentially lifesaving therapy in patients with hemorrhagic shock by carrying blood products.
INTRODUCTION AND BACKGROUND
Patients suffering from hemorrhagic shock are at high risk of morbidity and mortality.Reference Gann and Drucker1 Resuscitation with blood products have significant benefits over crystalloid alone, because crystalloids are associated with pulmonary edema, clot dislodgement, abdominal compartment syndrome, acidosis, cerebral edema, and coagulopathy.Reference Ravi and Puri2,Reference Holcomb, Tilley and Baraniuk3 Populations that may benefit from blood transfusions include patients with acute gastrointestinal bleeding (GIB), abdominal aortic aneurysm (AAA) rupture, trauma, coagulopathy, and pregnancy-related complications.Reference Baumann Kreuziger, Morton, Subramanian, Anderson and Dries4
Currently, in Ontario, blood products are routinely available in medium to large hospitals. Smaller hospitals may have only a limited supply of blood products, and nursing stations do not stock or have prompt access to blood products. In addition, land-based emergency medical services (EMS) or paramedic services do not routinely stock or carry blood products.
Support for prehospital blood product transfusion is growing.Reference Mena-Munoz, Srivastava and Martin-Gill5–Reference Bodnar, Rashford and Williams8 Studies of patients with multisystem traumatic injuries show a 95% reduction in odds of 24-hour mortality rate with air prehospital blood administration and a greater than 40% reduction at 30 days.Reference Brown, Cohen and Minei9 While some studies have demonstrated questionable benefit in trauma, they were conducted before the balanced transfusion era. Newer studies using a balanced resuscitation approach suggest a similar mortality benefit with this balanced approach in the prehospital environment.Reference Sumida, Quinn, Lewis, Jones and Baker10–Reference Kim, Zielinski and Jenkins12 It is essential that blood product administration be clinically indicated, because patients with traumatic brain injury who received a blood transfusion during transport who had no clinical evidence of shock had worse outcomes.Reference Elterman, Brasel and Brown13 Further research is needed regarding the optimal patient population and administration of blood products during transport.
In Ontario, healthcare is highly regionalized with specialized centres in larger metropolitan areas providing the vast majority of tertiary and quaternary care services. This regionalized system requires an air and land critical care transport program capable of transporting potentially unstable patients to definitive care. In order to meet the needs of the patients that it transports, a review of unmet need for blood products is necessary to improve access in areas where access is either limited or nonexistent. The primary outcome of this study is to quantify the number of patients meeting established physiologic criteria for blood product administration and to identify which patients receive and which ones do not receive blood products due to a lack of availability locally.
METHODS
Study design
We conducted a retrospective review of all patients undergoing air or land critical care transport to identify those in whom administration of blood products may have been beneficial during the 2017 calendar year.
Setting
Ontario is a large Canadian province (approximately 1.1 million km2 or 424,600 milesReference Ravi and Puri2) with a mix of urban, suburban, rural, and remote areas. The healthcare system is publicly funded and serves a population of approximately 13.5 million people. Ornge Transport Medicine is the publicly funded air medical and land critical care transport system providing all air medical patient transfers in Ontario. Ornge is Canada's single largest air medical transport provider, carrying out approximately 20,000 patient transports annually, of which approximately half are emergent, time-sensitive transports.
Ornge aircraft operate as either advanced or basic life support aircraft, with flight paramedics as the sole providers during transport. The scope of practice for advanced and critical care flight paramedics includes the administration of blood products,14 where such administration is done in consultation with dedicated physicians providing direct medical control and in keeping with medical directives and standing orders developed by the Ornge Medical Advisory Committee. All blood products administered by Ornge paramedics originate from sending facilities. The three most common indications for blood transfusion are hemorrhagic shock due to multisystem traumatic injuries, GIB, and postpartum hemorrhage (PPH), historically accounting for more than 90% of blood product administration at Ornge.Reference MacDonald and Ramjaun15 These three patient cohorts were selected for this study because of established criteria for blood product use.Reference Day, Anzelon and Conde16–Reference Rau, Wu and Kuo20
For the purposes of this study, a hospital with a limited supply of blood products was defined as having a small number of uncrossmatched units of blood (typically 2 to 4 units of O-negative and/or O-positive), no blood banking facilities, and no ability to crossmatch blood products.
Study population
The study screened all patient records for patients undergoing transport by Ornge flight paramedic crews during the 2017 calendar year. Patients were included, if upon review, the patient underwent emergent transport, had a presenting complaint of multisystem trauma, GIB, or PPH. Patients were excluded if the reason for interfacility transport was nonurgent repatriation, if transfer was cancelled by the sending facility, the patient was transported by another ambulance or service, or was pronounced dead prior to Ornge personnel making patient contact. Appendix 1 outlines the inclusion criteria, Appendix 2 outlines the criteria for blood product administration, and Figure 1 outlines derivation of the cohort.

Figure 1. Study cohort.
Established measures of shock used in identifying patients in need of blood product administration include the shock index (SI)Reference Day, Anzelon and Conde16 and change in shock index (ΔSI).Reference Schellenberg, Strumwasser and Grabo17 The shock index is defined as the heart rate (beats per minute) divided by systolic blood pressure (mm Hg). In trauma patients, an SI > 0.9 is associated with increased risk of mortality.Reference Day, Anzelon and Conde16 In patients with an SI of > 1.2, massive transfusion protocol (MTP) utilization is indicated.Reference Schroll, Swift and Tatum18–Reference Rau, Wu and Kuo20 As such, trauma patients with an SI > 1.2 at any point during transport were identified as benefitting from blood products administration. In patients with an upper GIB, an SI > 1.0 at any point during transport was used to identify patients as benefitting from blood products. In patients with pregnancy-related complications, an SI > 1.7 at any point during transport was used to identify patients as benefitting from blood products.
In addition, patients with a hemoglobin level of 70 g/L or less, identified either at the sending facility or by the Ornge transport team, were included based on principles and clinical practice guidelines developed by Choosing Wisely Canada.21 Patients requiring administration of vasopressor medications in the setting of a profound hemorrhage were also identified and included.
Data abstraction
Patient demographics (age, sex), sending hospital, and Ornge patient ID were abstracted from Ornge's electronic patient care record (ePCR). The reviewers used the ePCR to determine whether administration of blood products was indicated (see Appendix 2). The reviewers also identified whether any blood products were administered, how many, and of which type of product(s) was used, based on a specific procedure code documented by the paramedics on the ePCR.
Statistics
Two reviewers reviewed patient records independently. Data were collected on patient demographics, physiologic parameters, interventions during transport (i.e., intubation, tourniquet use), sending facility location, and whether or not blood products were administered.
Descriptive data were reported as means and standard deviations for parametric data or medians and interquartile ranges for nonparametric data. Any discrepancies between reviewers were resolved with a third reviewer blinded to the results of the initial review.
RESULTS
There were 11,520 emergent patient transports during the study period. Multisystem traumatic injuries, GIB, and PPH accounted for 95% of the total blood product administration during the study interval. Of 11,520 patients, 842 (7.3% of total) had one of the three presenting problems eligible for inclusion in this study. Of these, 290 (2.5% of total) met established physiologic criteria for blood product administration. The two investigators independently identified the same patients meeting inclusion criteria and were in agreement on which patients met established physiologic criteria for blood product administration.
A total of 167 of the 290 patients received blood product by Ornge flight paramedic crews prior to arrival at definitive care, with 57 of the 167 receiving products at a hospital with limited blood supply. The mean number of units administered per patient was 3.5. Table 1 summarizes the patient demographics and call types. Table 2 summarizes the time intervals for patients who met physiologic criteria for blood products administration.
Table 1. Patient demographics and call types

*Significant difference (p < 0.05) compared with a potentially eligible cohort.
**Modified scene call: rotor-wing aircraft initially dispatched to the scene, but re-routed in flight to meet local land EMS crew at the closest hospital, where patient contact is made.
Table 2. Time intervals (all times in minutes; mean ± standard deviation)
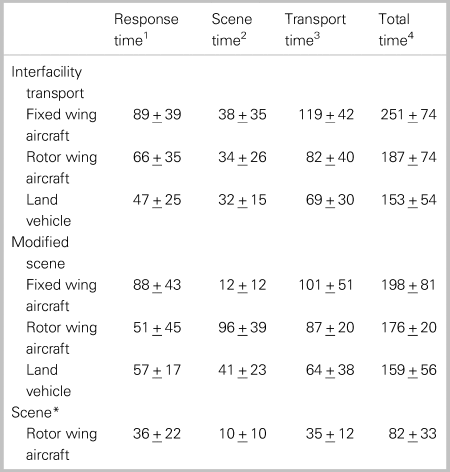
1Interval from call received to crew arrival at patient side.
2Interval from crew arrival at patient side to depart scene.
3Interval from depart scene to transfer of care at receiving facility.
4Interval from call received to transfer of care at receiving facility.
*All scene calls carried out by rotor wing aircraft.
The remaining 123 patients (42.4%) meeting criteria did not receive product because none was unavailable. The majority were scene responses, where blood products were not available on the aircraft.
DISCUSSION
Our findings suggest that a significant proportion of patients experiencing hemorrhagic shock in the transport setting also meet established criteria for blood product administration. We find that the need for blood is not adequately met due to limited availability, particularly for scene responses. In all, 180 (62.1%) out of 290 patients meeting physiologic criteria for blood product administration either did not receive it or received it at a facility with limited blood supply. Making blood products available to air medical crews would address that unmet need.
Early fluid resuscitation and strategies to control hemorrhage can be lifesaving,Reference Davis, Martin and Schreiber22,Reference Schroll, Smith and McSwain23 but prehospital crystalloid and colloid alone do not improve survival.Reference Bulger, May and Kerby24 Evidence for optimal hospital-based transfusion protocols for hemorrhagic shock and massive transfusions is now well established.Reference Holcomb, Tilley and Baraniuk25 The emphasis on early transfusion of plasma, platelets, and packed red blood cells (pRBCs) in balanced ratios leads to improved survival in the setting of hemorrhagic shock.
In order to identify a cohort of patients who would benefit from blood product administration, we opted to use previously published thresholds for shock indices.Reference Day, Anzelon and Conde16–Reference Rau, Wu and Kuo20 The thresholds differed based on the presenting problems but were based on the available published evidence. This approach was conservative in nature and would likely underestimate the true number of patients benefitting from blood product administration. Indeed, 93 patients identified in this study did not meet the physiologic criteria used in the study, yet these patients received blood products. This would support that the supposition that the thresholds used in the study was conservative, and the study's results underestimate the true need for blood products.
Early intervention with blood products is relevant in air medical transport where times to definitive care may be prolonged, and blood products are either not available or only in limited supply. Blood products administration during helicopter transport shows survival benefit in military and civilian settings for patients with severe injuries.Reference Shackelford, Del Junco and Powell-Dunford26,Reference Sperry, Guyette and Brown27 These findings suggest that damage-control resuscitation can be started during transport and can improve outcomes for patients destined for a trauma centre.Reference Cannon, Khan and Raja28
Blood product wastage is a concern, but wastage in the prehospital setting is minimal. In one example where blood was stored at land ambulance bases, paramedics administered 130 units of pRBCs over an 18-month period, with 97.8% of pRBC units not used being returned to the hospital-based blood banking system and, therefore, not wasted.Reference Bodnar, Rashford and Williams8 Of 898 units of pRBCs dispensed to an air medical program, 131 (14.6%) were transfused to 81 patients, with 756 (84.2%) returned to the blood bank, and 11 (1.2%) wasted.Reference Krook, O'Dochartaigh and Martin29
Ideally, patients with massive hemorrhage should receive pRBCs, fresh frozen plasma, and platelets in a ratio of 1:1:1. The results of this study indicate that this is not the current practice in this setting. In all, none of the 167 patients receiving pRBCs received fresh frozen plasma, and only 10 received platelets. This is likely due to the lack of availability of these two latter blood products at sending hospitals and the time it takes to thaw frozen plasma and make it available at the sending hospital before transport occurs. The availability of plasma may improve, particularly in the prehospital and transport setting,Reference Shlaifer, Siman-Tov and Radomislensky30 when freeze-dried plasma becomes available.
In addition to blood product availability, the crew's ability to safely function in the transport setting and deliver uncrossmatched blood product is essential to mitigate risk. The administration of blood products and management of potential complications are within the scope of practice for paramedics in Canada,14 and patients transported by crews specifically trained to work in the transport setting result in better patient outcomes and have fewer adverse events compared with ad-hoc hospital-based personnel.Reference Hatherill, Waggie, Reynolds and Argent31–Reference Bellingan, Olivier, Batson and Webb33
Shortened time to definitive care improves outcomes, and activation of a transport service for the patient with hemorrhagic shock is a key component to any regional or provincial massive hemorrhage protocol.Reference Callum, Yeh and Petrosoniak34 Shortening the time to definitive care to improve outcomes in patients with multisystem traumatic injuries,Reference Sampalis, Denis and Levoie35,Reference Celso, Tepas and Langland-Orban36 STEMI,Reference Carter37 and strokeReference Benoit, Khatri and Adeoye38,Reference Zaidi, Shawver and Espinosa Morales39 is well established, and regionalization to improve efficiency and outcomes is not new.Reference Sampalis, Denis and Levoie35
Equipping air medical transport services with blood products is of value in the regionalized delivery of healthcare. It can shorten time to definitive care, overcoming some of the challenges related to challenges in distance and geography that preclude readily available blood products at hospitals and healthcare facilities where utilization may be rare and wasting a precious resource is a concern.
Limitations
While this summary is the experience of Canada's largest air and land critical care transport provider, its findings are not necessarily applicable to other programs, patient populations, or geographic settings. Ontario is unique geographically, with distinct differences in resources, including the availability of blood products.
Given the strict physiologic criteria used in this study to retrospectively assess for indications for blood product administration, it is not possible to accurately determine the true need for blood product in this patient population. As a result, the findings of this study likely underestimate the true need for blood product administration in this setting.
Finally, approximately 5% of the blood product administered during the study period went to patients with other diagnoses. Catastrophic hemorrhage due to large vessels rupturing, such as an AAA, accounted for the remaining patients. These patients were not included in the study because the cohort was small, there are no clearly defined criteria for the administration of blood products, and potential controversy exists regarding fluid resuscitation.Reference Moreno, Cacione and Baptista-Silva40
CONCLUSION
Indications for blood product administration are present in 2.5% of patients undergoing time-sensitive air medical transport. Air medical services can enhance access to potentially lifesaving therapy in patients with hemorrhagic shock by carrying blood products, as blood may be unavailable or in limited supply locally in the majority of patients where it is indicated.
Supplemental material
The supplemental material for this article can be found at https://doi.org/10.1017/cem.2020.2.
Acknowledgements
The authors acknowledge Mahvareh Ahghari for her assistance in carrying out this study.
Competing interests
None declared.





