INTRODUCTION
Back pain is a common occurrence, chronically affecting up to 84% of Canadian adults at some point in their lives.Reference Andersson 1 There are numerous causes of back pain with the majority being attributed to musculoskeletal injury; however, less common conditions such as malignancy, infection, inflammatory disorders, degenerative disorders, and visceral diseases are also involvedReference Della-Giustina 2 , Reference Deyo and Weinstein 3 (Table 1). In over 80% of back pain cases, the exact trigger is unknown, and physicians describe the pain as a musculoskeletal injury.Reference Deyo and Weinstein 3 , Reference Ehrlich 4 Some of these conditions resolve after several weeks without any specific treatment, whereas others can result in chronic lower back pain.Reference Della-Giustina 2 Occasionally, patients may have a serious underlying systemic disease, including infectious, neoplastic, or inflammatory causes that manifest as back pain. In the clinical evaluation of back pain, it is important to recognize “red flags” that warrant further investigation in a timely mannerReference Deyo and Weinstein 3 (Table 2).
Table 1 Causes of back pain.Reference Della-Giustina 2 , Reference Corwell 10 , Reference Chou, Qaseem and Snow 11
Table 2 Red flags for lower back pain.Reference Della-Giustina 2 , Reference Corwell 10
Chiropractic manipulation of the spine (CSM) is a popular therapy for lower back pain and is viewed by the public as a relatively safe treatment.Reference Owell, Hanigan and Olivero 5 Although the public perception of CSM is that of a safe treatment, there have been multiple cases of injury resulting from spinal manipulation, including dislocations and fractures of vertebrae.Reference Hebert, Stomski and French 6 - Reference Ernst 8 The absolute risk of undergoing CSM is still actively debated, with continuing calls for more evidence actively debated.Reference Ernst 9 Certain medical conditions are contraindicated in specific types of CSM techniques, and, unfortunately, a patient may not always be aware that they have the underlying condition.Reference Globe, Farabaugh and Hawk 12 It is in these instances that emergency physicians may need to investigate beyond the presenting symptoms to entertain the possible underlying pathology behind a patient’s presenting complaint of back pain following CSM.
CASE REPORT
A 66-year-old male was seen by his family physician for investigation of lower back pain that had been present for the past 4 weeks. The patient had been active and previously well prior to the development of this pain. He had not experienced any previous traumatic injury, the pain was initially described over his lumbar region, and he did not demonstrate any neurological deficits.
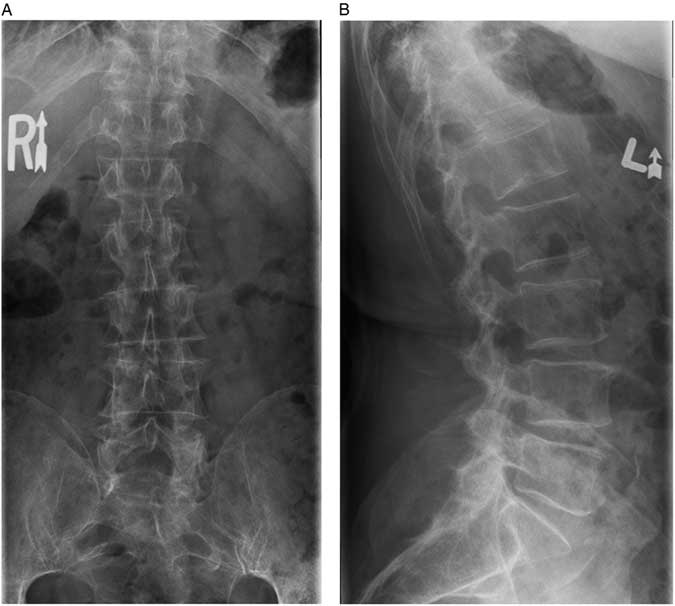
The family physician ordered thoracolumbar spine radiographs, which subsequently were reported as being free of any lesion or fracture (Figure 1). His past medical history was remarkable for a transient ischemic attack and hypothyroidism for which the patient was taking clopidogrel bisulfate, 75 mg once daily, and levothyroxine, 100 μg once daily, respectively. The patient’s routine laboratory investigations over the previous year demonstrated normal vitamin D, sodium, potassium, and chloride levels as well as a normal urinalysis. Two years prior, the patient did have a transient pancytopenia, which, after resolving spontaneously, was not investigated further. It was recommended by the family physician that the patient try conservative measures for his lower back pain, including the use of nonsteroidal anti-inflammatory medication.
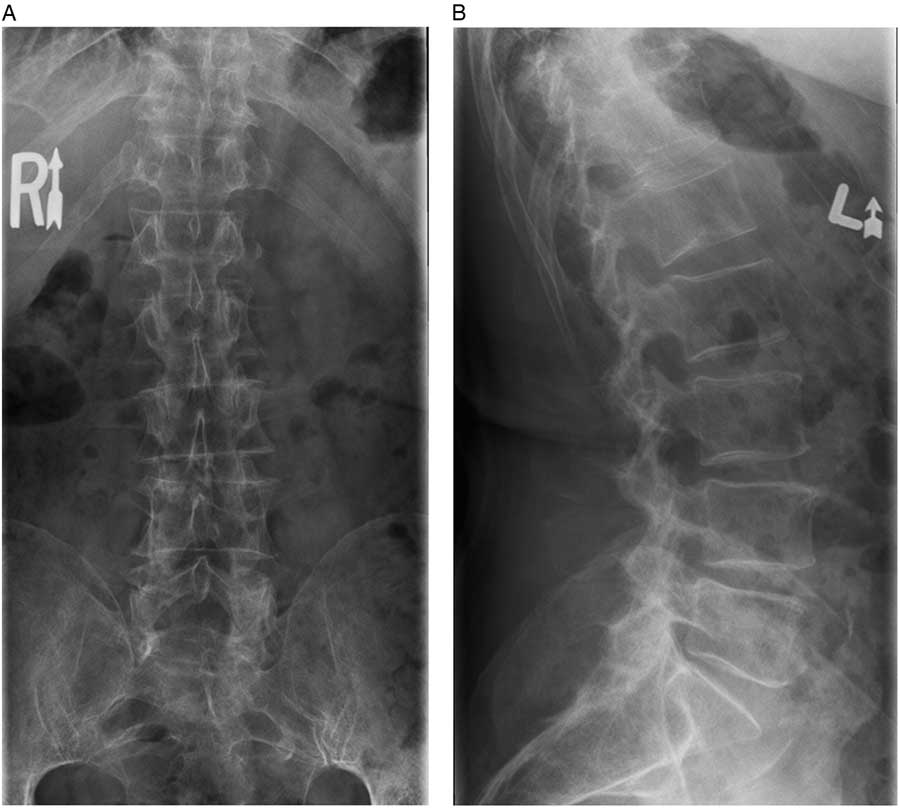
Figure 1 A) Anterior-posterior and B) lateral radiographs of the thoracolumbar spine acquired in the community. No spinal injuries were noted.
Following his visit to his family physician, the patient sought treatment from his local chiropractor. The patient underwent spinal manipulation for a suspected mechanical injury as the presumed cause of his lower back pain. The patient was unfortunately unable to accurately describe the exact type of thoracolumbar manipulation performed. Within 24 hours of manipulation, the patient developed more intense lower back pain. Despite this, he proceeded to attend two more sessions over the next 5 days with increasing levels of pain both during and following spinal manipulation. Due to the patient’s discomfort, the chiropractor recommended that he follow up with his family physician.
The family physician prescribed cyclobenzaprine, 10 mg, for muscle spasms and zopiclone, 7.5 mg, at night to help the patient with a new inability to sleep. Despite taking the cyclobenzaprine, the patient continued to have persistent lower back pain. The patient was seen again by the family physician 5 days later and was prescribed methoxisal, 1 to 2 tabs for four times a day as needed.
The patient presented to the emergency department following 1 day on the new medication. On examination, his vital signs were within normal limits, and he had a body mass index of 23.4 kg/m2. The patient described pain across the lower back and demonstrated tenderness on palpation of the lower thoracic and lumbar spinous processes. The patient had a limited range of motion at the lumbar spine due to pain. The patient had an unremarkable hip exam, and his lower extremity joints were unaffected. His motor function, sensation, and deep tendon reflexes were all normal. His cardiovascular, respiratory, and abdominal exams did not demonstrate any abnormalities. There was no palpable lymphadenopathy, and the digital rectal exam was unremarkable.
Laboratory investigations revealed pancytopenia, with a hemoglobin of 115 (range 137–180) g/L, leukocyte count of 1.9 (range 4.0–11.0×109)/L, and a platelet count of 135 (range 150–400×109)/L. Red blood cells were normocytic with a low reticulocyte count of 1%, and his peripheral blood smear demonstrated rouleaux cell formations. His serum electrolytes and creatinine were within normal limits. Hypercalcemia was detected with a corrected calcium level of 2.80 (range 2.10–2.55) mmol/L. New thoracic and lumbar spinal radiographs revealed subacute compression fractures involving the T11, L1, L2, and L3 vertebrae that were not present on the original films ordered by the family physician (Figure 2).
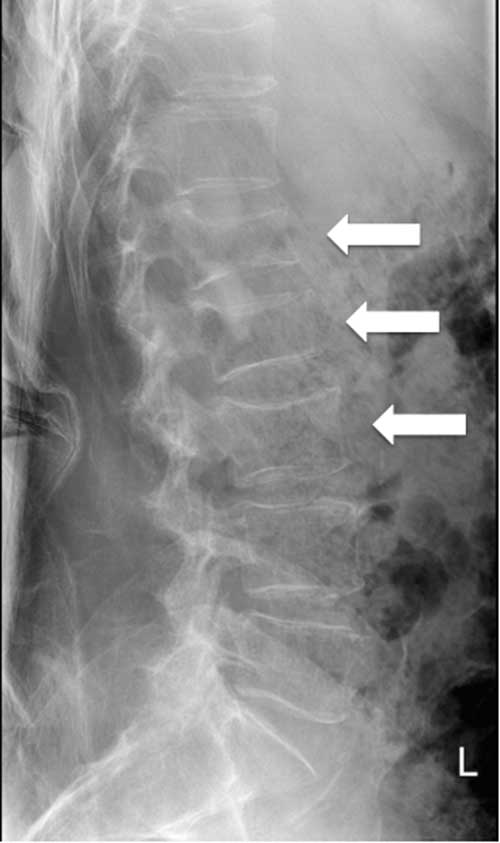
Figure 2 Lumbar spine radiograph acquired on presentation to the emergency department at 14 days following the initial spinal imaging. Loss of vertebral height of L1 (32%) and L2 (34%) as well as a mild central compression of L3 are revealed.
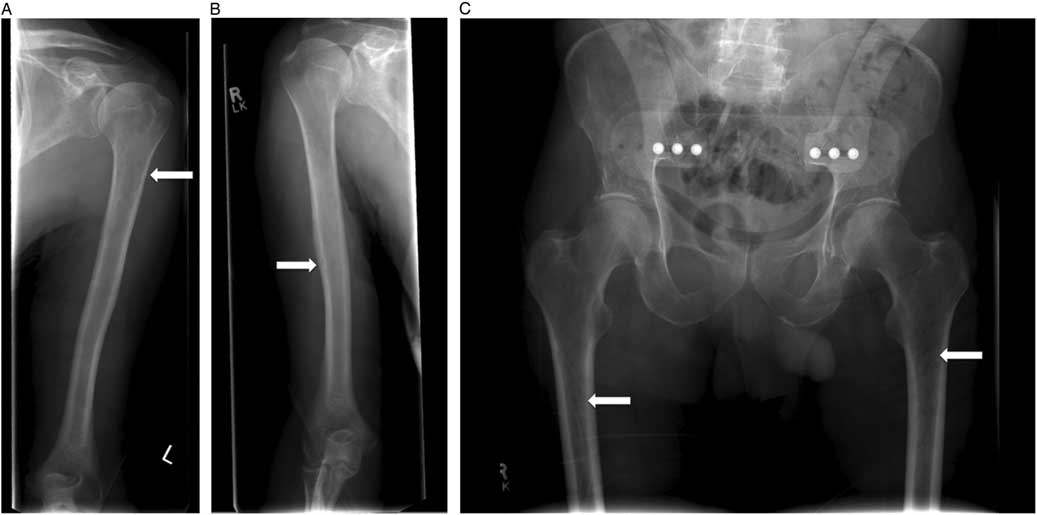
This patient was admitted and received further investigations to elucidate the cause of his compression fractures, pancytopenia, and hypercalcemia. The serum protein electrophoresis revealed an elevated gamma globulin, and urine protein electrophoresis revealed free lambda light chains. Immunoglobulin A (IgA) was significantly elevated at 39.36 (range 0.60–4.20) mg/L, as was the β2 microglobulin level at 4.80 (range 1.00–2.60) mg/L. A bone marrow biopsy confirmed a diagnosis of multiple myeloma. A skeletal survey demonstrated additional lucencies in the proximal femur and humerus bones bilaterally (Figure 3, A–C). The patient was followed by the hematology service for further management.
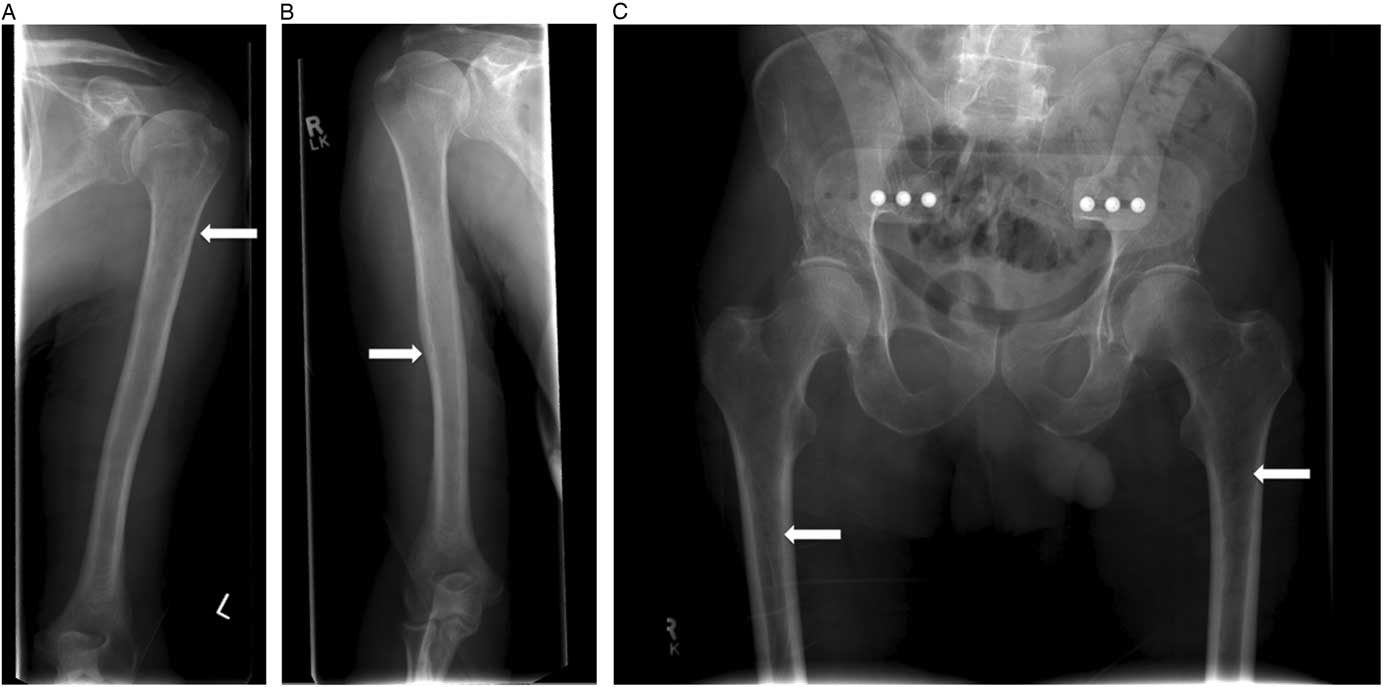
Figure 3 A, B) Skeletal survey identified radiographic lucencies in the proximal humeri and C) femurs bilaterally.
DISCUSSION
The majority of back pain is typically benign, self-limiting, and can be managed conservatively. In certain cases, back pain can have a more insidious cause such as the underlying malignancy discussed previously. The potential for harm with CSM in the context of undiagnosed spinal disease is a cause for concern. Although the fractures in the case described previously cannot be determined to be the sole result of the CSM, the association cannot be overlooked.
The incidence of CSM-related cervical spine complications is estimated to be between 5 and 10 per million manipulations.Reference Hurwitz, Aker and Adams 13 Unfortunately, information describing complications involving thoracic and lumbar spine manipulation is harder to find. Rubinstein et al. published a Cochrane meta-analysis in 2012 that investigated 16 articles encompassing 578 participants undergoing some form of CSM.Reference Rubinstein, Terwee and Assendelft 14 They found that only two cases involved a serious complication following manipulation of the thoracic or lumbar spine. The adverse events in these cases were not the result of the CSM itself. A systematic review by Hebert et al. published in 2012 reported 77 cases of CSM-related injury following manipulation of the lumbopelvic region over 41 articles.Reference Hebert, Stomski and French 6 The authors found that 9% of complications were fractures of the lumbar and thoracic vertebrae, with the majority being lumbar compression fractures and the exact technique of CSM being vaguely described.Reference Livingston 15 , Reference Austin 16
There are a variety of manipulative techniques used in chiropractic practice, with Canadian chiropractors using two or more techniques on average.Reference Mykietiuk, Wambolt and Pillipow 17 Classic techniques involve either static or dynamic high velocity, low amplitude (HVLA) thrusting or flexion/extension and distraction (joint separation).Reference Triano, McGregor and Skogsbergh 18 Recent clinical practice guidelines published by the American Chiropractic Association have found that most commonly studied and used therapies for lower back pain involve HVLA and flexion/distraction techniques.Reference Globe, Farabaugh and Hawk 12 HVLAs are contraindicated in patients with diseases like multiple myeloma because it can cause harm to the patient.Reference Globe, Farabaugh and Hawk 12 The most probable cause for our patient’s fractures is the use of HVLAs during his CSM due to his undiagnosed multiple myeloma.
Due to the many general risk factors for lower back pain, a detailed physical and history should be performed to identify red flags prior to initiating CSM. It is generally encouraged that patients older than 65 years with back pain should receive age- and symptom-appropriate laboratory investigations prior to initiating CSM. New evidence has been reported contradicting this mentality by demonstrating that early spine imaging versus later spine imaging in patients with new onset back pain had no significant difference in rates of missed cancer diagnoses.Reference Jarvik, Gold and Comstock 19 A recent systematic review evaluated the red flags of lower back pain directly related to cancer diagnoses.Reference Downie, Williams and Henschke 20 They reported that the greatest risk factor for fracture was older age, prolonged steroid use, severe trauma, or contusions and abrasions. The greatest risk factor for malignancy was a previous cancer diagnosis. Additionally, they reported several minor risk factors for cancer diagnosis such as age over 50, unexplained weight loss, and failure to improve after 1 month.Reference Downie, Williams and Henschke 20 Unfortunately, our patient’s risk factors, pain at rest and at night, and his previous episode of pancytopenia did not appear to be given more consideration.
Physician attitudes have also shifted towards a multidisciplinary approach to patient management, and thus chiropractors are often sought as team members in caring for those with musculoskeletal injuries and lower back pain. Although spinal manipulation may benefit carefully selected patients, there should be caution in patients with risk factors for osteoporosis, architectural bone disease, or underlying systemic disorders. Learning from our patient’s case, it is important to look for red flags on patient evaluation and use appropriate clinical judgment to determine initial suitability for CSM. As emergency physicians, remembering the associated underlying conditions that can cause a patient to present following CSM treatment is essential.
CONCLUSION
Emergency physicians, family physicians, and chiropractors are often the first contacts for patients with lower back pain, and they should perform a detailed history and physical to rule out undiagnosed medical conditions. This case serves as another reminder to ensure that red flags are properly investigated in what can potentially be a benign presentation.
Acknowledgements: The authors would like to thank the patient and his family for their assistance and willingness to share their story.
Competing interests: None declared.