Background
Schools of medicine in the United States are required to deliver a curriculum in ethics and humanities as a condition of accreditation by The Liaison Committee for Undergraduate Medical Education.Footnote 1 The purpose of this requirement is left unspecified, and schools variably focus curricular objectives on transmitting knowledge of normative ethics, shaping students’ professionalism, promoting reflection and empathy, and promoting virtuous character, among others.Footnote 2 –Footnote 8 The impact of these varied curricula remains difficult to measure due, in part, to the fact that its instructional objectives often are neither squarely performance-based nor behaviorally based.Footnote 9 , Footnote 10 These curricula may do little to effectively address the negative influences of the “hidden” curriculum,Footnote 11 , Footnote 12 to bolster students’ concern for social issues, to advance their skills in moral reasoning, and to preserve levels of empathy.Footnote 13 –Footnote 18 Although schools teach ethics increasingly as integrated within the curriculum,Footnote 19 schools do not typically teach moral reasoning and ethical analysis as deployable clinical skills, and competencies in undergraduate medical education (UME) do not require capability in identifying and managing ethically complex aspects of clinical care.Footnote 20 –Footnote 23
We submit that the goals of UME generally, and its ethics and humanities curricula specifically, are to produce physicians proficient in rendering quality medical care while negotiating the moral, ethical, social, and existential challenges of clinical practice within a demanding practice environment, a complex health system, and all within an evolving sociopolitical context. Toward this end, we created an integrative and outcomes-driven course in Social Sciences, Humanities, Ethics, and Professionalism (SHEP), within a three-year medical school. A substantial portion of the course is devoted to experiential activities in which moral reasoning and ethical analytic skills are applied to ethical and social frameworks and then advanced as clinical skills. We distinguish this activity from the more narrowly focused ethics case analysis that is common in health care education. For the latter, medical educators widely use the “four-box method,” which the authors found insufficient for our overall educational objective.Footnote 24
In the absence of tools designed to develop these integrative moral, ethical, and sociostructural knowledge and skills, we endeavored to create one. The SHEP Case Analysis Tool (SCAT) serves a number of purposes: (1) reinforce knowledge-based portions of the curriculum course pedagogy through convenient and immediate access to relevant information, (2) support meta-cognition through concept mapping and to stimulate thinking deeply and broadly about cases, and (3) apply multidimensional analysis to identify ethical, social, and systems issues that impact care of patients. The exercise in which this tool is used, the analysis and presentation of a case to peers and faculty, additionally serves to (4) develop problem-solving skills, (5) explicitly address the hidden or informal curriculum and support professional identity formation, and (6) to develop skills in reflective discourse with peers.
Concept mapping is an educational and metacognitive strategy by which complex concepts and relationships are actively and graphically represented.Footnote 25 SCAT was created on an open-access web-based concept mapping platform (Mindomo.com). First, we created a schematic of the structure and flow of clinical cases from initial assessment to treatment options to shared decision-making to outcome. Second, we added key stakeholders, inputs, influences, subinfluences, and structural considerations and features of the health system, across micro- and mezzo-levels, which have a bearing on clinical care (Figure 1). These include organizational ethics, racism and discrimination, and moral distress, among other concerns and considerations that affect clinical care. Each schematized and mapped element of the tool appears on the platform as a “tile.” Each tile opens to reveal a synopsis of the SHEP curricular material pertinent to the topic area (Figure 2). This aspect of the tool provides “point of need” reinforcement of the course pedagogy. Each tile’s curricular material is supplemented with question prompts to stimulate the application of the topical material to the case under analysis (Figure 3).
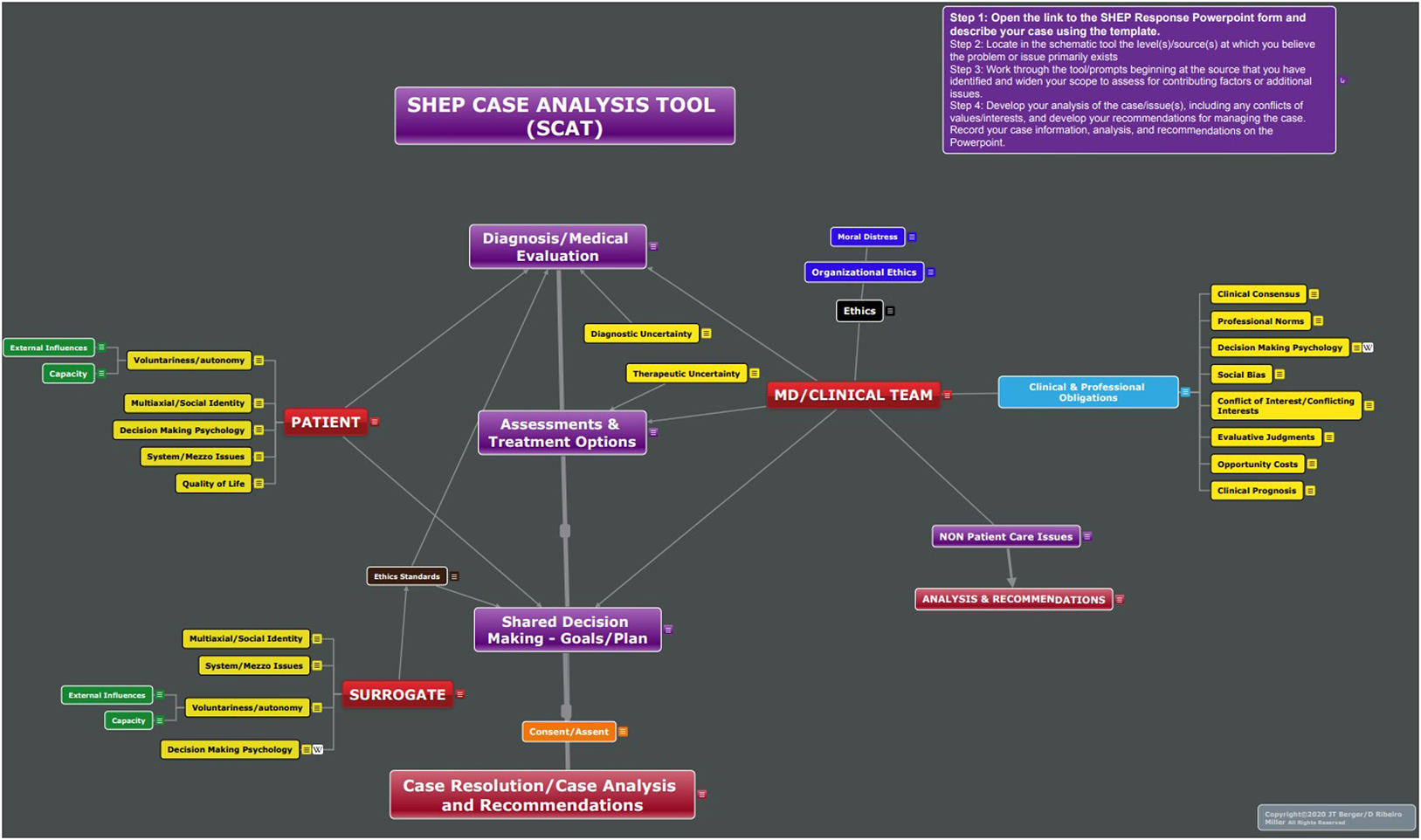
Figure 1. Full SCAT Concept Map.
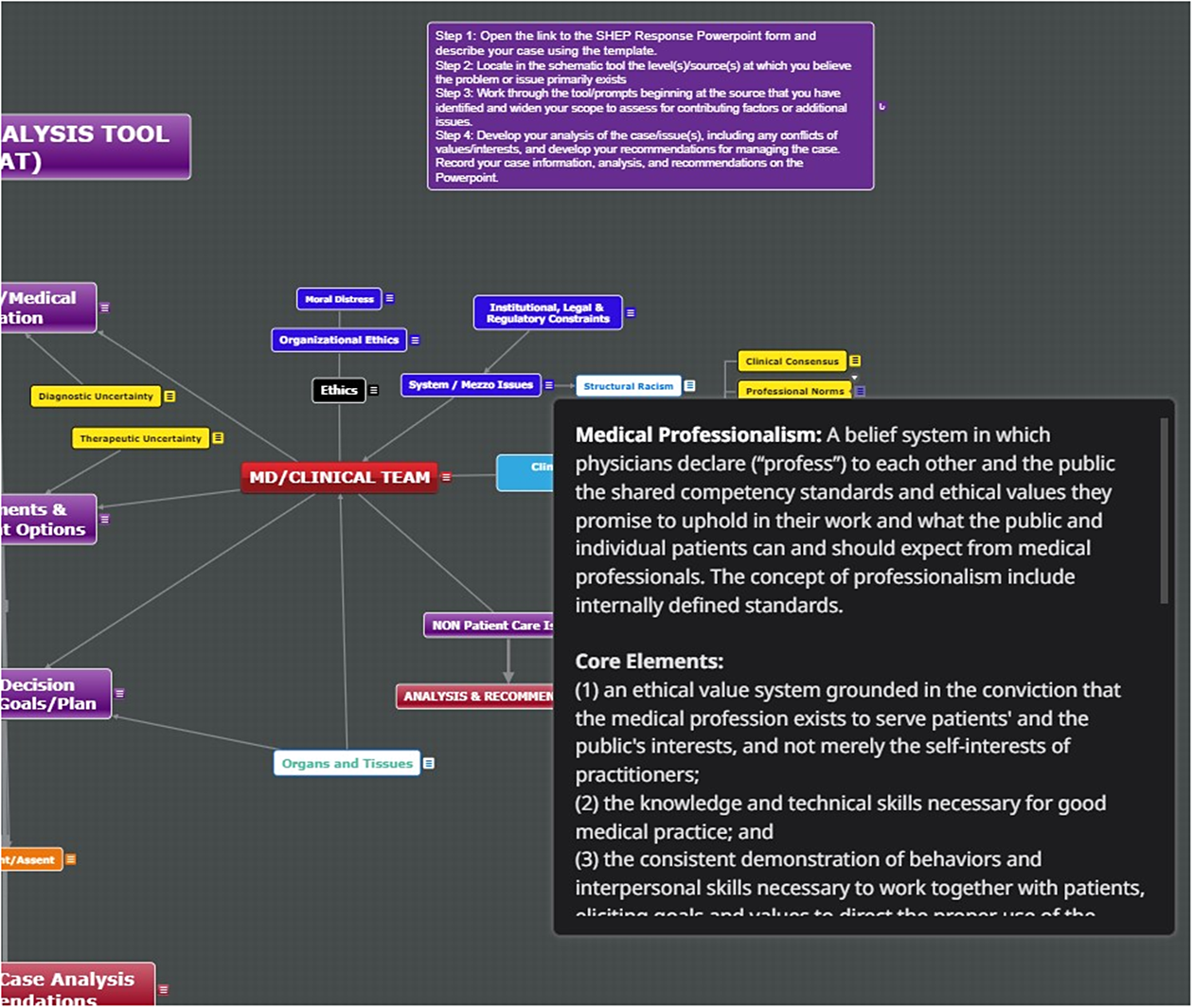
Figure 2. SCAT Expanded Tile/Content.
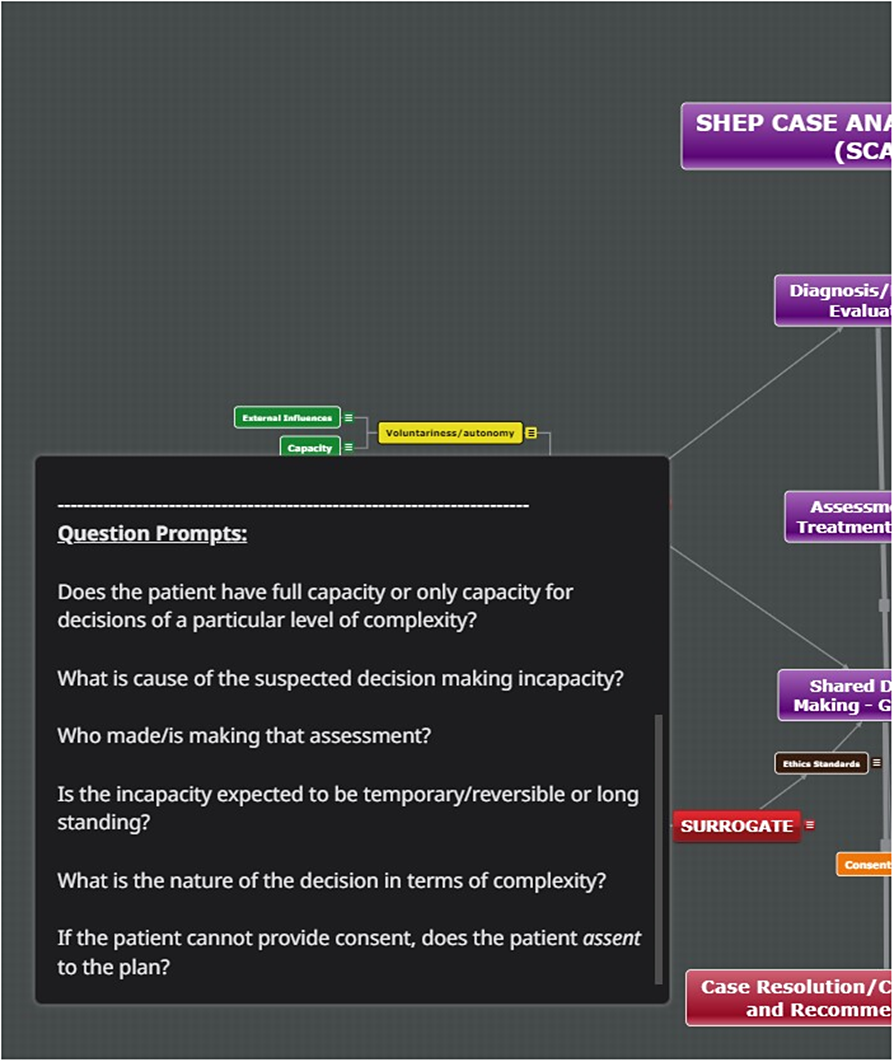
Figure 3. SCAT Question Prompts.
Once the tool was designed and loaded with content, it was beta tested with a group of medical residents and a group of attending physicians. We received feedback for concept, content, and design that led to reorganization of the tool to improve mapping flow and to visually de-clutter the tool. The tool was further revised for simplicity and for content additions and enhancements based on user experiences. A substantial portion of the SHEP pedagogy is represented in SCAT.
The SCAT-based case exercise is a prominent feature of the second-year curriculum, in which each student uses the tool to analyze and present a case in small-group sessions. To promote experiential learning, each student is tasked to identify a case from a clinical rotation in which they were directly involved. Students de-identify both the patients and the involved clinicians from their presentation. Students identify one or two “triggers” for selecting the case; these may be ethical, social, professional, or systems and policy issues. For example, one student reported being directed to assist in positioning a nonagitated patient for an injection of an antipsychotic medication. The patient had a history of a psychiatric diagnosis, the nurse had unreasonable fears of caring for the patient overnight, and the resident physician complied with the nurse’s clinically inappropriate request for a chemical restraint. The student identified the case’s racist overtones, and elucidated issues of professionalism and departures from ethical norms.
In an orienting session scheduled prior to this assignment, the faculty demonstrate the tool and mentor the students through a case analysis. To begin their case analysis using SCAT, students are directed to focus on the tile that most clearly represents what they perceive as the locus of the “trigger.” They proceed to explore neighboring tiles for content relating to the core triggers. After the students have made an initial exploration of the tool and drafted an analysis of the case, each student meets with faculty to review progress and to mentor the student on their identification of issues and the development of their analysis. Once the student has completed this part of the exercise, they are tasked with developing recommendations for improvement germane to the issues they have identified. Recommendations may be specific to the ethical and social management of the case at hand, as well as in the realm of education and training of medical students, faculty development of their role models, revisions to institutional policy, issues of organizational ethics, and systems concerns. Students are encouraged to search the relevant literature in bioethics, social sciences, review institutional policies and the law on the issues that they have identified, and to reference this material content in their presentations.
Each student presents their case, analysis, and recommendations in a small-group setting of eight students and two faculty facilitators. The 45-minute small-group presentation affords students a venue for developing skills in complex case presentation, in facilitating moral discourse and educating peers about normative ethics. Throughout the curriculum, each student presents one case and is a discussant in seven other students’ presentations. Herein, students benefit from peer-to-peer validation and moral and professional support around troubling issues and experiences; many of these experiences emerge as common and shared among students. Faculty play a critical role in students’ professional identity formation by actively nonnormalizing the untoward aspects of the hidden curriculum that are raised during the case presentation.
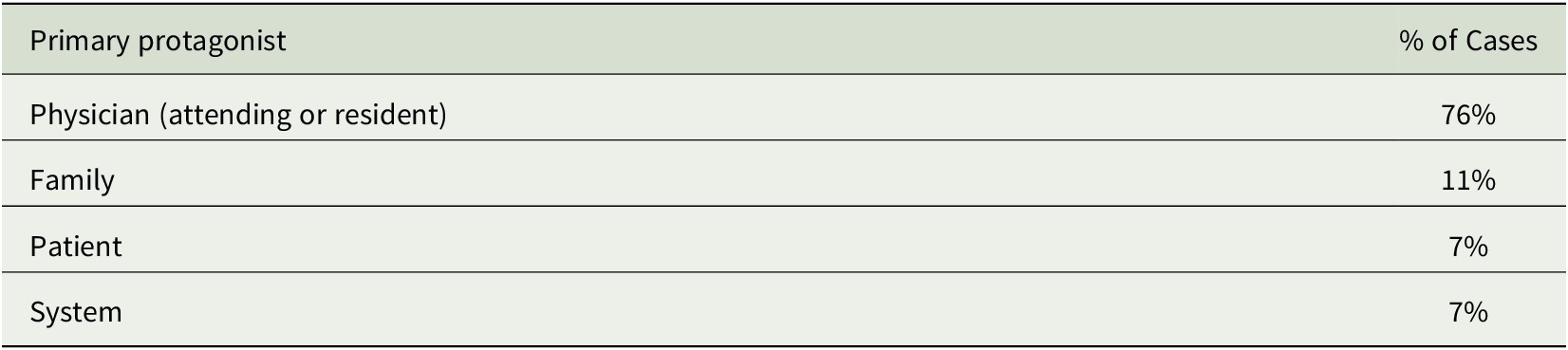
Two cohorts of 24 students have completed this exercise to date. Each cohort is the second-year class of students immersed in their core clinical clerkship. Students have identified cases from nearly all clinical areas, including general inpatient and critical care units, the operating room, emergency department, and ambulatory practices. Expectedly, and commensurate with students’ clinical assignments, most cases originate from the medical-surgical units (Table 1). Overwhelmingly, the source of the case “trigger” was a physician—either attending or resident (Table 2). Issues of professionalism predominate and were most often tied to disclosure, truth-telling, and informed consent. Other professionalism issues identified by students included poor boundaries, countertransference, problematic interpersonal behaviors, lapses in professional responsibility, departures from standard of care, violation of patient rights, and departures from ethical standards of surrogate decision-making. Nearly a quarter of cases involved issues of racism, bias, and discrimination, either as the primary or secondary issue.
Table 1. Setting/Location of Case
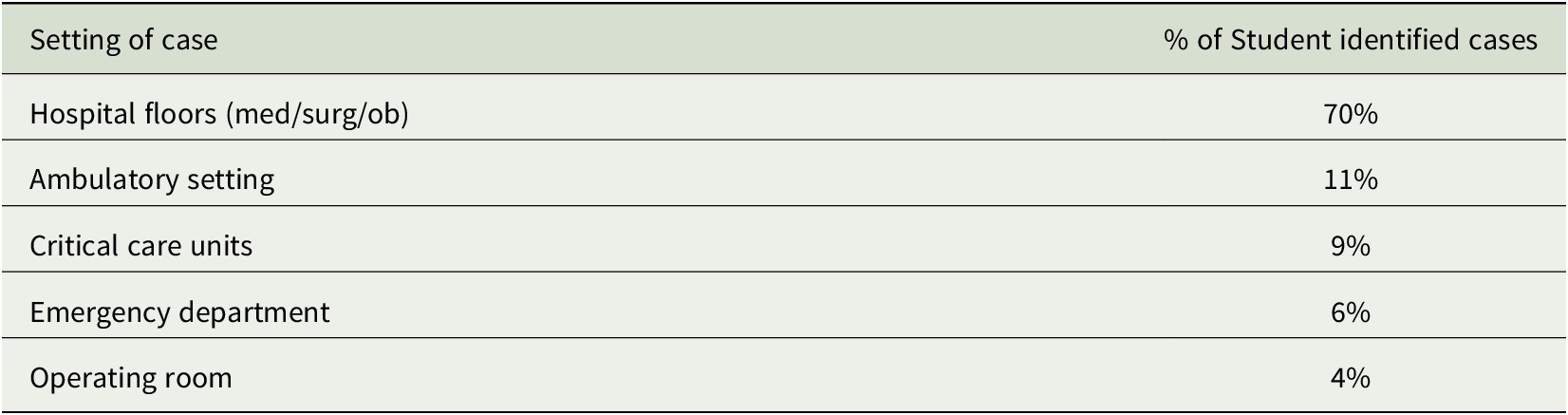
Table 2. Primary Protagonist
Student feedback and assessment
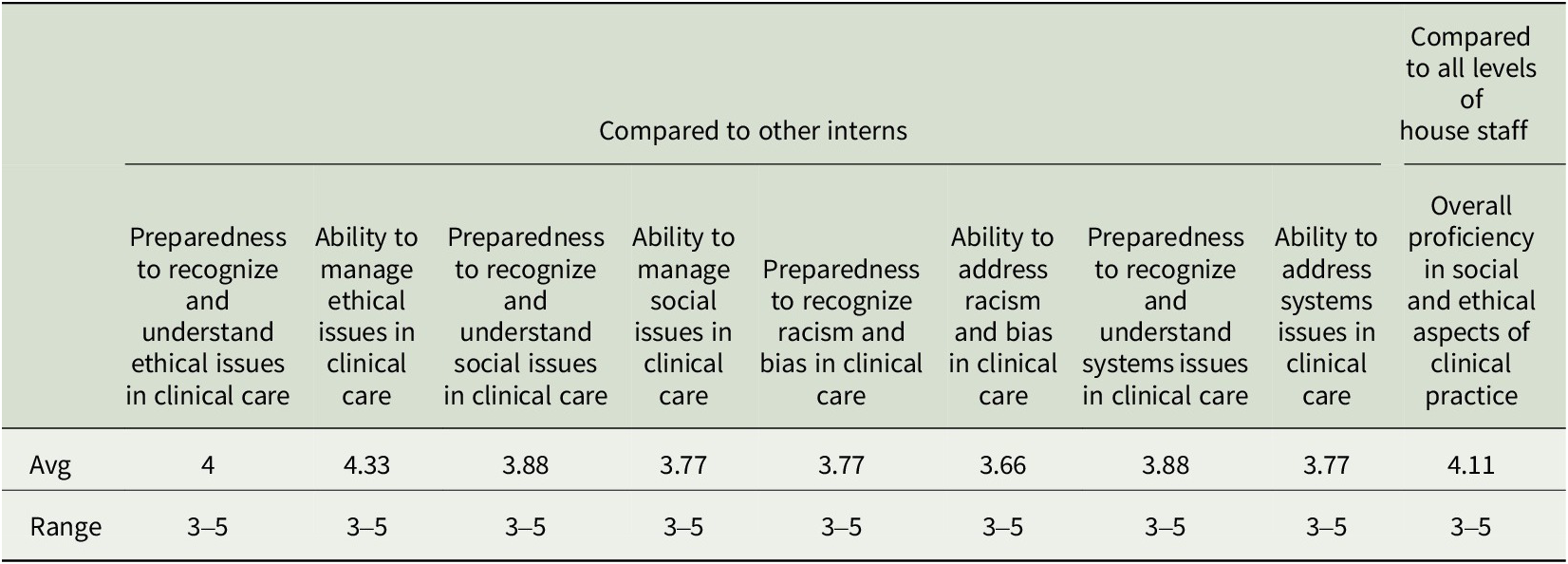
Student feedback has been strongly favorable in areas of presentation skills, analytic skills, and reinforcement of course pedagogy (Table 3). Students’ narrative feedback included “… the SCAT presentation helped me really focus on the ethical issues that are present in cases, whether or not they are obvious…this assignment really pushed me to think about changes that could be made in the ethical arena,” “The SCAT tool … helped to encourage a systematic thought process on ethical issues, and understand how the features of a case intersect and interrelate,” “It helped reinforce concepts taught last year,” and “I loved the tool once I was able to understand how to use it. I was overwhelmed at first…” In a postgraduate survey, former students (now interns), self-rated their overall efficacy in SHEP domains as generally superior to intern-peers in their training programs (Table 4).
Table 3. Student/User Assessment
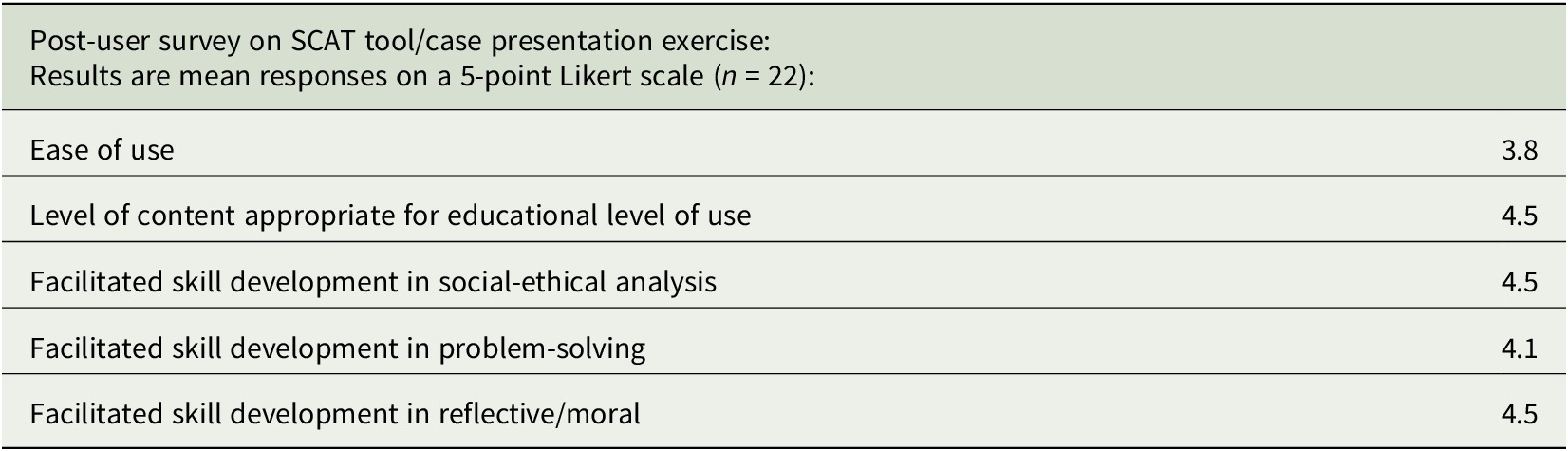
Table 4. Self-assessment of graduates in comparison to other interns in their primary residency programs
Discussion
Undergraduate education in ethics and humanities has long been atypical among other curricular imperatives in terms of consistency of content and course deliverables. Ethics and humanities education often does not translate into clinical skill development.Footnote 26 , Footnote 27 In response to these issues, the SHEP curriculum overall, and the SCAT-based exercise in particular, were developed to be outcomes-based. The course and case exercise support a richer understanding of normative ethics and sociostructural phenomena as shaped by social, sociological, historical, and political forces.
Although students in the course learn about “classic” cases in ethics, for example, Quinlan, Cruzan, and Canterbury v Spence, they sharpen their clinical skills by analyzing everyday cases, representing common social, system, and ethical issues. These case sessions provide a framework for expression of professional virtues, for calling out and rejecting negative influences of the inexplicit curriculum, for enhancing students’ ability to act with conviction from within the health system structure in accordance with professional norms and requirements, and for improving awareness of larger structural forces as part of a commitment to improving systems of care.
SCAT as a standalone device may be somewhat cumbersome for point of care use due to the number of domains it encompasses, that is, ethical, social, and organizational, among others, as well as due to the amount of content embedded in it. It may be more suitable for more deliberate and non-time-sensitive efforts to analyze complex cases. Moreover, it requires first-time users to undergo an in-service session and additional one-on-one mentoring. We continue to refine the tool having recently added structure and content pertaining to organ donation, gamete donation, and gestational surrogacy. We are in the process of trialing its use to learners outside of the SHEP course and assessing its effectiveness in terms of transmitting knowledge and improving reasoning and analytic skills. Future applications of the tool may include a mobile version.
Conclusion
Concept mapping can be adapted to education in ethics, social sciences, and related concerns. Students’ use of the tool is associated with high levels of self-assessed efficacy in understanding complex cases.









