Vitamin D is a fat-soluble vitamin derived from endogenous production in the skin that can be obtained either from the diet or by exposure to ultraviolet B from sunlight with a wavelength of 290–315 nm(Reference Zhou, Zhou and Zhang1). The active form of vitamin D is calcitriol or 1,25-dihydroxyvitamin D3 (1,25(OH)2D3). Vitamin D is essential for optimal intestinal calcium (Ca) absorption to support the regulation of Ca homeostasis for bone health and phosphorus metabolism(Reference Khazai, Judd and Tangpricha2). Vitamin D also has a role in inflammatory response and influences immunity at various stages, such as antibacterial response, antigen presentation and regulation of adaptive and innate immunity(Reference Dimitrov and White3).
Vitamin D intake is reported to be associated with oral health status such as periodontal conditions(Reference Amano, Komiyama and Makishima4), oral cancer(Reference Grimm, Cetindis and Biegner5), tooth mineralisation(Reference Zhang, Beck and Rahemtulla6) and tooth loss(Reference Zhan, Samietz and Holtfreter7). Vitamin D receptor play an important role in maintaining oral health, as it is also reported to be associated with periodontal disease progression(Reference Amano, Komiyama and Makishima4). Mostly periodontal status has been assessed by bleeding on probing (BOP), pocket depth (PD), gingival bleeding, clinical attachment loss (CAL) and alveolar bone loss. Vitamin D along with Ca are considered as one of the important factors in ensuring good oral health(Reference Antonenko, Bryk and Brito8). Studies also reported that those with high vitamin D serum level had lower number of teeth with periodontal pockets(Reference Antonoglou, Suominen and Knuuttila9), decreased risk of tooth loss(Reference Zhan, Samietz and Holtfreter7) and better periodontal conditions(Reference Alshouibi, Kaye and Cabral10).
In addition, a systematic review on clinical controlled trials that were conducted on children reported that vitamin D supplement was associated with a reduced risk of caries among the children(Reference Hujoel11). There are a significant number of cross-sectional studies about oral health and vitamin D among the adults’ population. However, there is no systematic review of clinical trials was conducted on adults with regards to the vitamin D supplements and oral health. Therefore, this comprehensive review aimed to explore clinical trial data about the effect of vitamin D on oral health among the adult population.
Methodology
Information sources and search strategy
An electronic database search was performed using PUBMED, World of Science, Scopus, The Cochrane Library, OVID, Proquest and Ebcohost. There was no limit on the date retrieved and it was based on the databases that have a link with the institutions. The PICO model was used to define the review questions. The population group of this review was adults, and the Interventions were related to vitamin D administration. The comparison was placebo or control intervention group(s), and the outcomes measures were oral health parameters.
The search terms were based on and adapted from previous reviews related to vitamin D and oral health(Reference Hujoel11–Reference Chung, Balk and Brendel13). The related MESH words were also used in the search. The keywords for vitamin D were vitamin D OR plasma vitamin D OR 25-hydroxy vitamin D OR plasma vitamin D OR 25-hydroxycholecalciferol OR 25hydroxyergocalciferol OR calcidiol OR calcifediol OR ergocalciferol OR cholecalciferol OR calciferol OR 25-hydroxycholecalciferol vitamin D OR 25-hydroxycholecalciferol vitamin D3 OR 25-hydroxyvitamin D OR 25-hydroxyvitamin D3 OR 25(OH)D OR 25(OH)D3 OR 1,25(OH)2D OR 25-hydroxyvitamin D. Meanwhile, the keywords used for oral health were broader, to ensure its cover most of the related area. Examples of the keywords used in the search were dental health OR oral health OR dental hygiene OR mouth diseases OR oral cancer OR plaque control OR dental deposit OR periodontal pocket OR oral mucositis OR dry mouth OR facial pain OR halitosis. Related articles from reference lists were manually searched for potential papers that met inclusion criteria.
Study screening and selection
All the titles retrieved from the search were screened by two reviewers (NAM and KM). If there was a doubt regarding the title, the abstract was read. If there was disagreement between the two reviewers, discussion and consensus was achieved with a third reviewer (NR). Potentially relevant articles related to the vitamin D and oral health were included for further screening. Duplicated papers were identified and removed. The titles and type of studies were grouped accordingly. The inclusion criteria for the search were randomised controlled trials studies relating to both ‘Vitamin D intervention (s)’ and ‘oral health’. Studies performed on animals, review papers and those not in the English language were not selected for this review. Following this, the full texts of the effective articles were retrieved and analysed. Data were extracted based on: (i) study profile (such as year and country of the study, study setting and sample size), (ii) method of assessment and outcome(s), (iii) intervention (mode, dosage, frequency, duration and additional intervention) and (iv) key findings (Table 1).
Table 1. Details of the studies

BOP, bleeding on probing; CAL, clinical attachment loss; PD, pocket depth.
Data items
For each study, information on the oral assessments indicators and vitamin D were retrieved. The oral assessments included were (i) periodontal conditions, (ii) bone loss or bone gain and (iii) tooth retention. The vitamin D levels and dosage were also obtained from each study. The measurement was standardised to the International Unit (μg) or USA Pharmacopeia (USP).
Study quality and risk of bias assessment
The studies quality (‘quality of reporting’) was assessed and quantified using the Consolidated Standards of Reporting Trials (CONSORT) checklist(Reference Moher, Hopewell and Schulz14). The studies were rated across twenty-five items. The studies’ risk of bias was assessed using the Cochrane revised tool for assessing the risk of bias in randomised trials (RoB 2)(Reference Sterne, Savović and Page15). The following parameters were used to assess the bias: (i) randomisation process, (ii) deviations from intended interventions, (iii) missing outcome data, (iv) measurement of outcome and (v) selection of the reported result.
Synthesis of vitamin D effectiveness
Qualitative synthesis of interventions in terms of (i) serum vitamin D levels, (ii) dental plaque levels (oral hygiene and plaque index scores), (iii) gingival health status (bleeding on probing (BOP) and gingival index (GI) scores), (iv) periodontal PDs, (v) clinical attachment loss (CAL) is a distance from the cemento-enamel junction to the bottom of clinical pocket, (vi) bone attributes- alveolar bone levels, infrabony defects and bone loss and (vii) others – number of dental caries and periodontal inflamed surface area scores. Quantitative synthesis was not employed because of heterogeneity among studies in terms of vitamin D intervention and in terms of the outcome of studies.
Results
A total of 1812 studies were identified from the initial search. Duplicated studies were identified and removed (n 310). Two independent reviewers screened all the remaining studies (n 1502). Following this, 1427 studies were excluded due to unmet inclusion criteria (45 were animal/laboratory-based studies, 16 were review papers and 1366 not related to vitamin D interventions relating to oral health). Full texts of the seventy-five potentially effective studies were retrieved and screened by two independent reviewers for eligibility. The seventy studies were excluded because one study was a review, three studies were laboratory, sixteen studies were not related to ‘Vitamin D and oral health’, eighteen studies were excluded because of age (studies among children aged ≤ 18) and thirty-two studies were excluded because of study design (twenty-one cross-sectional studies, eight case study and three cohort studies). One additional study was identified through the reference linkage from the reference lists of studies screened. Finally, six ‘effective studies’ met the inclusion criteria to inform this review and synthesis of the studies’ findings was performed. The study screening and selection process was summarised in Fig. 1 (PRISMA flow diagram of the screened articles). Table 1 describes the details of the six papers that met the inclusion criteria.
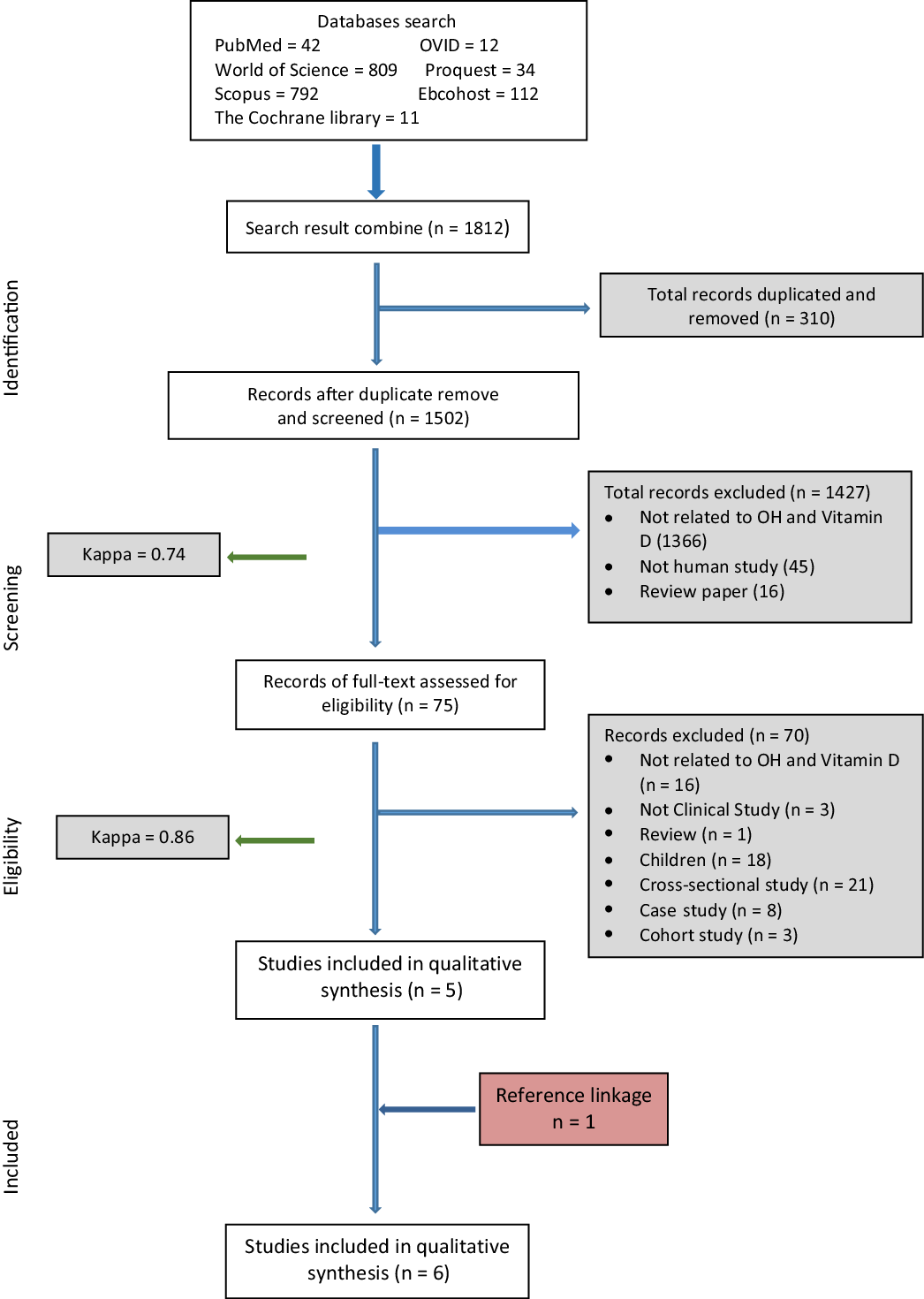
Fig. 1. PRISMA flow of the review process.
Studies characteristics
Among the six studies, five studies were published between the year 2001 and 2017(Reference Woelber, Bremer and Vach16–Reference Krall, Wehler and Garcia20). The study from the reference linkage was published in 1979(Reference Wical and Brussee21). Half (50·0 %, n = 3) of the studies were performed in the USA(Reference Bashutski, Eber and Kinney19–Reference Wical and Brussee21), one in Europe (Germany)(Reference Woelber, Bremer and Vach16) and two studies in Asia (Indian and Pakistan)(Reference Khan, Ahmad and Hussain17,Reference Hiremath, Rao and Naik18) . Most studies were performed in the clinical (dental) setting (83·3 %, n = 5)(Reference Woelber, Bremer and Vach16,Reference Hiremath, Rao and Naik18–Reference Wical and Brussee21) , and one study was a community-based study among pregnant women(Reference Khan, Ahmad and Hussain17). These six trials involved a total of 419 participants out of 443 recruited participants. The dropout rate ranged from approximately 0 %(Reference Bashutski, Eber and Kinney19,Reference Krall, Wehler and Garcia20) to 23 %(Reference Wical and Brussee21). Test group (vitamin D intervention) sample size ranged from 11(Reference Woelber, Bremer and Vach16) to 82(Reference Krall, Wehler and Garcia20). Control group sample sizes ranged from 5(Reference Woelber, Bremer and Vach16) to 63(Reference Krall, Wehler and Garcia20). Duration of the studies varied: 8 weeks(Reference Woelber, Bremer and Vach16), 3 months(Reference Hiremath, Rao and Naik18), 6 months(Reference Khan, Ahmad and Hussain17), 12 months(Reference Bashutski, Eber and Kinney19,Reference Wical and Brussee21) and 5 years(Reference Krall, Wehler and Garcia20). The age of the subjects ranging from minimum of 23 years old to maximum age of 79 years old.
The studies involved investigations on the effects of vitamin D supplementation on the periodontal status(Reference Woelber, Bremer and Vach16–Reference Hiremath, Rao and Naik18), alveolar bone loss(Reference Bashutski, Eber and Kinney19,Reference Wical and Brussee21) and tooth retention(Reference Krall, Wehler and Garcia20), as well as the vitamin D serum levels(Reference Khan, Ahmad and Hussain17,Reference Hiremath, Rao and Naik18) . The type of subjects varied among the studies, namely dental patients with gingivitis(Reference Woelber, Bremer and Vach16), pregnant women(Reference Khan, Ahmad and Hussain17), subject from dental college clinic (did not specify the type of clinic)(Reference Hiremath, Rao and Naik18), patients with severe periodontal disease scheduled for open flap debridement surgery(Reference Bashutski, Eber and Kinney19), healthy adults with bone loss from the hip study(Reference Krall, Wehler and Garcia20) and patients who had undergone extraction for an immediate denture(Reference Wical and Brussee21).
Study intervention(s)
All patients in the experimental group received supplementation of vitamin D but of different dosages and of different types of delivery modes; modified diet with 500 μg vitamin D and sun exposure of 15 min(Reference Woelber, Bremer and Vach16), 4000 μg vitamin D supplement daily(Reference Khan, Ahmad and Hussain17), 2000 μg, 1000 μg and 500 μg of vitamin D daily(Reference Hiremath, Rao and Naik18), subcutaneous injection of teriparatide (20 μg) with Ca (1000 mg) and vitamin D oral supplements (800 μg)(Reference Bashutski, Eber and Kinney19), vitamin D (≥ 400 μg/d) and Ca (≥ 1000 mg/d) supplement, Ca (500 mg/d) and vitamin D (700 μg/d)(Reference Krall, Wehler and Garcia20) and 750 mg of calcium carbonate and 375 μg units of vitamin D(Reference Wical and Brussee21).
In two-third of the studies (66·6 %, n = 4), the control groups received placebo tablets (typically microcrystalline cellulose and lactose)(Reference Khan, Ahmad and Hussain17,Reference Hiremath, Rao and Naik18,Reference Krall, Wehler and Garcia20,Reference Wical and Brussee21) . In one study, the control group was assigned to follow their usual diet (unmodified)(Reference Woelber, Bremer and Vach16). Meanwhile, in the study of Bashutski et al. (Reference Bashutski, Eber and Kinney19), both the experimental and the control groups were given the same vitamin D supplements (and of similar dose) but the control group received a placebo subcutaneous injection whereas the test group received teriparatide injection.
Outcome measures
The primary outcomes for the studies were bleeding on probing(Reference Woelber, Bremer and Vach16), periodontal disease(Reference Khan, Ahmad and Hussain17), GI and serum vitamin D level(Reference Hiremath, Rao and Naik18), infrabony defect(Reference Bashutski, Eber and Kinney19), tooth loss(Reference Krall, Wehler and Garcia20) and alveolar bone loss(Reference Wical and Brussee21). Three of the studies used clinical oral indicators and blood samples serum of vitamin D(Reference Khan, Ahmad and Hussain17–Reference Bashutski, Eber and Kinney19), and the other studies used oral assessment with either a radiographic assessment(Reference Bashutski, Eber and Kinney19,Reference Wical and Brussee21) or a questionnaire(Reference Krall, Wehler and Garcia20). The questionnaire was related to tooth loss(Reference Krall, Wehler and Garcia20) and/or daily diet(Reference Woelber, Bremer and Vach16,Reference Krall, Wehler and Garcia20) . One study used three parameters; oral indicators, blood samples and radiographic assessment(Reference Bashutski, Eber and Kinney19). The oral indicators that were commonly used were the bleeding on probing, GI, plaque index, probing depth and clinical attachment loss. Other oral indicators were alveolar bone loss, periodontal inflamed surface area (PISA), DMFT (Decay, Missing, Filled, Teeth) and tooth loss.
Synthesis of results
Periodontal conditions
(i) Bleeding on probing
Two studies assessed the bleeding on probing (BOP) status(Reference Woelber, Bremer and Vach16,Reference Bashutski, Eber and Kinney19) . Both studies reported a significant reduction of BOP at the end of the study. In one of the studies, subjects were given 500 μg vitamin D daily, along with sun exposure and other dietary intake changes - significant difference between the test and control group were observed (P < 0·05)(Reference Woelber, Bremer and Vach16). The other study reported that within the test groups, a significant reduction was observed in the BOP at 12 months, ranging from 12 % to 36 % for vitamin D deficient (P < 0·01) and vitamin D sufficient (P < 0·01) supplied with 800 μg vitamin D supplements(Reference Bashutski, Eber and Kinney19). However, there was no significant difference in BOP between the groups. Whereas in the control groups, a reduction in BOP was observed but there were no significant difference between and within the groups at the end of 12 months.
(ii) gingival index
Two studies assessed GI scores(Reference Woelber, Bremer and Vach16,Reference Hiremath, Rao and Naik18) . Both studies showed a significant reduction in the GI scores. The subjects were given 500 μg vitamin D daily, were exposed to sun exposure and given other dietary intake changes - significant difference between the test and control group were observed (P < 0·01)(Reference Woelber, Bremer and Vach16). Meanwhile, the other study demonstrated a significant improvement in the GI score for all test groups that received vitamin D supplements. All dosage 500 μg, 1000 μg and 2000 μg showed significant reduction after 90 days (P < 0·001) compared with the placebo group (P > 0·05). In addition, the serum vitamin D levels were significantly increased monthly in all experimental groups. The anti-inflammatory effects were seen earlier with a higher dosage of Vitamin D. The experimental group with the highest dosage of vitamin D supplementation, i.e. 2000 μg had a mean serum level increased of ∼10·0 ng/ml (P < 0·001) and a mean change of GI scores of –0·63 ± 0·09 after 30 d. Meanwhile, the other groups with vitamin D supplementation of1000 μg had a mean serum level increased of ∼5·6 ng/ml (P < 0·001) and a mean change of GI scores of –0·38 ± 0·01, and 500 μg had a mean serum level increased of ∼4·3 ng/ml and a mean change of GI scores of –0·28 ± 0·01 after 30 days. The increased dose of vitamin D was directly proportional to the serum vitamin D level and to lower GI scores.
(iii) plaque index
One study assessed the plaque index scores(Reference Woelber, Bremer and Vach16), however no significant difference was observed between the test and control group (P > 0·05). There was also no significant difference within the test group (a minimal reduction occurred with mean scores: 0·88 ± 0·48 to 0·84 ± 0·47), while increased plaque index scores were observed in the control group.
(iv) pocket depth
Three studies assessed the PD(Reference Woelber, Bremer and Vach16,Reference Khan, Ahmad and Hussain17,Reference Bashutski, Eber and Kinney19) . All studies showed a reduction in PD scores, but the changes were not significant at the end of study, between the test and control group in two studies(Reference Woelber, Bremer and Vach16,Reference Khan, Ahmad and Hussain17) . A reduction was observed in one study from baseline to 6 months, but there were no significant differences(Reference Khan, Ahmad and Hussain17). Another study showed significant reduction within the test groups, with vitamin D sufficient having greater PD reduction than the vitamin D deficient (P < 0·01) at all time points (3 months, 6 months and 9 months). There was no significant reduction observed between the groups at 12 months. Meanwhile, within the control groups, no significant difference was observed between the groups at all time points (P > 0·05). A significant reduction was observed in vitamin D sufficient compared with vitamin D deficient at 12 months (P < 0·01)(Reference Bashutski, Eber and Kinney19).
(v) Clinical attachment loss
Three studies assessed clinical attachment loss(Reference Woelber, Bremer and Vach16,Reference Khan, Ahmad and Hussain17,Reference Bashutski, Eber and Kinney19) . There was no significant improvement observed in two of the studies, either between the groups or within the groups(Reference Woelber, Bremer and Vach16,Reference Khan, Ahmad and Hussain17) . One study showed significant clinical attachment loss gain in vitamin D sufficient group compared with the vitamin D deficient group at 6 months (P < 0·01), but there was no significant improvement at 12 months between the groups (P > 0·05). However, within the control groups, there was a significant improvement of clinical attachment loss at 12 months in vitamin D sufficient compared with the vitamin D deficient (P < 0·01).
(vi) periodontal inflamed surface area
One study assessed the periodontal inflamed surface area score(Reference Woelber, Bremer and Vach16). Vitamin D dosage of 500 μg daily with sun exposure and other dietary intake changes reported a significant difference between the test and control group at the end of the study (P < 0·001). The test group inflammation area was reduced significantly, while the control group inflammation area increases at the end of the study.
Tooth loss
One study assessed the number of teeth lost(Reference Krall, Wehler and Garcia20). The subjects were given 700 μg vitamin D daily for 3 years, in combination with calcium citrate (500 mg) daily. There was a significant difference in tooth loss between the test and control group at three years (P < 0·05); the prevalence of tooth loss in the test group was 13 % and 27 % in the control group. Although there was a significant difference in tooth loss between the groups at follow-up, only Ca intake was significantly associated with odds of tooth loss during follow-up (OR = 0·5; 95 % CI:0·2, 0·9, P < 0·05). The Ca and vitamin D supplements were associated with a lower risk of tooth loss in older adults and women (OR 0·4; 95 % CI: 0·2, 0·9; P < 0·05). The control group (without the Ca and vitamin D supplements) lost one or more teeth compared with the test group during the study.
Alveolar bone loss
Two studies assessed the alveolar bone loss using radiographic assessment following periodontal surgery(Reference Bashutski, Eber and Kinney19) and tooth extraction(Reference Wical and Brussee21). Both studies showed that Ca and vitamin D helps to reduce the process of bone loss following the extraction with increased bone gain after periodontal surgery. The differences between the groups in both studies were still significant at follow-up assessment of 12 months. One study showed that within the test group, the vitamin D sufficient, there was significant radiographic linear bone gained compared with vitamin D deficient at 6 months, 9 months and 12 months (P < 0·05). However, no significant difference changes were observed at all time points within the control groups. While the other study showed a significant reduction in bone loss following extraction of teeth and immediate denture placement in the test group compared with the control group (P < 0·01). The participants in the test group were given 750 mg of Ca and 375 USP (or μg) units of vitamin D. The bone loss in the experimental group was less compared with the control group; 12·7 ± 5·2 mm2 and 19·8 ± 8·3 mm2, respectively. The percentage of the difference between the test and control group was 39 % less bone resorption in the mandible and 32 % less bone resorption in the maxilla.
In summary, two studies(Reference Woelber, Bremer and Vach16,Reference Hiremath, Rao and Naik18) that provided the same amount of vitamin D (500 μg) showed a significant reduction in GI scores at follow-up assessment. Three studies prescribed Ca and vitamin D, and the dosage varied from 375 μg to 800 μg(Reference Bashutski, Eber and Kinney19–Reference Wical and Brussee21). Thus, no comparison can be performed. Two of the studies investigated the alveolar bone area using radiographic evaluations(Reference Bashutski, Eber and Kinney19,Reference Wical and Brussee21) .
Quality of reporting of studies
The percentage of items reported using CONSORT ranged from 49 %(Reference Wical and Brussee21) to 73 %(Reference Khan, Ahmad and Hussain17) (Table 2). There were five unreported items for all the studies namely; changes to trial outcomes, interim analyses and stopping guidelines, changes to methods after trial commencement, the reason of the trial ended, and presentation of absolute and relative effect sizes. Three of the trials did not mention the randomisation in their title(Reference Bashutski, Eber and Kinney19–Reference Wical and Brussee21). There was only one trial reported on the following items: the type of randomisation(Reference Khan, Ahmad and Hussain17), description on the similarity of interventions(Reference Bashutski, Eber and Kinney19) and the availability of the full trial protocol(Reference Bashutski, Eber and Kinney19).
Table 2. CONSORT checklist for clinical trial studies

Risk of bias
Four of the studies (67 %) had low risk of bias arising from randomisation process(Reference Hiremath, Rao and Naik18–Reference Wical and Brussee21) and due to missing outcome data(Reference Woelber, Bremer and Vach16,Reference Khan, Ahmad and Hussain17,Reference Krall, Wehler and Garcia20,Reference Wical and Brussee21) . Five studies (83 %) had low risk of bias due to deviation from intended intervention and due to measurement of the outcome(Reference Woelber, Bremer and Vach16–Reference Hiremath, Rao and Naik18,Reference Krall, Wehler and Garcia20,Reference Wical and Brussee21) . With regards to selection of the reported result, three of the studies had low risk of bias(Reference Woelber, Bremer and Vach16,Reference Khan, Ahmad and Hussain17,Reference Wical and Brussee21) , two studies had some concern(Reference Hiremath, Rao and Naik18,Reference Bashutski, Eber and Kinney19) and one had high risk of bias(Reference Krall, Wehler and Garcia20). The low risk of bias for the domains in all studies ranged from 20 % to 100 %, A study by Wical et al. (1979) has the highest percentage of low risk of bias and Batshutski et al. (2011) had the lowest percentage of low risk of bias. Four out of the five domains in Batshutski study were in some concern category (Table 3).
Table 3. Risk of bias

Discussion
This systematic review revealed that there was still insufficient evidence to support a positive relationship between vitamin D and oral health. Although the systemic search has retrieved many studies with regards to vitamin D and oral health, most of the studies were cross-sectional or observational studies. Higher-quality studies are required to assess the optimal dosage of vitamin D in relation to oral health. The reviewed papers were varied in terms of intervention(s) (mode of administration, dosage, frequency of use, duration) and outcomes.
In general, the systematic review revealed that vitamin D supplements with different dosages, mode of administration, duration and in combinations with other interventions (most notably Ca) showed a significant improvement in the outcomes measures, namely, periodontal health parameters, serum level of vitamin D, reduced bone loss, bone gain and tooth loss. The lowest dosage was reported by a study of Wical & Brussee (1979) which showed a significant reduction in alveolar bone loss associated with the intake of Ca and 375 USP of vitamin D. However, parameters such as serum level and periodontal conditions were not assessed in the study. The finding was in agreement with a study by Bashutski et al. (2011) that showed a combination of Ca and vitamin D improved linear bone gain. Another study by Krall et al. (2001) reported that tooth retention could be improved with Ca and vitamin D supplements. In addition, a study by Bashutski et al. (2011) also showed that sufficient vitamin D level (> 20 ng ml) at baseline was essential to enhance the bone gaining effects, improved PD, clinical attachment loss and BOP. Meanwhile, those studies with the lowest intake of Vitamin D (i.e. 500 μg) showed significant improvement of GI scores. Thus, it indicated that 500 μg would be the recommended dosage to maintain gingival health, and a combination of Ca and vitamin D would help to maintain bone level. Studies also showed that an increased dosage of vitamin D significantly increased the serum level of vitamin D. The review also revealed that the higher the dosage of vitamin D, the earlier the effect can be seen in the serum level and anti-inflammatory effect(Reference Khan, Ahmad and Hussain17,Reference Hiremath, Rao and Naik18) .
The importance of sunlight exposure for the synthesis of vitamin D by the skin was well established. The benefit may override the harmful effects, provided there is no excessive exposure to the sunlight(Reference Serrano22). The use of high sunscreens protection with high UV may compromise the serum vitamin D level(Reference Passeron, Bouillon and Callender23). However, daily or recreational sunscreen was not shown to compromise serum vitamin D level. There was only one study in this review that considered a sun exposure for the interventions group(Reference Woelber, Bremer and Vach16). However, the results of the study cannot be generalised due to small sample size and additional intake of the dietary components. Moreover, the effects were also based on the dietary elements which make it difficult to provide evidence on which elements has the most impact on the outcome’s parameters.
Studies have shown that a high dosage of vitamin D supplements was essential to reach the optimal serum level. However, the recommended target levels for vitamin D in the serum varied. A review paper reported serum vitamin D target levels ranging from 25 to 50 nmol/l or 10–20 ng/ml (corresponding to 400–800 μg daily intake of vitamin D supplementation which was varied with age)(Reference Pilz, Trummer and Pandis24). A recent review search in PubMed recommended the serum vitamin D target level (25-hydroxyvitamin D [25(OH)D] to be more than 50 nmol/l or 20 ng/ml(Reference Amrein, Scherkl and Hoffmann25). Meanwhile, a clinical practice guideline described a vitamin D deficiency when the serum level of vitamin D is below 20 ng/ml (50 nmol/l), and vitamin D insufficiency at 21–29 ng/ml (55 to 75 nmol/l)(Reference Holick, Binkley and Bischoff-Ferrari26).
Despite the importance of vitamin D, many people are not able to attain the optimal serum level of vitamin D daily. A single centre analysis study that involved approximately 610 000 patients from 136 countries reported that more than three-quarters of the patients were in the stage of serum vitamin D deficiency due to insufficient level(Reference Haq, Svobodová and Imran27). Among them, the patients who were from the United Arab Emirates, Saudi Arabia and other middle eastern countries were those who had vitamin D deficiency. Another study was conducted on approximately 1500 Saudis’ patients reported that the prevalence of female patients with vitamin D deficiency was high(Reference Kanan, Al Saleh and Fakhoury28). Although these countries typically have year-round sunshine, the low serum level of vitamin D among the population is a major concern. This could be related to their culture, religious practice and lifestyle. In addition, the serum vitamin D level also varied among people living in four different seasons. Their serum vitamin D levels were at a lower level during the winter months(Reference Raza, Syed and Ali29). Hence, the importance of vitamin D supplementations and the risk of low serum level of vitamin D should be made aware to the target population.
With regards to the quality of reporting, studies are of ‘moderate quality’. There were no details on such items in all studies; changes to trial outcomes, interim analyses and stopping guidelines, changes to methods after trial commencement, the reason the trial ended and presentation of absolute and relative effect sizes. Thus, there might be no such process during the study, or it was not reported. Nevertheless, reporting the details based on the CONSORT guideline would help to improve and guide future studies. Regarding the risk of bias within individual studies, lack and unclear information were the main contributing factors.
This review has some limitations. It is acknowledged that publication bias might have occurred during the selection of the studies from the databases. The selection was limited to English published papers and those that were available online. No authors were contacted and no papers in other languages were evaluated. However, involving more than one reviewer and using a broad search strategy helps reduce publication bias. The cross-reference of the published studies may also enhance it. In addition, the reporting of this systematic review was based on the time frames mentioned. Further updating information in the future is highly recommended. The published studies were relatively heterogenic, in particular the sample size, the intervention and outcomes of the study. Thus, the specific effects of vitamin D on oral health are not clear.
In conclusion, there are few clinical trials that have evaluated the effectiveness of vitamin D supplements to oral health. Among existing studies, there is substantial heterogeneity with respect to vitamin D interventions (mode of administration, dosages and duration of administration) and oral health outcomes assessed, as well as Ca supplementation added to the intervention. There are several shortcomings in the quality (of reporting) of studies and their risk of bias. Nonetheless, qualitative synthesis indicates some evidence to support the provision of vitamin D supplements for periodontal health. Further, high-quality clinical trials related to vitamin D interventions are warranted to provide a quantitative synthesis of their effectiveness.
Acknowledgments
The authors would like to thank the USIM library staff; Encik Lukman Anwar Arifin for his help in assisting and guiding the author to perform the search strategy, and Puan Sharifah Norabidzah Nurul Aida for assisting us with the article search. The authors also would like to thank Mrs Samantha Kar Yan Li for assisting us in the analysis.
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
N. Ab M. - formulating the research question(s), designing the study, carrying out the study, analysing the data, interpreting the findings and writing the article. S. M. Y. - formulating the research question(s) and designing the study. K. N. M. - carrying out the study and analysing the data. S. N. R. Md R. - carrying out the study and analysing the data. W. L. D. - analysing the data and interpreting the findings. G. P. - analysing the data and interpreting the findings. C. McG. - analysing the data, interpreting the findings and writing the article.
There are no conflicts of interest.







