The links between Fe deficiency anaemia (IDA) and socio-economic status are well established within developed countries( Reference Bodnar, Scanlon and Freedman 1 – Reference Kim, Shin and Han 4 ), with it being noted that women and children from disadvantaged groups – those with low incomes, the poorly educated and migrants – are at particular risk. However, there is a more limited body of research demonstrating this link in Australia. Although it is generally accepted that the same disadvantaged groups are at a greater risk, there is very limited information on the prevalence of IDA in Australia and the groups who may be at risk( 5 ). Of the limited research that has been conducted, it is generally accepted that indigenous people within Australia, who are also known to have disproportionately high rates of low income and poor education, are more likely to experience IDA( Reference Khambalia, Aimone and Zlotkin 6 ). There is also some evidence to suggest that migrants, those living in low-income areas and the homeless are also at a higher risk( 7 ).
Despite the general recognition of the inequalities surrounding anaemia, little is known about who actually receives Fe supplements, and whether the groups who are most at risk of IDA are actually more likely to use supplements. There is limited evidence from the USA that shows that low-income women and migrant women were less likely to use Fe supplements( Reference Cogswell, Kettel-Khan and Ramakrishnan 8 ); however, no research has been reported on this relationship in Australia.
The Australian Health Survey undertaken in 2012 offers a unique opportunity to address this lack of research. This survey, conducted by the Australian Bureau of Statistics (ABS), has collected nationally representative data on Hb and ferritin levels collected from patient biomedical tests, and Fe supplementation use through the National Nutrition and Physical Activity Survey (NNPAS) and National Health Measures Survey (NHMS) components of the survey. This study aims to (1) use the Australian Health Survey to identify the groups who are most at risk of IDA and (2) determine whether these groups are more likely to use Fe supplements.
Methods
The Australian Health Survey has been flagged as the most comprehensive survey to date of the health of the Australian population, and it includes three components: the National Health Survey, the NNPAS and the NHMS. This study will focus on the NNPAS and NHMS( 9 ).
The NNPAS consists of 9519 households from all areas of Australia, excluding households in very remote Australia. The survey also excluded those living in non-private dwellings, such as motels, boarding schools, hospitals and nursing homes. Within each state of Australia, each person had an equal chance of selection, except those aged 65 years and over, who had a double chance of selection in order to improve estimates for this age group. The response rate for the NNPAS was 77 %. Within each household, information was collected from one adult and one child aged 2–17 years, giving a total sample of 12 153 persons. The NNPAS was conducted between May 2011 and June 2012. All participants in the NNPAS aged 5 years and over were then invited to voluntarily participate in the NHMS. Blood and urine samples were collected from participants aged over 11 years, and urine samples only were collected from those aged 5–11 years. The response rate for the NHMS was 37 %( 9 ).
To adjust the results obtained from the survey sample to be representative of the entire Australian population, the ABS assigned weights to each person and each household. The weight is a numerical value indicating the number of people in the population that each unit (person or household) represents. Weights were based upon the probability of selection, they were adjusted for non-response and they were calibrated against known population benchmarks from the 2006 Census of Population and Housing( 9 ).
Biomedical measure of anaemia
The NHMS collected Fe biomarkers from blood collections of those aged 12 years and over. These biomarkers consisted of serum ferritin, inflammation marker (C-reactive protein), soluble transferrin receptor and Hb. People with inflammation (C-reactive protein>10 mg/l) were excluded by the ABS from the ferritin results, as inflammation can affect ferritin levels. On the basis of Hb results, the ABS classified individuals as being at risk of anaemia based upon the following reference values for normal and abnormal Hb levels published by the WHO:
Non-pregnant females: <120 g/l
Pregnant females: <110 g/l
Males aged 12–14 years: <120 g/l
Males aged 15 years and over: <130 g/l( 9 ).
On the basis of World Health Organization( 10 ) recommendations, the authors then identified those with IDA as those at risk of anaemia based upon the above Hb levels, and having serum ferritin levels <15 µg/l.
Iron supplement use
Respondents were asked about their supplement use in the past 24 h, and they were able to select the exact supplement they used based upon a list of 10 000 dietary supplements registered for use in Australia by the Therapeutic Goods Administration. Respondents were encouraged to enter the AUST-L numbers on their supplement containers to ensure accurate matching( 9 ). On the basis of the supplements entered, the ABS recorded the nutrient content of the supplements in mg. The authors then classified anyone who consumed 18 mg or more of Fe/d as a part of their supplement consumption to be taking Fe supplements. This is based upon the National Institutes of Health’s classification of the nutrient content of a typical multivitamin with Fe supplement( 11 ).
Socio-economic variables
The Australia Health Survey, Nutrition and Physical Activity Release contains a number of socio-economic variables. The socio-economic variables included in this study were as follows:
-
1. Country of birth: Australia or overseas
-
2. Main language spoken at home: English or language other than English
-
3. Labour force status: employed (full time or part time), unemployed or not in the labour force
-
4. Level of non-school qualification: Bachelor’s degree or above, Advanced Diploma or Diploma or Certificate, or no non-school qualification
-
5. Equivalised household income quintile.
Statistical analysis
Initial descriptive analysis was undertaken to determine which of the socio-economic groups had the highest proportion of people with anaemia. Univariate analysis was initially undertaken to determine the relationship between having anaemia and age, sex, country of birth, main language spoken at home, level of non-school qualification and income. A logistic regression model was constructed of anaemia, with country of birth, main language spoken at home, labour force status, level of non-school qualification and income included as explanatory variables. The model was also adjusted for age and sex.
The analysis was then repeated to look at Fe supplement use by socio-economic group. The entire analysis was undertaken on weighted data, unless otherwise stated, and significance was set at the 0·05 level.
Results
There were 123 records on the NNPAS and NHMS who had IDA. On the basis of weighted results from the NNPAS and NHMS, there were 318 200 people whose Hb levels put them at risk of anaemia (3 % of the population) in 2012. Of these people, 71 % had serum ferritin levels that indicated that they had IDA (225 600 people). Of the people with IDA, 30 % were classified as being overweight based upon their BMI (39 % in non-IDA population) and 15 % were classified as being obese (37 % in non-IDA population).
Table 1 shows the correlation matrix between the variables included in the modelling: sex, country of birth, main language spoken at home, employment status, level of education attainment, income quintile and age. Table 2 shows that those whose main language spoken at home was English, were not in the labour force, were female and in the lowest income quintiles all had the highest proportion of people with IDA.
Table 1 Correlation matrix for variables used in modelling

OS, overseas.
Table 2 Model of iron deficiency anaemia (IDA) by socio-economic status (Odds ratios and 95 % confidence intervals)
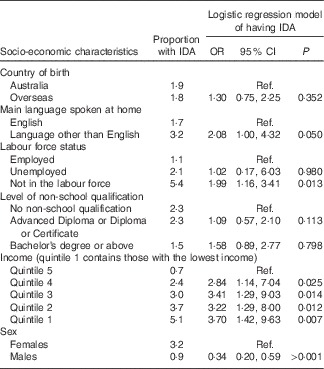
Ref., referent values.
The results of the univariate analysis show that males were significantly less likely to have anaemia than females (OR 0·046; 95 % CI 0·013, 0·158; P<0·0001), and those in income quintile 1 (OR 5·212; 95 % CI 1·332, 20·425; P=0·0177), income quintile 3 (OR 9·315; 95 % CI 2·446, 35·472; P=0·0011) and income quintile 4 (OR 4·191; 95 % CI 1·043, 16·845; P=0·0435) were all significantly more likely to have anaemia than those in income quintile 5.
The univariate analysis showed no difference in the likelihood of having anaemia between those born overseas and those born in Australia (P=0·7913); those whose main language spoken at home was English (P=0·1017) and those whose main language spoken at home was not English; between those who were unemployed (P=0·2029) and not in the labour force (P=0·2465), compared with those who were employed; and between those with a Bachelor’s degree or above (P=0·9210), those with an Advanced Diploma or Diploma or Certificate (P=0·7103) and those with no non-school qualification.
Table 2 also shows the results of the logistic regression model of IDA, with country of birth, main language spoken at home, labour force status, education level, income, sex and age all included as explanatory variables. Males had 0·34 times the odds of having IDA compared with females (95 % CI 0·20, 0·59), after adjusting for country of birth, main language spoken at home, labour force status, education level, income and age. After adjusting for other factors, those whose main language spoken at home was not English had twice the odds of having IDA compared with those whose main language spoken at home was English (95 % CI 1·00, 4·32). Similarly, those who were not in the labour force also had twice the odds of having IDA as those who were employed (95 % CI 1·16, 3·41), after controlling for country of birth, main language spoken at home, education level, income, sex and age. After adjusting for other factors, there was an increasing chance of having IDA with declining household income, with those in income quintile 1 having 3·7 times the odds of having IDA compared with those in income quintile 5 (95 % CI 1·42, 9·63).
Iron supplement use
There were an estimated 143 000 people in 2011–2012 who took Fe supplements, representing 0·5 % of the Australian population. Those who were born in Australia, those whose main language spoken at home was English, those who were not in the labour force, those who were in the highest income quintile, those who were employed and those who had a Bachelor’s degree had the highest rate of Fe supplement use (Table 3).
Table 3 Model of use of iron supplements by socio-economic status (Odds ratios and 95 % confidence intervals)

Ref., referent values.
After adjusting for country of birth, labour force status, education level, income, sex and age, those whose main language spoken at home was not English were significantly less likely to take Fe supplements (P=0·002) than those whose main language spoken at home was English. There was no significant difference in the likelihood of taking Fe supplements between those who were not in the labour force and those who were employed (P=0·618), after adjusting for other factors. There was also no significant difference in the likelihood of taking Fe supplements between those who were in income quintile 1 and in higher income quintiles, after adjusting for other factors. Similarly, there was no significant difference in the likelihood of taking Fe supplements between males and females (P=0·854), after adjusting for other factors.
Discussion
Using the biomedical results from the NNPAS and NHMS, we have demonstrated that the socio-economic differences in IDA reported internationally( Reference Bodnar, Scanlon and Freedman 1 – Reference Kim, Shin and Han 4 ) are also seen within the Australian population. People who mainly speak a language other than English at home and are in lower income quintiles were all more likely to experience IDA. The difference in the likelihood of IDA between groups with different levels of highest education attainment reported in the univariate analysis was accounted for in the full regression model by the other explanatory variables, most likely income level.
The impacts of anaemia are well documented for children and pregnant women: IDA in pregnancy is associated with numerous adverse outcomes, including low birth weight( Reference Scholl 12 , Reference Elhassan, Abbaker and Haggaz 13 ), preterm birth( Reference Scholl 12 , Reference Zhou, Yang and Hua 14 , Reference Scanlon, Yip and Schieve 15 ), fetal growth retardation( Reference Kozuki, Lee and Katz 16 ), neonatal mortality and stillbirth( Reference Zeng, Dibley and Cheng 17 , Reference Rohilla, Raveendran and Dhaliwal 18 ), as well as reduced Fe status in mother and infant( Reference Allen 19 ), which, in turn, is linked with impaired mother–infant interactions( Reference Perez, Hendricks and Beard 20 ), delayed psychomotor development, lower intelligence quotient (IQ) and poor school performance( Reference Lozoff, Jimenez and Wolf 21 – Reference Chang, Zeng and Brouwer 23 ). Despite prompt correction of IDA in infancy, significant cognitive disadvantage persists >10 years later( Reference Lozoff, Jimenez and Hagen 24 ). This parallels the irreversible effects of Fe deficiency on myelination and glial and neurotransmitter function in rodents at critical periods of early development( Reference Beard 25 ). The impacts of IDA in adulthood are less studied; however, anaemia has been linked to poor workforce performance( Reference Edgerton, Gardner and Ohira 26 ), and Fe supplementation has been shown to improve attention, concentration and IQ( Reference Falkingham, Abdelhamid and Curtis 27 ).
Given the consistent findings regarding the unequal distribution of IDA between different socio-economic groups and the known severity of the impacts of IDA, it was expected that the groups most at risk of IDA would also be more likely to use Fe supplements. However, the results have shown that there was no significant difference in the likelihood of using Fe supplements between males and females, and those in the lowest income quintile and those in higher income quintiles. Furthermore, those whose main language spoken at home was not English were actually less likely to take Fe supplements than those whose main language spoken at home was English.
This mismatch between those who are at a high risk of IDA and the use of Fe supplements shows that there is a serious need for targeted education programmes to raise the awareness of the impacts of IDA and the treatments that are available. Internationally, education and supplement programmes targeted at low-income mothers have been shown to be effective at reducing future cases of IDA among their children( Reference Rivera, Sotres-Alvarez and Habicht 28 ), and a similar programme may be suitable for adaption within Australia to target children and adults from disadvantaged groups. The results also show that there may be shortcomings within the healthcare system that ensures that those at highest risk of IDA are aware of the implications of IDA and the treatment options available. It is known, for example, that migrant women who are not proficient in English are less likely to utilise health services( Reference Kelaher, Williams and Manderson 29 ), and thus they may be less likely to be aware of IDA.
Previous studies have shown that IDA is more prevalent among individuals who are classified as being obese and, following from this, it has also been noted that obesity may be associated with an impaired ability to absorb Fe( Reference Aigner, Feldman and Datz 30 ). Thus, Fe supplementation may not be a simple solution to IDA among obese patients. Although only a small proportion of individuals with IDA in this study were also measured as being obese based upon their BMI (15 %), this is an issue that warrants consideration when tailoring the most suitable course of treatment for Fe deficiency. A number of studies have reported that normal dietary Fe absorption fwas re-established when obese subjects experienced weight loss in a healthy, sustainable manner( Reference Amato, Santoro and Calabro 31 – Reference Gong, Yuan and Teng 33 ). Thus, Fe supplementation in obese subjects coupled with a healthy weight-loss programme may be a more suitable treatment option.
Conclusion
The biomedical results contained within the NNPAS conducted by the ABS has allowed nationally representative estimates of the groups who are most at risk of IDA to be produced. However, this study has shown that these groups are not most likely to use Fe supplements. As such, it appears that there is a mismatch between those who are most in need of Fe supplements and those who currently receive them.
Acknowledgements
None.
Funding for the work came from a National Health and Medical Research Council (NHMRC) project grant (APP 1070370). Part of the funding for E. J. C.’s salary comes from an NHMRC Early Career Fellowship. All authors are independent from the funder, and the funder played no part in the study.
E. J. C. designed the study, undertook the data analysis and drafted the manuscript. D. J. S. provided input to the study design, assisted with the interpretation of the results and edited the manuscript.
The authors declare that they have no conflicts of interest.





