Impact statement
Precision medicine advances have driven many welcome insights into mechanisms of disease and means to treat them. However, these advances have an environmental footprint which in turn can lead to adverse health impacts. Our article argues that precision medicine research should have an interest in this environmental footprint not only because of international priority setting, but also because of its commitment to health. We describe these impacts, focusing in particular on data intensive approaches such as those associated with the energy required to collect, store, process and analyse data, as well as the materials associated with the manufacture of digital technologies, and the waste produced from them. We point to the scant discussions of the impacts of data intensive approaches to date in the health research literature, despite a growing awareness of the importance of the need for environmental sustainability within healthcare. We highlight how the carbon footprint of certain data intensive approaches compares to – for example, airline travel-and then point to various ways in which precision medicine researchers can consider the adverse environmental and health impacts of their work. Relatively simple interventions such as considerations around where, how, and when data is stored, processed, and analysed can make a significant impact on the environmental footprint of these activities. We hope our article will be of interest to a wide range of experts involved in precision medicine including policy makers.
Introduction
Technological advances in our ability to create, link and store data relating to health have brought promises and aspirations of personalising healthcare decisions for a given patient, so that they can receive the most targeted, and therefore effective treatment (Ginsburg and Phillips, Reference Ginsburg and Phillips2018). All sorts of clinical-related data – including genomic, proteomic, other ‘omic’ and biochemical analyses – can be linked with environmental exposure data, longitudinal information from ‘wearables’ and other patient-reported data, with the aim of improving care, reducing the need for unnecessary investigations and targeting therapies more appropriately. Examples that have already entered routine clinical practice are many and varied and include the treatment of certain cancers, rare genetic conditions (e.g., cystic fibrosis and Duchenne muscular dystrophy), infectious diseases (e.g., HIV) and drug responses (e.g., warfarin and codeine sensitivity) (Ashley, Reference Ashley2016; Ginsburg and Phillips, Reference Ginsburg and Phillips2018).
These advances inevitably have a significant environmental footprint, which is sometimes justified by using consequential narratives of being necessary to improve healthcare and/or that health has intrinsic value so has a ‘free pass’ to not consider these issues (Samuel et al., Reference Samuel, Hardcastle and Lucassen2022). Nevertheless, the adverse environmental impacts of data-driven precision medicine include its effect on the climate, material environment, water and air pollution and (toxic) waste production and thus question whether this ‘free pass’ is appropriate. This article reviews the current literature associated with the environmental impacts of precision medicine, particularly focussing on the underlying data-intensive approach. It highlights that while much concern has focused on the environmental impacts of medicine more generally, less attention has been paid to the data-driven aspects of (precision) medicine. The review considers (1) the literature on environmental impacts studied in medicine, (2) the literature on environmental impacts associated with data-driven technologies and (3) the [scant] literature on environmental impacts of data-driven precision medicine. It concludes by highlighting various environmental considerations that precision medicine researchers, and the field more broadly, should take into account.
Climate change and the need to consider the environmental impacts of (precision) medicine
Calls for an environmentally sustainable medicine have been made for several decades (Pierce and Jameton, Reference Pierce and Jameton2004, Dwyer, Reference Dwyer2009, Brown et al., Reference Brown, Buettner and Canyon2012, Eckelman and Sherman, Reference Eckelman and Sherman2018, Richie, Reference Richie2019, Health Care Without Harm, 2021). Healthcare contributes to between 1% and 5% of various global environmental impacts, including greenhouse gas emissions, particulate matter, air pollutants, reactive nitrogen in water and water use (Lenzen et al., Reference Lenzen, Malik, Li, Fry, Weisz, Pichler, Chaves, Capon and Pencheon2020). Healthcare is also a massive emitter of waste, much of which is plastic, with single-use plastic items (syringes, blood bags and tubing) saturating everyday medical practice across the globe (Hodges, Reference Hodges2017). The recent COVID-19 pandemic has exemplified the issue with the generation of eight million tonnes of pandemic-associated plastic waste, primarily from hospitals (Peng et al., Reference Peng, Wu, Schartup and Zhang2021).
While the consideration of all types of environmental impacts is important, the recent categorisation of the climate emergency (Pidgeon, Reference Pidgeon2021) has driven particular and urgent attention to environmental impacts, such as carbon dioxide and greenhouse gas emissions, that contribute to climate change. There is now no doubt that climate change is caused by human factors, resulting in an increased frequency and severity of extreme temperatures, flooding, cyclones, droughts and fire weather (IPCC, 2022). Healthcare industries contribute approximately 5.5% of a country’s total emissions (as of 2014; e.g., the United States, the Netherlands, Belgium and Japan all emit approximately 8% of the country’s total emissions; it is 3.3% for Mexico and 6% for Great BritainFootnote 1) (Pichler et al., Reference Pichler, Jaccard, Weisz and Weisz2019). Without measures to tackle these consequences, we will see the extinction of species on land and in the ocean, as well as the devastation of environments (IPCC, 2022). Climate change also directly affects the social and environmental determinants of health – clean air, safe drinking water, sufficient food, water and secure shelter (cities, settlements and infrastructure) (World Health Organisation, 2021; IPCC, 2022). Climate events (heat, floods and cyclones) have affected food production and nutrition levels (what can be grown and the time that land can be farmed) – particularly in Africa and Central and South America (Romanello et al., Reference Romanello, McGushin, Di Napoli, Drummond, Hughes, Jamart, Kennard, Lampard, Rodriguez, Arnell, Ayeb-Karlsson, Belesova, Cai, Campbell-Lendrum, Capstick, Chambers, Chu, Ciampi, Dalin, Dasandi, Dasgupta, Davies, Dominguez-Salas, Dubrow, Ebi, Eckelman, Ekins, Escobar, Georgeson, Grace, Graham, Gunther, Hartinger, He, Heaviside, Hess, Hsu, Jankin, Jimenez, Kelman, Kiesewetter, Kinney, Kjellstrom, Kniveton, Lee, Lemke, Liu, Liu, Lott, Lowe, Martinez-Urtaza, Maslin, McAllister, McMichael, Mi, Milner, Minor, Mohajeri, Moradi-Lakeh, Morrissey, Munzert, Murray, Neville, Nilsson, Obradovich, Sewe, Oreszczyn, Otto, Owfi, Pearman, Pencheon, Rabbaniha, Robinson, Rocklöv, Salas, Semenza, Sherman, Shi, Springmann, Tabatabaei, Taylor, Trinanes, Shumake-Guillemot, Vu, Wagner, Wilkinson, Winning, Yglesias, Zhang, Gong, Montgomery, Costello and Hamilton2021; IPCC, 2022). Increased exposure to extreme heat, wildfire smoke, atmospheric dust and aeroallergens have been associated with climate-related cardiovascular and respiratory distress resulting in increased morbidity and mortality (Romanello et al., Reference Romanello, McGushin, Di Napoli, Drummond, Hughes, Jamart, Kennard, Lampard, Rodriguez, Arnell, Ayeb-Karlsson, Belesova, Cai, Campbell-Lendrum, Capstick, Chambers, Chu, Ciampi, Dalin, Dasandi, Dasgupta, Davies, Dominguez-Salas, Dubrow, Ebi, Eckelman, Ekins, Escobar, Georgeson, Grace, Graham, Gunther, Hartinger, He, Heaviside, Hess, Hsu, Jankin, Jimenez, Kelman, Kiesewetter, Kinney, Kjellstrom, Kniveton, Lee, Lemke, Liu, Liu, Lott, Lowe, Martinez-Urtaza, Maslin, McAllister, McMichael, Mi, Milner, Minor, Mohajeri, Moradi-Lakeh, Morrissey, Munzert, Murray, Neville, Nilsson, Obradovich, Sewe, Oreszczyn, Otto, Owfi, Pearman, Pencheon, Rabbaniha, Robinson, Rocklöv, Salas, Semenza, Sherman, Shi, Springmann, Tabatabaei, Taylor, Trinanes, Shumake-Guillemot, Vu, Wagner, Wilkinson, Winning, Yglesias, Zhang, Gong, Montgomery, Costello and Hamilton2021, IPCC, 2022). High temperatures can also reduce the frequency, duration and motivation to be physically active, in turn, a known factor in the risk of cardiovascular disease, diabetes, cancer, cognitive decline and all-cause mortality (Romanello et al., Reference Romanello, McGushin, Di Napoli, Drummond, Hughes, Jamart, Kennard, Lampard, Rodriguez, Arnell, Ayeb-Karlsson, Belesova, Cai, Campbell-Lendrum, Capstick, Chambers, Chu, Ciampi, Dalin, Dasandi, Dasgupta, Davies, Dominguez-Salas, Dubrow, Ebi, Eckelman, Ekins, Escobar, Georgeson, Grace, Graham, Gunther, Hartinger, He, Heaviside, Hess, Hsu, Jankin, Jimenez, Kelman, Kiesewetter, Kinney, Kjellstrom, Kniveton, Lee, Lemke, Liu, Liu, Lott, Lowe, Martinez-Urtaza, Maslin, McAllister, McMichael, Mi, Milner, Minor, Mohajeri, Moradi-Lakeh, Morrissey, Munzert, Murray, Neville, Nilsson, Obradovich, Sewe, Oreszczyn, Otto, Owfi, Pearman, Pencheon, Rabbaniha, Robinson, Rocklöv, Salas, Semenza, Sherman, Shi, Springmann, Tabatabaei, Taylor, Trinanes, Shumake-Guillemot, Vu, Wagner, Wilkinson, Winning, Yglesias, Zhang, Gong, Montgomery, Costello and Hamilton2021). Effects on mental health have also been documented from loss of livelihoods and culture through climate events (Romanello et al., Reference Romanello, McGushin, Di Napoli, Drummond, Hughes, Jamart, Kennard, Lampard, Rodriguez, Arnell, Ayeb-Karlsson, Belesova, Cai, Campbell-Lendrum, Capstick, Chambers, Chu, Ciampi, Dalin, Dasandi, Dasgupta, Davies, Dominguez-Salas, Dubrow, Ebi, Eckelman, Ekins, Escobar, Georgeson, Grace, Graham, Gunther, Hartinger, He, Heaviside, Hess, Hsu, Jankin, Jimenez, Kelman, Kiesewetter, Kinney, Kjellstrom, Kniveton, Lee, Lemke, Liu, Liu, Lott, Lowe, Martinez-Urtaza, Maslin, McAllister, McMichael, Mi, Milner, Minor, Mohajeri, Moradi-Lakeh, Morrissey, Munzert, Murray, Neville, Nilsson, Obradovich, Sewe, Oreszczyn, Otto, Owfi, Pearman, Pencheon, Rabbaniha, Robinson, Rocklöv, Salas, Semenza, Sherman, Shi, Springmann, Tabatabaei, Taylor, Trinanes, Shumake-Guillemot, Vu, Wagner, Wilkinson, Winning, Yglesias, Zhang, Gong, Montgomery, Costello and Hamilton2021). The occurrence of malaria, dengue fever and Zika are all on the rise because increasing climate temperatures mean the geographical area where mosquitos can survive is extended, as well as their annual season, resulting in greater disease transmission (Romanello et al., Reference Romanello, McGushin, Di Napoli, Drummond, Hughes, Jamart, Kennard, Lampard, Rodriguez, Arnell, Ayeb-Karlsson, Belesova, Cai, Campbell-Lendrum, Capstick, Chambers, Chu, Ciampi, Dalin, Dasandi, Dasgupta, Davies, Dominguez-Salas, Dubrow, Ebi, Eckelman, Ekins, Escobar, Georgeson, Grace, Graham, Gunther, Hartinger, He, Heaviside, Hess, Hsu, Jankin, Jimenez, Kelman, Kiesewetter, Kinney, Kjellstrom, Kniveton, Lee, Lemke, Liu, Liu, Lott, Lowe, Martinez-Urtaza, Maslin, McAllister, McMichael, Mi, Milner, Minor, Mohajeri, Moradi-Lakeh, Morrissey, Munzert, Murray, Neville, Nilsson, Obradovich, Sewe, Oreszczyn, Otto, Owfi, Pearman, Pencheon, Rabbaniha, Robinson, Rocklöv, Salas, Semenza, Sherman, Shi, Springmann, Tabatabaei, Taylor, Trinanes, Shumake-Guillemot, Vu, Wagner, Wilkinson, Winning, Yglesias, Zhang, Gong, Montgomery, Costello and Hamilton2021; IPCC, 2022). The World Health Organisation (WHO) predicts that between 2030 and 2050, climate change will cause approximately 250,000 additional deaths per year from malnutrition, malaria, diarrhoea and heat stress (World Health Organisation, 2021). While international efforts aim to limit global warming to 1.5°C, evidence shows that we must be prepared for warming up to 4°C (UK Government, 2022). In the UK, for example, the surface temperature has already risen by 1.2°C since pre-industrial times (UK Government, 2022).
Reducing carbon emissions and other environmental impacts of (precision) medicine
A group of 60 countries has already committed to developing climate-resilient and/or low-carbon health systems, and nine countries have now pledged to make their healthcare systems net-zero by 2040Footnote 2 (Indonesia, Malawi, Sierra Leonne, Kenya, Liberia, Ivory Coast, Burkina Faso, Nigeria and UK). Various hospitals internationally have also signed up for the United Nation-backed ‘Race to Zero’ initiative.Footnote 3 For example, in England, since 2007, the National Health Service (NHS) has reduced the carbon footprint of health and social care by 18.5% (equating to the annual emissions from a small country such as Cyprus). Carbon and energy reduction initiatives have focused on a number of levels including buildings, estates and facilities; medical infrastructure, including disposable containers (McPherson et al., Reference McPherson, Sharip and Grimmond2019); travel; and electronic devices such as freezers, lights and computers (NHS England, 2018).
Examples of areas in which the environmental impacts of specific health procedures and devices can be reduced include: imaging (Alshqaqeeq et al., Reference Alshqaqeeq, McGuire, Overcash, Ali and Twomey2020), anaesthetics (Ryan and Nielsen, Reference Ryan and Nielsen2010), inhalers (Wilkinson et al., Reference Wilkinson, Braggins, Steinbach and Smith2019), dialysis (Moura-Neto et al., Reference Moura-Neto, Barraclough and Agar2019), eye care (Buchan et al., Reference Buchan, Thiel, Steyn, Somner, Venkatesh, Burton and Ramke2022) and surgery (Namburar et al., Reference Namburar, Pillai, Varghese, Thiel and Robin2018; Thiel et al., Reference Thiel, Woods and Bilec2018), all of which can have particularly high environmental impacts.
Perhaps more pertinent to precision medicine research and manufacturing, global healthcare and technology companies are similarly decarbonising their biomedical research, as well as their manufacture of medical devices and pharmaceuticals (Pierce and Jameton, Reference Pierce and Jameton2004; Hawkes, Reference Hawkes2012; NHS England, 2018; Kmietowicz, Reference Kmietowicz2021).Footnote 4 This is important, since a recent analysis has identified the pharmaceutical industry to be significantly more emission-intensive than the automotive industry (Belkhir and Elmeligi, Reference Belkhir and Elmeligi2019). Emissions are related to upstream manufacturing and research transportation costs for drug distribution, as well as downstream prescribing (Richie, Reference Richie2021).
Developing environmentally sustainable healthcare means going beyond climate considerations to ensure natural resources are not harvested faster than they can be regenerated, or emitting waste faster than what can be assimilated by the environment (Mensah, Reference Mensah2019). The effects on biodiversity must be considered (Bull et al., Reference Bull, Taylor, Biggs, Grub, Yearley, Waters and Milner-Gulland2022), as must water consumption. For example, health services in various countries are reducing their water consumption,Footnote 5 for example, NHS England has reduced its water footprint by 21% since 2010 – the same water volume as 243,000 Olympic swimming pools (NHS England, 2018). Precision medicine research must also attend to waste from its research laboratories. Various international initiatives have encouraged laboratories to reduce consumption, and reuse and recycle materialsFootnote 6 (e.g., see Rae et al., Reference Rae, Farley, Jeffery and Urai2022 who reviewed the environmental sustainability of neuroscience research).
Environmental impacts of data-driven technologies
One aspect of precision medicine is data-driven research. Data-driven initiatives have resulted in an exponential increase in computing storage and processing power that has allowed precision medicine researchers to collect and collate myriad types of health-related data sets for analysis. Data-linkage studies, using a range of complex algorithms, such as machine learning and other artificial intelligence technologies are driving this ‘datafication’ (Ruckenstein and Schüll, Reference Ruckenstein and Schüll2017) of health (Erikainen and Chan, Reference Erikainen and Chan2019), making it the fastest growing sector in the datasphere (Reinsel et al., Reference Reinsel, Gantz and Rydning2018). Proteomics, metabolomics and genomics are all data-intensive solutions used by precision medicine researchers. Hogan (Reference Hogan2020) has emphasised that by 2025, it is predicted that between 100 million and 2 billion human genomes will have been sequenced globally, using some 40 exabytes of data (Hogan, Reference Hogan2020). The UK 100,000 genomes project uses 21 petabytes of storage, which is equivalent storage to some 40,000 years of playback on an MP3 player (Davies, Reference Davies2017). By 2025, the UK Biobank database – a leading international biobank – is expected to grow to 15 petabytes – an amount of data equivalent to that created annually by the Large Hadron Collider, though likely will be much greater than this as it continues to analyse the data it has already collected, as well as collect new data from various imaging studies.Footnote 7 Furthermore, precision medicine research of electronic health records by ML/AI techniques uses petabytes of storage (Nelson and Staggers, Reference Nelson and Staggers2018).Footnote 8
Whilst the hypothesised and proven benefits are varied, the adverse consequences of precision medicine’s environmental footprint require recognition and consideration. Digital and data-driven technologies are often described using metaphors of immateriality (connecting ‘virtually’) or fluffiness and transparency (computing in a ‘cloud’), yet their physical presence is real, comprised of a multitude of computers, servers, cables and wires (Holt and Vonderau, Reference Holt, Vonderau, Parks and Starosielski2015; Lucivero, Reference Lucivero2020). Large and expansive data centres house data servers, and physical digital infrastructures supply information and communication technologies (ICTs). And, while data centres are often portrayed in environmentally friendly ways (e.g., surrounding trees, images of clean and shiny servers) (Holt and Vonderau, Reference Holt, Vonderau, Parks and Starosielski2015), this may obscure the fact that data consumption has adverse environmental impacts (Lucivero, Reference Lucivero2020). To understand these adverse environmental impacts and how they relate to precision medicine, we start with a review of the broader literature on the environmental (and adverse health) impacts of digital technologies.
Carbon emissions
Heavy carbon dioxide emissions result from the energy required to generate and process large amounts of data. The most recent estimate of the digital sector’s contribution to global carbon emissions has been calculated between 2.1% and 3.9% (Freitag et al., Reference Freitag, Berners-Lee, Widdicks, Knowles, Blair and Friday2021). This range reflects some of the uncertainties, controversies and complexities that perplex carbon accounting in the digital sector. This includes the lack of transparency about data centre carbon emissions and the speed of technological innovation which in turn means that calculations may be based on old hardware efficiency figures. It also includes the fact that digital technologies are networks and infrastructures rather than discrete entities, meaning that carbon emissions associated with a particular device or product are difficult to measure (e.g., Horner et al., Reference Horner, Shehabi and Azevedo2016; Bieser and Hilty, Reference Bieser and Hilty2018; Koomey and Masanet, Reference Koomey and Masanet2021). Furthermore, Freitag et al. (Reference Freitag, Berners-Lee, Widdicks, Knowles, Blair and Friday2021) and Samuel et al. (Reference Samuel, Hardcastle and Lucassen2022) both point to how researchers approach carbon accounting differently depending on their discipline, relying on different assumptions and methodologies. Calculating embodied carbon emissions (those emissions associated with the manufacture and transport of digital servers, devices, equipment and servers), while possible (Whitehead and Adrews, Reference Whitehead and Adrews2015), also presents challenges because any emissions attributed to a specific digital material are likely to be entangled with those of other economic sectors (Pierce and Jameton, Reference Pierce and Jameton2004). This is particularly relevant if we consider the environmental impacts of digital technologies specifically used for precision medicine. This is because precision medicine only uses a small proportion of digital infrastructures, and so it is difficult to dis-entangle exactly what the environmental impact is for this particular field. Nevertheless some data are available for consideration. First, it has been estimated that healthcare data overall make up roughly 6% of all digital data in the datasphere, and this is only likely to increase given that it is the fastest growing sector.Footnote 9 As such, considering the environmental impacts of data-driven precision medicine is important. Second, while the environmental impacts of data-driven precision medicine – for example, those related to genomics, and/or the use of natural language processing for analysing electronic medical records – have not yet been studied to any great extent, they are likely to have energy-intensive needs. For example, the energy required to train one particular model in precision medicine research – a deep learning artificial intelligence model (BERTFootnote 10 based model without hyperparameter tuning) on a graphics processing unit (GPU) (Rasmy et al., Reference Rasmy, Xiang, Xie, Tao and Zhi2021) – has been calculated as equivalent to a trans-American flight (Strubell et al., Reference Strubell, Ganesh and McCallum2019).Footnote 11 Furthermore, a recent study calculated the energy required to conduct a genome-wide association study on biobank data for just one disease trait, to be equivalent to driving about 30 or 100 km, depending on the software used (Grealey et al., Reference Grealey, Lannelongue, Saw, Marten, Meric, Ruiz-Carmona and Inouye2021).
The digital sector has worked hard recently to drive efficiency gains.Footnote 12 Tools available to quantify the carbon footprint of a piece of software are improving (Anthony et al., Reference Anthony, Kanding and Selvan2020; Rae et al., Reference Rae, Farley, Jeffery and Urai2022) and ‘off the shelf’ energy-efficient computing hardware and software are also increasingly gaining attention (e.g., Marković et al., Reference Marković, Mizrahi, Querlioz and Grollier2020).Footnote 13 Some scholars predict that likely improvements in energy efficiency and the move to renewable energy will relieve at least some of the above concerns (Malmodin and Lundén, Reference Malmodin and Lundén2018; Giles, Reference Giles2019), with many hyperscalersFootnote 14 already at or heading to net-zero carbon use. However, Blair (Reference Blair2020) argues that the pace of data-driven innovation could outpace the world’s renewable energy sources (Blair, Reference Blair2020). Other scholars stress that it would be remiss to view renewables as a solution to the problem (Morozov, Reference Morozov2013) given that they have their own environmental impacts. For example, with their use (e.g., where they are placed, their effects on the landscape and biodiversity, as well as – for offshore wind – their potential effects on sea temperature),Footnote 15 as well as the materials used for their construction (Bihouix, Reference Bihouix2020; Mills, Reference Mills2020) especially rare mineral extraction, which is increasing rapidly to satisfy global demands (Bolger et al., Reference Bolger, Marin, Tofighi-Niaki and Seelmann2021; Voskoboynik and Andreucci, Reference Voskoboynik and Andreucci2021).
Moreover, research has explored the rebound effects of digital technologies, that is, the effects that come from improvements in efficiency. There is now a significant research literature that shows that while increases in energy efficiency may offer environmental advantages in the short term, they will also very likely lead to an increase in consumption in the longer term (Takahashi et al., Reference Takahashi, Tatemichi, Tanaka, Nishi and Kunioka2004; Alcott, Reference Alcott2005; Hilty et al., Reference Hilty, Köhler, Von Schéele, Zah and Ruddy2006; Börjesson Rivera et al., Reference Börjesson Rivera, Håkansson, Svenfelt and Finnveden2014). We see this in precision medicine, with more health data being collected stored and analysed. In fact, the collection of ever-increasing amounts of (health) data from both clinical and non-clinical (environmental, social media, passive [sleep, heart rate, etc.]) sources allows precision medicine researchers to use ever more powerful (and energy hungry) algorithms to answer endless health-related research questions. One example is digital phenotyping – a precision medicine field developed specifically because the increases in digital efficiency have allowed the collection and analysis of tremendous swaths of data. Digital phenotyping uses machine learning techniques to analyse moment-by-moment individual data from personal sensors and smartphones (social media data, sleep, location, phone records, heart rate, etc.) to improve the diagnoses for targeted intervention (Insel, Reference Insel2017). Such trends in artificial intelligence growth have led to increasing model size and energy consumption (Wu et al., Reference Wu, Raghavendra, Gupta, Acun, Ardalani, Maeng, Chang, Aga, Huang and Bai2022).
Impacts of resource extraction
The datafication of health and the move to data-driven precision medicine practices also contribute to the global demand for mineral and metal consumption associated with developing digital infrastructures. Practices associated with mineral extraction often lack regulation, particularly in low-to-middle income countries (LMICs). Mining-associated harms are numerous (Mancini et al., Reference Mancini, Eslava, Traverso and Mathieux2021) and include respiratory illness, injuries, cancers and adverse mental health. Community health risks occur through exposure to the air, water, soil and noise pollution that come from mineral extraction and (highly toxic) processing and manufacturing (Harris et al., Reference Harris, Viliani and Spickett2015; Schwartz et al., Reference Schwartz, Lee and Darrah2021). A recent global census of 406 lower-to-middle income countries’ mining-related hazardous waste sites – affecting an estimated 7.5 million people – revealed that arsenic, lead and mercury, are all strongly associated with adverse health effects, contributing more than three-quarters of the environmental risks at these sites (Caravanos et al., Reference Caravanos, Ericson, Ponce-Canchihuamán, Hanrahan, Block, Susilorini and Fuller2013). Responsible mining is now an important issueFootnote 16 legislation and ethical codes are enforced in many countries (Arvanitidis et al., Reference Arvanitidis, Boon, Nurmi and Di Capua2017; Global Reporting Initiative, 2019; Ayeh and Bleicher, Reference Ayeh and Bleicher2021) and have led to several improvements in practice (Deberdt and Billon, Reference Deberdt and Billon2021). However, poor practices also continue (Bilham, Reference Bilham2021), often attributed to gaps in the regulation (Magallón Elósegui, Reference Magallón Elósegui2020)Footnote 17 or to the fact that initiatives are often developed by powerful companies who shape the discourse and neglect important stages of the mining life cycle (Phadke, Reference Phadke2018), and who outsource responsibility ‘at a distance’ (Calvão et al., Reference Calvão, McDonald and Bolay2021; Deberdt and Billon, Reference Deberdt and Billon2021), disregard complexity (Ayeh and Bleicher, Reference Ayeh and Bleicher2021) and do not engage with the social and cultural context of the industry (Hecht, Reference Hecht2012; Mantz, Reference Mantz2018; Smith, Reference Smith2022). While health-related and other adverse mining-associated impacts are context specific and will vary depending on the type of mining, the mineral being extracted, as well as the economic, political and cultural context (Bilham, Reference Bilham2021), Samuel and Lucassen (Reference Samuel and Lucassen2022) have argued that those working in precision medicine must become more aware of these issues in order to mitigate them as much as possible.
Electronic waste (e-waste)
The digital technology sector produces a massive amount of e-waste that contains hazardous materials such as lead, cadmium, mercury and nickel, making it a major challenge for disposal, especially when the levels of many of these substances exceed permissible limits (Mmereki et al., Reference Mmereki, Li, Baldwin, Hong and Mihai2016; Rautela et al., Reference Rautela, Arya, Vishwakarma, Lee, Kim and Kumar2021). This includes the data servers and ICT digital infrastructure that is used in precision medicine. A lack of regulation associated with disposal, recycling and resource recovery (Gabrys, Reference Gabrys2012; Mmereki et al., Reference Mmereki, Li, Baldwin, Hong and Mihai2016; Lepawsky, Reference Lepawsky2018; Rautela et al., Reference Rautela, Arya, Vishwakarma, Lee, Kim and Kumar2021) means that only about one-fifth of e-wastes are formally collected and recycled globally, with a lack of clarity around what happens to the remainder, but the likelihood is that they are dumped on landfills or traded through illegal markets (Forti et al., Reference Forti, Baldé, Kuehr and Bel2020). Resource recovery from e-waste landfills is a source of livelihood and business opportunities, but unregulated and informal e-waste recycling methods (e.g., open burning, incineration, acid stripping of metals and acid baths) generate hazardous by-products that have been shown to be present at increased levels in those living around informal e-waste sites, seriously affecting their health (Gabrys, Reference Gabrys2012; Dai et al., Reference Dai, Xu, Eskenazi, Asante, Chen, Fobil, Bergman, Brennan, Sly, Nnorom, Pascale, Wang, Zeng, Zeng, Landrigan, Drisse and Huo2020; Ngo et al., Reference Ngo, Watchalayann, Nguyen, Doan and Liang2021; Singh et al., Reference Singh, Ogunseitan and Tang2021). Furthermore, Lepawsky (Reference Lepawsky2018) argues that e-waste is more than just end-of-life digital products, but also includes the solid, liquid and gaseous toxic waste that comes from the manufacturing of digital products.
Other environmental impacts
Less literature has explored the effects of digital technologies on water consumption and biodiversity, though some exist (e.g., Ristic et al., Reference Ristic, Madani and Makuch2015; Mytton, Reference Mytton2021; Lei and Masanet, Reference Lei and Masanet2022). Data centres consume water indirectly through electricity generation (often thermoelectric power) and directly through cooling the ICT equipment which generates substantial heat (and subsequent loss through evaporation) of water.Footnote 18
Precision medicine, data-driven technologies and environmental impacts
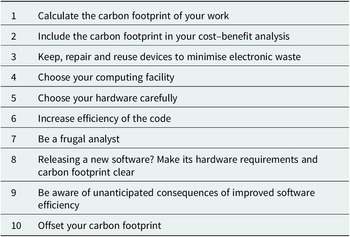
While the environmental impacts of data-driven and digital technologies have received substantial attention in the academic, policy and news media arena (Gilmore, Reference Gilmore2018; Kuntsman and Rattle, Reference Kuntsman and Rattle2019; Schwartz, Reference Schwartz2019; Department for Environment, 2021), they have received surprisingly little attention in the health sector, or in precision medicine literature. Rather, the literature has largely focused on promised benefits and increased patient autonomy (Samuel and Farsides, Reference Samuel and Farsides2017; Birk and Samuel, Reference Birk and Samuel2020). One exception is Samuel and Lucassen’s (Reference Samuel and Lucassen2022) recent mapping of the literature exploring specific environmental impacts of data-driven health research, some of which included research associated with precision medicine. These authors show how most studies have focused on developing software and hardware solutions using green IT, that is, an approach to IT that produces minimal waste during its development and operation and promotes recyclability, with less focus on a consideration of the need to think about changes in data practices (Samuel and Lucassen, Reference Samuel and Lucassen2022). This is not always the case – some scholars have highlighted what researchers and clinicians can do to decrease their environmental impact (Rae et al., Reference Rae, Farley, Jeffery and Urai2022). Scott et al. (Reference Scott, Palacios, Maturana, Mathias and Monteiro2012) take a specific focus on e-waste in the health sector, promoting reduce, reuse and recycle mottos. Tongue (Reference Tongue2019) calls for more differentiation between useful and redundant data when considering which data should be stored in a healthcare system given the environmental impacts associated with exponential increases in data collection and processing, and Chevance et al. (Reference Chevance, Hekler, Efoui-Hess, Godino, Golaszewski, Gualtieri, Krause, Marrauld, Nebeker, Perski, Simons, Taylor and Bernard2020) have called for ‘digital temperance’ rather than ‘overconsumption and overpromotion’ of data in health systems. These latter authors have described three guiding principles to be incorporated into any health-related data-relevant practices: (1) restraint in production, use and promotion of digital technologies; (2) lifecycles instead of waste (cf. the circular economy); and (3) complex systems approaches through inter-disciplinary collaboration. Lannelongue et al. (Reference Lannelongue, Grealey, Bateman and Inouye2021) have proposed a series of 10 rules for health researchers to make computing more environmentally sustainable, which are listed in Table 1 (Grealey et al., Reference Grealey, Lannelongue, Saw, Marten, Meric, Ruiz-Carmona and Inouye2021). Such rules are particularly relevant to researchers working in the field of data-driven precision medicine, but as yet there has been little literature focussing on initiatives to mitigate the ever-increasing data consumption by precision medicine researchers.
Table 1. Ten rules proposed by Lannelongue et al. (Reference Lannelongue, Grealey, Bateman and Inouye2021) to help make computing for health-related purposes more environmentally sustainable

Conclusion
As healthcare and health research become increasingly ‘datafied’, assumptions remain that the use of data is ‘free’ with few or no consequences to the environment. We have brought attention to the environmental impacts of the data-intensive approaches associated with precision medicine. While such approaches only account for a small proportion of the total adverse environmental (and health) impacts associated with digital technologies more generally, and information is limited on the exact environmental impacts of data-driven precision medicine, it is still important to reflect on this in healthcare and research practices.
Data-driven precision medicine researchers need to consider what data is being collected and analysed and why, what will happen to that data, and what impact it may have on health and the environment (good and bad). As we have shown in this review, while the promise of health benefit is a laudable goal for precision medicine research, adverse health effects can also result from the environmental impacts of precision medicine technologies. Furthermore, it remains true that those most likely to benefit from precision medicine will be those less likely to be harmed by the environmental risks attached to it and vice-versa.
There is a range of ways this imbalance might be re-dressed. Precision medicine researchers can ensure that their data is stored in data centres that are powered by renewable energy, and also adopt best practice in procurement and waste disposal. Progress can be seen from the fact that many data centres are already using efficient data servers, are actively moving towards net zero, and reducing other environmental impacts. Furthermore, environmentally friendly data storage solutions can be found in long-term data storage, which has longer data accessibility speeds, but significantly lower energy costs. Researchers should consider differentiating their data in terms of storage needs so that data that is not anticipated for short-term use can be stored at lower energy costs. Finally, precision medicine researchers developing their own algorithms must be diligent in their research methods to ensure algorithms are only run once they have been carefully checked and piloted. A range of carbon trackers that allow researchers to estimate the carbon emissions associated with their algorithms can help build awareness around the issues.Footnote 19 The field of precision medicine must also think more broadly about how to ensure the adverse and beneficial environmental/health impacts of the field are more evenly distributed. This can involve, for example, developing research questions that have (more) global relevance, and for which any potential beneficial health impacts have been considered early in the research process in terms of their global (and national) affordability and accessibility (Samuel and Richie, Reference Samuel and Richie2022). Finally, at a policy level, high-energy-consuming technological solutionism through precision medicine must be explicitly balanced with low-tech (and energy) health solutions, such as those that address the social determinants of health. Social science research has long shown that these social determinants of health play a far greater role in health outcomes than a country’s technological clinical capabilities (Institute of Medicine (US) Committee on Assuring the Health of the Public in the 21st Century, 2002). Furthermore, increasing the efficiency of digital solutions should not be viewed as a free pass towards continued consumption, but rather efficiency should be viewed as providing the necessary space between society’s consumption and the need not to overshoot planetary boundaries (forthcoming). Overall, there is a range of practices that precision medicine researchers, as well as policymakers, should consider to help balance the benefits and adverse environmental impacts of precision medicine.
Open peer review
To view the open peer review materials for this article, please visit http://doi.org/10.1017/pcm.2022.1.
Data availability statement
Data availability is not applicable to this article as no new data were created or analysed in this study.
Author contributions
G.S. wrote the first draft of the manuscript. A.M.L. reviewed and edited the draft.
Financial support
This work was supported by the Wellcome under Grant number: 222180/Z/20/Z and 205339/A/16/Z.
Competing interests
The authors declare no competing interests exist.
Ethics standards
Not applicable, because this article does not contain any studies with human or animal subjects.



Comments
Dear Editors,
Upon invite, we have now written our review for the first issue of Precision Medicine, entitled, The environmental impact of data-driven precision medicine initiatives, for publication in Precision Medicine.
Kind Regards
Gabby and Anneke