Abdominal obesity is a strong predictor of metabolic disorders and premature mortality( Reference Cameron, Dunstan and Owen 1 , Reference Fox, Despres and Richard 2 ). Therefore, increasing secular trends of abdominal obesity in recent decades( Reference Ford, Mokdad and Giles 3 ) and the recently reported high prevalence of abdominal obesity( Reference Ford, Mokdad and Giles 3 , Reference Gutierrez-Fisac, Guallar-Castillon and Leon-Munoz 4 ) are a matter of health policy concern.
Sedentary lifestyle and dietary patterns promoting energy overconsumption are considered to be the main drivers of the obesity epidemic( Reference Apovian 5 ). Epidemiological evidence indicates an inverse association between adherence to the Mediterranean diet and general obesity( Reference Romaguera, Norat and Vergnaud 6 , Reference Buckland, Bach and Serra-Majem 7 ). However, little is known about the impact of this dietary pattern, which includes foods characteristic of the Mediterranean olive grove areas, on abdominal fat accumulation( Reference Rallidis, Lekakis and Kolomvotsou 8 ). An inverse association has been found in some( Reference Romaguera, Norat and Mouw 9 ) but not in all( Reference Asghari, Mirmiran and Rashidkhani 10 ) cross-sectional studies, and long-term prospective data are lacking.
Most studies have measured adherence to the Mediterranean diet by scores based on consumption patterns and modified to reflect the particular study population. This approach makes it difficult to compare results between different populations( Reference Kesse-Guyot, Ahluwalia and Lassale 11 ). A Mediterranean diet score has also been created a priori by a few studies( Reference Rumawas, Dwyer and McKeown 12 ), using food intake recommendations.
The present study had three objectives: (1) to explore the prospective association of adherence to the Mediterranean diet with waist circumference (WC) changes; (2) to determine the 10-year incidence of abdominal obesity defined by WC cut-offs, according to adherence to the Mediterranean diet in a population-based sample in Spain; (3) to assess whether the use of a different strategy to define the Mediterranean diet construct had an impact on the results obtained.
Materials and methods
Study population
Data were obtained from a population-based survey conducted in Girona (Spain) in 2000 and 2009. The baseline survey carried out in 2000 examined a randomly selected, population-based sample of 3058 men and women aged 25–74 years (participation rate: 71·0 %). A two-stage sampling method was used in 2000: seventeen towns were randomly selected in the first stage. Half of the towns were urban (>10 000 inhabitants) and half were rural (500–10 000 inhabitants). The second sampling stage consisted of randomly recruiting the same number of female and male participants, stratifying by 10-year age groups from the closest census.
In 2009, the 2715 non-institutionalised participants still residing in the catchment area were invited for re-examination, and 2181 attended (follow-up participation rate: 80·3 %). Participants following a special diet at re-examination (n 207 (9·8 %)) were excluded. The participants were duly informed, and they signed their consent to participate in the study. The project was approved by the local Ethics Committee (CEIC-PSMAR, Barcelona, Spain).
Anthropometrics
A calibrated precision scale was used for measuring weight. Readings were rounded up to 200 g. Height was measured in the standing position and rounded up to the nearest 0·5 cm. Weight was divided by height squared (kg/mReference Fox, Despres and Richard 2 ) to establish the BMI.
WC was measured midway between the lowest rib and the iliac crest in the horizontal position. Readings were rounded up to the nearest 0·5 cm. Abdominal obesity was defined by sex-specific cut-offs of more than 102 cm for men and more than 88 cm for women( Reference Lean, Han and Morrison 13 ).
All the anthropometric parameters were measured both at baseline and at follow-up, using the same protocol.
Dietary intake assessment
Dietary intake was determined using a validated( Reference Benitez-Arciniega, Mendez and Baena-Diez 14 , Reference Schroder, Covas and Marrugat 15 ) FFQ, administered by a trained interviewer at baseline and at follow-up. In a 166-item food list including alcoholic and non-alcoholic beverages, the participants indicated their usual consumption frequency and chose from ten frequency categories ranging from never or less than once per month to six or more times per d.
Adherence to the Mediterranean diet was determined by the validated REGICOR-Mediterranean diet score (R-MDS)( Reference Benitez-Arciniega, Mendez and Baena-Diez 14 ). The published Pearson correlation for the energy-adjusted R-MDS v. multiple recalls was 0·48( Reference Lean, Han and Morrison 13 ). The R-MDS was calculated using two strategies: sex-specific tertile distribution of food intake( Reference Benitez-Arciniega, Mendez and Baena-Diez 14 ) (R-MDS) and dietary recommendations established in Spain( 16 , 17 ) (MDS-rec). The lowest tertile was coded as 1, medium as 2 and the highest as 3 for cereals, fruits, vegetables, legumes, fish, olive oil and nuts. For meat (including red meat, poultry and sausages) and dairy products, the score was inverted, with the highest tertile being coded as 1 and the lowest as 3. Moderate red wine consumption (up to 20 g/d) was coded as 3, and that more or less than this daily portion was coded as 1. Using the second strategy, consumption that met the recommendations for cereals, fruits, vegetables, legumes, fish, olive oil, nuts and dairy products was coded as 3, that at least weekly as 2 and that less than weekly levels as 1 for legumes, fish and nuts; consumption at least daily was coded as 2 and that less than daily levels as 1 for cereals, fruits, vegetables, olive oil and dairy products (see Supplementary Appendix 2, available online). For meat (including red meat, poultry and sausages) and dairy products, the score was partially inverted, with consumption more than weekly levels being coded as 1, that weekly as 2 and that meeting the recommended levels as 3. Red wine consumption was coded as described previously.
Energy misreporting
Implausible energy reporters were identified by the revised Goldberg method described previously( Reference Mendez, Popkin and Buckland 18 ). BMR was calculated using the Mifflin equation( Reference Mifflin, St Jeor and Hill 19 ):
The index of variability (S) in the components of energy balance was determined. Subjects with BMR falling above or below the upper and lower 95 % CI limits of 1·96 standard deviations for plausible energy intake were characterised as implausible energy reporters.
The following formula was used:
where
where d is the number of recording days; CV2 wEI and CV2 wBMR represent the intra-individual variations in the repeated measures of energy intake and BMR, respectively; and CV2 tP represents the inter-individual variation in physical activity levels (PAL)( Reference Black 20 ).
Other variables
The validated Minnesota leisure-time physical activity (LTPA) questionnaire was administered by a trained interviewer( Reference Elosua, Marrugat and Molina 21 , Reference Elosua, Garcia and Aguilar 22 ). LTPA is expressed as metabolic equivalents × min/d. The measurements of smoking habits and demographic and socio-economic variables were obtained from structured standard questionnaires administered by trained personnel. The participants were dichotomously categorised into non-smokers (never smokers and ex-smokers with more than 1 year of smoking cessation) and current smokers. Maximum educational level attained was determined and dichotomously recorded for analysis as primary school v. secondary school or university.
All dietary and energy intake and expenditure measurements were performed both at baseline and at follow-up, using the same protocol.
Statistical analysis
General linear modelling procedures were used to compare the baseline characteristics of the participants by tertiles of the R-MDS and by categories of the MDS-rec. ANOVA test and polynomial contrasts were used to determine overall P and P for linear trend, respectively, for normally distributed continuous variables. The Kruskal–Wallis test was used to determine overall P for non-normal distribution. Overall P and P for linear trend for categorical variables were obtained using the Pearson χ2 and Mantel–Haenszel linear-by-linear association χ2 tests, respectively.
Linear regression models were fitted to analyse the association between changes in WC and adherence to the Mediterranean diet at baseline. Changes in WC (in cm; continuous variable) were included as the dependent variable and scores as explanatory variables. For analyses, three models were fitted. The first model included sex (men/women; dichotomous), age (years; continuous) and baseline WC. The second model included smoking (yes/no; dichotomous), energy intake (kcal; continuous), alcohol consumption (g, continuous), educational level (more than primary school yes/no; dichotomous), LTPA (metabolic equivalents × min/d; continuous), and energy under- and over-reporting (both yes/no; dichotomous). The third model included changes in BMI (BMI at follow-up − BMI at baseline; continuous) to determine whether changes in WC are independent of changes in BMI. This model was adjusted by sex (men/women; dichotomous), age (years; continuous), smoking (yes/no; dichotomous), energy intake (kcal; continuous), alcohol consumption (g; continuous), educational level (more than primary school yes/no; dichotomous), LTPA (metabolic equivalents × min/d; continuous), and energy under- and over-reporting (both yes/no; dichotomous). Participants with baseline abdominal obesity were excluded from analysis in multiple logistic regression models assessing the association between R-MDS and MDS-rec adherence at baseline and 10-year incidence of abdominal obesity. Baseline R-MDS and MDS-rec values are represented by tertiles and categories, respectively.
To explore effect modification according to sex, R-MDS and MDS-rec, we modelled interaction terms for sex/R-MDS and sex/MDS-rec. Differences were considered significant if P< 0·05. Statistical analysis was carried out using SPSS version 18.0. (SPSS, Inc.).
Results
The prevalence of abdominal obesity at baseline was 29·3 % (men: 23·8 %; women: 34·4 %) and at follow-up was 40·8 % (men: 30·5 %; women: 50·5 %). Of the 1329 participants without abdominal obesity at baseline, 291 (21·9 %) had abdominal obesity at follow-up (men: 14·9 %; women: 29·6 %).
Participants with high adherence to the Mediterranean diet were less prone to smoke and had a lower prevalence of abdominal obesity than those with low dietary adherence (Tables 1 and 2). Age, LTPA, alcohol consumption and energy intake increased across the R-MDS tertiles and MDS-rec categories. The proportion of energy under-reporters decreased with greater adherence to the Mediterranean diet; with lesser adherence, energy over-reporting increased.
Table 1 General characteristics of the sample at baseline according to tertiles of the REGICOR-Mediterranean diet score (R-MDS)*
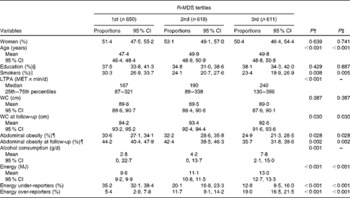
LTPA, leisure-time physical activity; MET, metabolic equivalents; WC, waist circumference.
* Age, WC, WC at follow-up, alcohol consumption and energy are continuous variables; women, education, smokers, abdominal obesity, abdominal obesity at follow-up, energy under-reporters and energy over-reporters are categorical variables.
† P values were obtained using the ANOVA, Kruskal–Wallis and Pearson χ2 tests for normal continuous, non-normal continuous and categorical variables, respectively.
‡ P values for linear trend were obtained using polynomial contrast for normal continuous variables and using the Mantel–Haenszel linear-by-linear association χ2 test for categorical variables.
§ More than secondary school education.
∥ Active smokers or ex-smokers for less than 1 year.
¶ WC >102 cm in men and >88 cm in women.
Table 2 General characteristics of the sample at baseline according to categories of the Mediterranean diet score based on dietary recommendations (MDS-rec)*
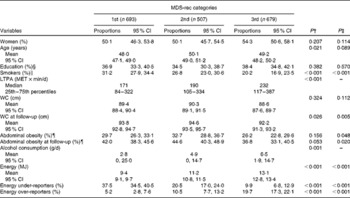
LTPA, leisure-time physical activity; MET, metabolic equivalents; WC, waist circumference.
* Age, WC, WC at follow-up, alcohol consumption and energy are continuous variables; women, education, smokers, abdominal obesity, abdominal obesity at follow-up, energy under-reporters and energy over-reporters are categorical variables.
† P values were obtained using the ANOVA, Kruskal–Wallis and Pearson χ2 tests for normal continuous, non-normal continuous and categorical variables, respectively.
‡ P values for linear trend were obtained using polynomial contrast for normal continuous variables and using the Mantel–Haenszel linear-by-linear association χ2 test for categorical variables.
§ More than secondary school education.
∥ Active smokers or ex-smokers for less than 1 year.
¶ WC >102 cm in men and >88 cm in women.
Linear regression analysis revealed a significant negative association of WC gain with the R-MDS and MDS-rec (P= 0·007 and 0·024, respectively) in the fully adjusted models (Table 3). A 10-point increase in the R-MDS and MDS-rec was associated with a decrease of 1·7 and 1·5 cm in WC, respectively. The association of changes in WC with adherence to the Mediterranean diet was independent of BMI changes.
Table 3 Multiple linear regression analysis of the association between 10-point increase in the REGICOR-Mediterranean diet score (R-MDS) and the Mediterranean diet score based on dietary recommendations (MDS-rec) and 10-year changes in waist circumference (WC) (in cm) (β-Coefficients and 95 % confidence intervals)
* Model 1 includes sex (men/women; dichotomous), age (years; continuous) and baseline WC (cm; continuous).
† Model 2 additionally includes smoking (yes/no; dichotomous), energy intake (kcal; continuous), alcohol consumption (g; continuous), educational level (more than primary school yes/no; dichotomous), leisure-time physical activity (metabolic equivalents × min/d; continuous), and energy under- and over-reporting (both yes/no; dichotomous).
‡ Model 3 includes variables of model 2 and changes in BMI (BMI at follow-up − BMI at baseline; continuous).
In the multivariate logistic analysis, high adherence to the Mediterranean diet (top tertile) was associated with a reduced 10-year incidence of abdominal obesity, but this association did not reach significance (Table 4). The magnitude of risk reduction was similar for both scores.
Table 4 OR of 10-year incidence of abdominal obesity according to tertile distribution of the REGICOR-Mediterranean diet score (R-MDS) and categories of the Mediterranean diet score based on dietary recommendations (MDS-rec)* (Odds ratios and 95 % confidence intervals)
Ref., reference.
* Total number of participants = 1329; distribution of the participants according to tertiles of the R-MDS: 1st tertile = 451; 2nd tertile = 419; 3rd tertile = 459; distribution of the participants according to categories of the MDS-rec: 1st category = 487; 2nd category = 341; 3rd category = 501.
† Model 1 includes sex (men/women; dichotomous), age (years; continuous) and baseline waist circumference (cm; continuous).
‡ Model 2 additionally includes smoking (yes/no; dichotomous), energy intake (kcal; continuous), alcohol consumption (g; continuous), educational level (more than primary school yes/no; dichotomous), leisure-time physical activity (metabolic equivalents × min/d; continuous), and energy under- and over-reporting (both yes/no; dichotomous).
Discussion
In the present prospective study, it was found that high adherence to the Mediterranean diet was associated with a lower gain in abdominal adiposity but not with the incidence of abdominal obesity within 10 years. In recent decades, increased WC has been reported for several populations( Reference Ford, Mokdad and Giles 3 ). In the present study, general obesity was about 7 % less prevalent than abdominal obesity at baseline. Most importantly, 10-year incidence of abdominal obesity was 14·8 % higher than that of general obesity. This is a cause of concern due to the direct association between WC and cardiometabolic risk( Reference Fox, Despres and Richard 2 ).
A recently published meta-analysis( Reference Kastorini, Milionis and Esposito 23 ) of the impact of adherence to the Mediterranean diet on the metabolic syndrome and its components has revealed a positive effect on WC changes in eleven randomised controlled trials. It is worth noting that this was mainly due to one trial that demonstrated a mean WC difference of − 4·20 cm ( − 7·99 to − 0·41) between the Mediterranean and control diets( Reference McManus, Antinoro and Sacks 24 ).
Among the prospective observational studies, only three surveys( Reference Kesse-Guyot, Ahluwalia and Lassale 11 , Reference Rumawas, Meigs and Dwyer 25 , Reference Tortosa, Bes-Rastrollo and Sanchez-Villegas 26 ) evaluated the association between the Mediterranean diet and WC changes. In the SUN prospective cohort (Seguimiento Universidad de Navarra; University of Navarra follow-up) the difference in WC between the highest and lowest tertiles of the Mediterranean diet score in sex- and age-adjusted models was almost 0( Reference Tortosa, Bes-Rastrollo and Sanchez-Villegas 26 ). Participants in the Framingham Heart Study Offspring Cohort who closely adhered to the Mediterranean diet had a significantly lower WC than their low-adhering peers( Reference Rumawas, Meigs and Dwyer 25 ). Additionally, the SUpplementation en VItamines et Minéraux AntioXydants (SU.VI.MAX) study reported a negative association between WC gain and two of the three Mediterranean diet score indices calculated( Reference Kesse-Guyot, Ahluwalia and Lassale 11 ).
Our data confirm the findings of previous studies showing a protective association of the Mediterranean diet with abdominal adiposity gain. In the present study, a 10-point increase in dietary scores was associated with a 1·7 cm decrease in WC.
Cross-sectional studies( Reference Kastorini, Milionis and Esposito 23 , Reference Martinez-Gonzalez, Garcia-Arellano and Toledo 27 ) have reported mixed results, which might be due to differences in the surrogate markers of abdominal obesity used (WC, waist:hip ratio and waist:height ratio). In the present study, cross-sectional analysis revealed that the risk of abdominal obesity decreased with high adherence to the Mediterranean diet.
Some( Reference Romaguera, Norat and Vergnaud 6 , Reference Mendez, Popkin and Jakszyn 28 , Reference May, Romaguera and Travier 29 ) but not all( Reference Beunza, Toledo and Hu 30 , Reference Yannakoulia, Panagiotakos and Pitsavos 31 ) prospective studies provide evidence for the protective effects of the Mediterranean diet on the incidence of general obesity. To our knowledge, no previous study has addressed the association between the Mediterranean diet and incidence of abdominal obesity. We defined abdominal obesity by WC, a surrogate marker of abdominal adiposity. We observed an inverse, but non-significant, association between adherence to the Mediterranean diet and incidence of abdominal obesity. One explanation for these results is the moderate magnitude of the association of WC change with the R-MDS. On the other hand, a substantial increase in the prevalence of abdominal obesity at follow-up and low mean change in the R-MDS ( − 0·5 points) during 10 years cancelled the effect of the Mediterranean diet on the incidence of abdominal obesity. This outcome is of interest at the public health level because it is also important to know which diets do not promote abdominal obesity.
Higher adherence to the Mediterranean diet was associated with high consumption of MUFA and PUFA, high dietary fibre intake and low energy density (data not shown). High consumption of fibre might partially explain the impact of the Mediterranean diet on abdominal adiposity through various protective mechanisms, with the increase of satiety and decrease of energy consumption( Reference Galisteo, Duarte and Zarzuelo 32 , Reference Schroder 33 ), modification of hepatic cholesterol metabolism( Reference Beunza, Toledo and Hu 30 ), and increased production of SCFA being among them( Reference Hu, Chen and Xu 34 ). Du et al. ( Reference Du, van der and Ginder 35 ) found that a 1 kcal/g (4 kJ/g) increase in energy density was associated with a 0·09 cm gain in WC per year. It has been hypothesised that energy density could be a mediator between depressive symptoms and abdominal adiposity gain( Reference Grossniklaus, Dunbar and Gary 36 ). However, the mechanisms linking WC changes and energy density are not understood. Fatty acids can activate the PPARγ gene( Reference Xu, Lambert and Montana 37 ), which is involved in lipid metabolism and particularly in the process of adipocyte differentiation. It has been demonstrated that the WC gain caused by the 12Ala allele carriers of the PPARγ gene was depressed by adherence to the Mediterranean diet( Reference Razquin, Alfredo and Martinez-Gonzalez 38 ).
Assessing the adherence to the Mediterranean diet by a score based on population-based food consumption distribution is specific to a particular population, making it difficult to compare results between studies. This construct has mainly been used by studies reporting on the association between adherence to the Mediterranean diet and incidence of obesity and/or changes in anthropometric markers of adiposity( Reference Kesse-Guyot, Ahluwalia and Lassale 11 , Reference Martinez-Gonzalez, Garcia-Arellano and Toledo 27 ). To overcome the limitation on comparability of results, we calculated two scores, one based on food distribution and the other based on food intake recommendations. We observed no meaningful impact of the type of construct used on the association between the score obtained and WC or incidence of abdominal obesity.
The strengths of the present study are the population-based design, the high participation rate during follow-up, and the measurement of anthropometric variables at baseline and at 10-year follow-up. Furthermore, dietary intake and LTPA data were recorded using validated questionnaires and all the analyses were controlled for misreporting. A benefit of using the MDS-rec is that it allows generalisability to other populations. However, all the dietary instruments measuring past food intake are vulnerable to random and systematic measurement errors.
In conclusion, adherence to the Mediterranean diet was negatively associated with changes in abdominal adiposity measured by WC. Participants with high adherence to the Mediterranean diet were less likely to develop abdominal obesity according to R-MDS tertile distribution and MDS-rec categories. However, the association was not significant. The type of R-MDS calculation (population distribution v. dietary recommendations) did not have a strong impact on these associations. Evidence of the present study underlines the usefulness of the Mediterranean diet for the prevention of abdominal weight gain.
Supplementary material
To view supplementary material for this article, please visit http://dx.doi.org/10.1017/S0007114513003966
Acknowledgements
The authors thank Elaine Lilly, PhD (Writers First Aid), for revising the manuscript for English language.
The present study was supported by a grant (2FD097-0297-CO2-01) from Fondo Europeo de Desarrollo Regional (FEDER); by portions of grants from Spain's Ministerio de Sanidad y Consumo, Instituto de Salud Carlos III FEDER (PI11/01900), Red HERACLES (RD06/0009), by scholarship for PhD formation from the National Program of University Professors Formation (FPU), from the Ministry of Education of Spain (AP2010-3198), and by a joint Miguel Servet contract (CP03/00115) from the Instituto de Salud Carlos III and the Health Department of the Catalan Government (Generalitat de Catalunya). The CIBERESP is an initiative of the Instituto de Salud Carlos III, Madrid, Spain.
The authors' contributions are as follows: A. N. F. and A. A. B.-A. prepared the manuscript, with significant input and feedback from all the co-authors; S. F. G., M. F. and R. E. participated in the design and execution of the study and contributed to the critical revision of the manuscript for important intellectual content; H. S. conducted the analyses, with results being interpreted by all the co-authors. All the authors approved the final version of the manuscript.
None of the authors has any conflicts of interest to declare.






