Gastric cancer is the fifth most common cancer and the third leading cause of cancer-related death worldwide. The incidence is significantly elevated in Eastern Asia, compared with North America and Europe(Reference Bray, Ferlay and Soerjomataram1). Increasing evidence has shown that gastric cancer was induced by synergistic effects of Helicobacter pylori infection, dietary factors and genetic instability(Reference Yamaguchi and Kakizoe2–Reference Banday, Alam and Mir4). Since H. pylori eradication has been applied, the morbidity of gastric cancer has decreased(Reference Lee, Chiang and Chou5). However, the eradication of H. pylori is becoming more difficult(Reference Megraud, Coenen and Versporten6,Reference Savoldi, Carrara and Graham7) .
Different sorts of food patterns and foods have various effects on gastrointestinal tumours(Reference Nair, Chouhan and Sen Gupta8,Reference Muscaritoli, Amabile and Molfino9) . Previous studies on diet and gastric cancer mainly used a posteriori methods to study the association between gastric cancer risk and dietary patterns(Reference Bertuccio, Rosato and Andreano10). Diets were generally categorised into healthy/prudent patterns (rich in fruit and vegetables), Western/unhealthy patterns (rich in starchy foods, meat and fat) and alcohol-drinking patterns (high consumption of alcohol). The healthy/prudent pattern showed a protective effect on gastric cancer, while the Western and alcohol-drinking patterns were risk factors. This method summarises the dietary consumption via factor analysis, principal component analysis or cluster analysis and correlated the dietary patterns with diseases’ risk. However, the a posteriori method defined dietary patterns empirically, for example, in Bahmanyar & Ye’s study(Reference Bahmanyar and Ye11), the Western pattern mainly included processed meat, red meat, sweets, high-fat dairy, high-fat gravy, high-energy drinks, whole grains and coffee, while in Kim et al.’s study(Reference Kim, Sasaki and Sasazuki12), the Western pattern mainly included butter, mayonnaise, cheese, beef, pork, poultry, bacon, liver, soda beverages, fruit juice, vegetable juice and instant noodles, which added the heterogeneity of the study. The a priori method assesses the dietary quality by a unified scoring system. For example, the Mediterranean diet score (MDS) system includes vegetables, legumes, fruits and nuts, dairy products, cereals, meat and meats products, alcohol and olive oil.
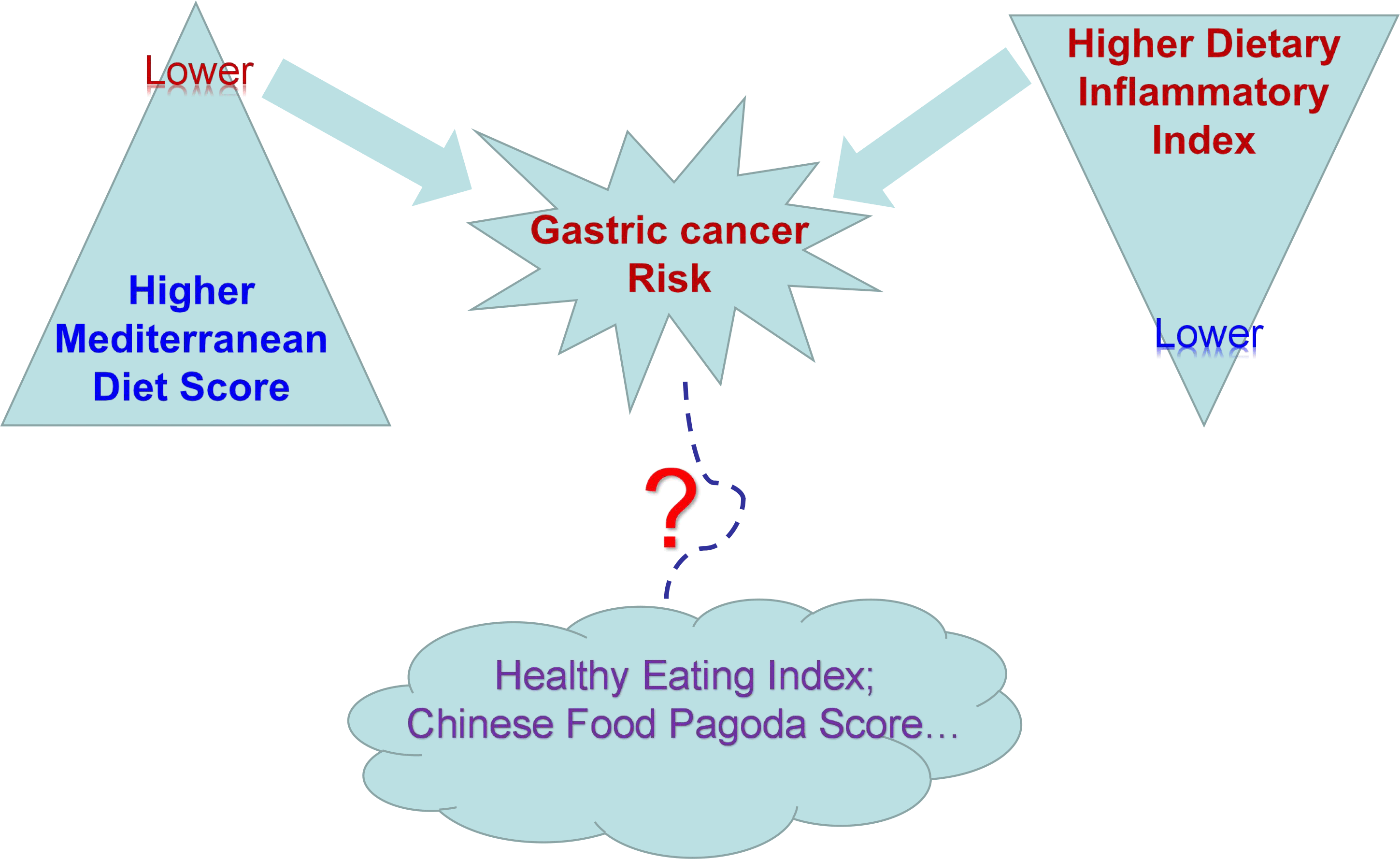
The a priori methods, namely dietary indices, were hypothesis-driven and were used to quantify dietary quality according to dietary guidelines or certain types of diets. The dietary management would be more precise and practical by using this method. So, the dietary indices could be used for chronic disease prevention and management by not only nutritionists but also clinicians and gastropathy patients. Increasing evidence has indicated the correlation between these index-based dietary patterns and the risk of gastric cancer, such as the MDS(Reference Buckland, Agudo and Luján13,Reference Buckland, Travier and Huerta14) , the healthy eating index (HEI)(Reference Li, Park and Wu15) and the dietary inflammatory index (DII)(Reference Agudo, Cayssials and Bonet16–Reference Lee, Lee and Choi18). The Mediterranean dietary pattern (MDP), which is characterised by a high intake of vegetables, fruits, legumes, non-refined cereals, nuts, olive oil, moderate intake of fish and dairy products and low intake of red meat, could prevent gastric cancer. Because these ingredients containing an abundance of antioxidants could reduce DNA damage, they could also reduce H. pylori infection(Reference Mentella, Scaldaferri and Ricci19) and inhibit the angiogenesis process of tumours(Reference Martinez-Poveda, Torres-Vargas and Ocana20). The DII, however, could reflect the inflammatory effect caused by diet(Reference Cavicchia, Steck and Hurley21), which was a key process in gastric cancer initiation and progression(Reference Montinaro and Walczak22). However, to date, there is no systematic review and meta-analysis on the association between index-based dietary patterns and gastric cancer risk. In order to quantify the general effects of high consumption of different index-based dietary patterns on gastric cancer, we carried out a systematic review and meta-analysis of observational studies on the relationship between the index-based dietary patterns and gastric cancer incidence.
Materials and methods
The protocol was registered in PROSPERO International Prospective Register of systematic reviews (ID: CRD 42018100575).
Inclusion and exclusion criteria
Studies were included if they met the following SPIDER(Reference Methley, Campbell and Chew-Graham23) (Sample, Phenomenon of Interest, Design, Evaluation, Research type) criteria: (1) Sample: for cohort studies, the general population without gastric cancer; for case–control studies, patients who were diagnosed with gastric cancer. (2) The Phenomenon of Interest: the incidence of gastric cancer. (3) Design: studies using index-based dietary patterns to reflect dietary quality. (4) Evaluation: the consumption of certain index-based dietary patterns, such as the Mediterranean diet (reflected by the MDS) and the inflammatory diet (reflected by DII). (5) Research type: prospective cohort, retrospective cohort, case–control.
Studies were excluded for: (1) cellular, animal experiments; (2) studies on the other risk or protective factors for gastric cancer; (3) studies on certain drugs, foods, nutrients or eating behaviours; (4) studies that used a posteriori methods to identify dietary patterns.
Search strategy
A comprehensive search of literature published before December 2018 was performed in PubMed (https://www.ncbi.nlm.nih.gov/pubmed), Embase (https://www.embase.com), Web of Science (https://www.webofknowledge.com), Cochrane Library (https://www.cochranelibrary.com), CNKI (https://www.cnki.net), VIP (http://www.cqvip.com), WAN FANG (http://www.wanfangdata.com.cn) and SinoMed (http://www.sinomed.ac.cn). Publications with title and abstract containing the keywords ‘diet’, ‘gastric’, ‘cancer’ were identified. The full list of the searching strategy was as follows: (diet* OR food OR eat*) AND (quality OR pattern OR score OR index OR indices) AND (gastric OR stomach) AND (cancer OR neoplasm OR tumor OR carcinoma). There were no restrictions on the types of publications or the participants’ characteristics, but only studies published in English and Chinese were considered.
Screening
Two authors screened all the identified literature by title and abstract independently and selected articles according to the inclusion and exclusion criteria. Then, a full-text screen was made on all possibly eligible papers. Relevant studies in reference lists that met the inclusion criteria were also included. Finally, all eligible articles were collected, and disagreements that could not be resolved by discussion were presented to a third person for the final decision.
Data extraction
Data extracted included general information (authors and year of publication, time of enrollment or follow-up time and the regions of the study), participants (numbers of participants), dietary assessment (data collection method and dietary indices used for assessment), adjusted variables (factors related to gastric cancer, such as H. pylori infection, age, sex, alcohol intake, smoking, physical activity, etc.), main findings (conclusion of the relation of dietary indices to gastric cancer incidence, OR, risk ratio or hazard ratio (HR) of the highest quantile interval compared with the referent or one-unit increase in the score, 95 % CI, P value), subgroup analysis (female and male, gastric cardia adenocarcinoma (GCA) and gastric non-cardia adenocarcinoma (GNCA), intestinal type and diffuse type). Data not shown in the publication were acquired by sending an email to the author.
Quality assessment
The quality and risk of bias of the included studies were assessed using a modified Newcastle–Ottawa Scale (NOS) for assessing the quality of non-randomised studies(Reference Wells, Shea and O’Connell24). Two researchers independently assessed the quality of the studies using the NOS, and the disagreement was resolved by discussion with the third person. Three aspects, namely, selection, comparability and outcomes, were assessed using this scale, with a maximum score of nine. Studies scored six or more stars were considered as having high quality.
Statistical analysis
We first categorised all the retrieved dietary indices used in gastric cancer incidence studies. Then for each type of indices, mean difference with 95 % CI was pooled into the relevant effect models.
For heterogeneity assessment, we first carried out a Q test. As the test detected moderate degrees of heterogeneity and there were not many included studies, P ≤ 0·1 was considered of significant heterogeneity. Then, the I 2 statistic was calculated. I 2 equaling 0–25 % indicates that the heterogeneity might not be important; 25–50 % represents moderate heterogeneity; 50–75 % represents substantial heterogeneity and 75–100 % represents considerable heterogeneity(Reference Higgins, Thompson and Deeks25). When heterogeneity was more than 25 %, a random effect model was used for meta-analysis. A fixed effects model was used when the heterogeneity was less than 25 %(Reference Higgins and Green26). Publication bias would be assessed by Begg’s and Egger’s tests if the included studies were ten studies or more.
All calculations and graphs were performed using Review Manager version 5.3 (Nordic Cochrane Center).
Subgroup analysis and sensitivity analysis
In order to deal with heterogeneity, subgroup analysis is necessary. These will focus on four aspects: (1) patterns of diets (MDP and inflammatory diet pattern); (2) types of study (cohort study or case–control study); (3) types of gastric cancer (GCA and GNCA, intestinal type and diffuse type) and (4) regions of study. In order to explore the influence of the methodological quality of the study on effect size, sensitivity analyses might be performed. Pre-specified sensitivity analyses will be performed by removing one study at a time and determining the influence of a single article on the overall pooled estimate.
Results
Study characteristics and quality assessment
As shown in the flow chart (Fig. 1), eleven publications were selected from 4104 pieces of the article identified by the systematic review. The main characteristics and NOS scores of each study are shown in Tables 1 and 2, respectively. According to NOS assessment, all studies were eligible, among which nine were considered as high quality. Among these, five studies focused on the association between gastric cancer and Mediterranean diet using different versions of the MDS created by Trichopoulou et al. (Reference Trichopoulou, Kouris-Blazos and Wahlqvist32). They are the relative MDS in Buckland’s studies(Reference Buckland, Agudo and Luján13,Reference Buckland, Travier and Huerta14) ; the alternate MDS(Reference Fung, McCullough and Newby33) in Li et al.’s study(Reference Li, Park and Wu15); the MDS in the first case–control study in Praud et al.’s study(Reference Praud, Bertuccio and Bosetti29); the MDS, MDP adherence index(Reference Sanchez-Villegas, Martinez and De Irala34) and Mediterranean Adequacy Index(Reference Alberti-Fidanza and Fidanza35) in the second case–control from the same article(Reference Praud, Bertuccio and Bosetti29) and Literature-based adherence score to the Mediterranean Diet(Reference Sofi, Macchi and Abbate36,Reference Sofi, Dinu and Pagliai37) in Stojanovic et al.’s study(Reference Stojanovic, Giraldi and Arzani30). Other widely applied dietary indices were different versions of DII(Reference Cavicchia, Steck and Hurley21), such as the Literature-derived Population-based DII(Reference Shivappa, Steck and Hurley38) used in the case–control study by Shivappa et al. (Reference Shivappa, Hebert and Ferraroni17), as well as another two case–control studies by Lee et al. (Reference Lee, Lee and Choi18) and Vahid et al. (Reference Vahid, Shivappa and Faghfoori31); and Inflammatory Score of the Diet in Agudo’s cohort study, which is mainly based on DII and changed according to local dietary habits(Reference Agudo, Cayssials and Bonet16). There were three other types of dietary indices, the food index score used in Campbell et al.’s study(Reference Campbell, Sloan and Kreiger28), the HEI-2005(Reference Guenther, Reedy and Krebs-Smith39) used in Li et al.’s cohort study(Reference Li, Park and Wu15) and the Chinese Food Pagoda (CHFP) score(Reference Yu, Zhang and Xiang40) used in Zhang et al.’s cohort study(Reference Zhang, Zheng and Li27).

Fig. 1. Flow chart of the literature search. MDS, Mediterranean Diet Score.
Table 1. Main characteristics of eleven studies in the systematic review*

GC, gastric adenocarcinoma; EPIC, Europe Prospective Investigation into Cancer and Nutrition Cohort; GCA, gastric cardia adenocarcinoma; GNCA, gastric non-cardia adenocarcinoma; CGC, cardia gastric cancer; NCGC, non-cardia gastric cancer; HRcon, Hazard Ratio for continuous variable; MDS, Mediterranean Diet Score; rMED, relative MDS; aMED, alternate MDS; MDPAI, Mediterranean Dietary Pattern Adherence Index; MAI, Mediterranean Adequacy Index; MEDI-LITE, Literature-based adherence score to the Mediterranean Diet; DII, Dietary Inflammatory Index; ISD, Inflammatory Score of the Diet; HEI-2005, Healthy Eating Index-2005; CHFP, Chinese Food Pagoda.
* All OR represents the OR of the highest quantile compared with the referent, and the lowest quantile was considered as the referent. All HR represents the HR of the highest quantile compared with the referent, and the lowest quantile was considered as a referent.
Table 2. Newcastle–Ottawa Scale of eleven studies in the systematic review

In the studies on indices based on MDP and gastric cancer incidence, there were different conclusions. Three case–control studies and two cohort studies indicated that high adherence to the Mediterranean diet was associated with reducing gastric cancer risk, while the other cohort study on the American population demonstrated that Mediterranean diet was associated with increased risk of GCA and decreasing risk of GNCA. In the studies related to DII, the score was associated with increased gastric cancer risk. The HEI, based on the American dietary guidelines, showed a protective effect in the cohort study. What is more, the food index score was inversely associated with gastric cancer incidence. There was only one piece of study on HEI and one piece of study on food index score, other studies focused on MDS and DII. Therefore, we carried out a meta-analysis on the studies using MDS (including MDS, relative MDS, alternate MDS, and Literature-based adherence score to the Mediterranean Diet) or DII (including Literature-derived Population-based DII and Inflammatory Score of the Diet). The analysis was carried out for case–control and cohort studies, respectively.
Meta-analysis
Since the included studies focused on different versions of dietary indices, and only the studies on MDS and DII have more than one study, we included the studies on MDS and the studies on DII in the meta-analysis. Because two pieces of Buckland et al.’s literature (2010(Reference Buckland, Agudo and Luján13) and 2015(Reference Buckland, Travier and Huerta14)) were from the same study(Reference Riboli, Hunt and Slimani41) (the one published in 2015 has a larger population), two cohort studies on MDS, two case–control studies on MDS and three case–control studies on DII were included in meta-analysis, respectively.
The estimated OR and HR for the highest quantile interval v. the lowest values of MDS and DII are shown in Figs. 2 and 3, respectively. For MDS and gastric cancer risk, there were two case–control studies and two cohort studies focusing on the association between MDP and gastric cancer risk. For the case–control studies, groups with a high MDS had a significantly lower odds of developing gastric cancer than those with a low score (OR 0·42 (95 % CI 0·20, 0·86), P = 0·02). For the cohort studies, there was a similar tendency in both GCA (HR 0·84 (95 % CI 0·47, 1·49), P = 0·54) and GNCA (HR 0·92 (95 % CI 0·63, 1·35), P = 0·67); the combined HR was 0·89 (95 % CI 0·68, 1·17), P = 0·4. However, the tendency was not significant. There was a substantial heterogeneity in both case–control (I 2 = 77 %) and cohort studies (I 2 = 52 %). As there were only two studies for each meta-analysis, the sensitivity analysis could not be carried out. The subgroup analysis did not show any reduction of heterogeneity for the cohort studies (for GCA I 2 = 73 %; for GNCA I 2 = 59 %). As two cohort studies were carried out in America (USA) and Europe (ten different countries), respectively, and two case–control studies were all in Italy, the subgroup analysis on the region of study is impossible to carry out. The heterogeneity might be caused by different versions of MDS (alternate MDS in Li et al.’s study(Reference Li, Park and Wu15), relative MDS in Buckland et al.’s study(Reference Buckland, Travier and Huerta14), MDS in Praud et al.’s study(Reference Praud, Bertuccio and Bosetti29) and Literature-based adherence score to the Mediterranean Diet in Stojanovic et al.’s study(Reference Stojanovic, Giraldi and Arzani30)). According to the NOS system, all studies included are of high quality. Stojanovic et al.’s case–control study scored lower for lack of non-response rate description.

Fig. 2. Forest plot for the Mediterranean diet patterns and gastric cancer risk studies. HR, hazard ratio; MDS, Mediterranean Diet Score; IV, inverse variance; Random, random-effect methods; GCA, gastric cardia adenocarcinoma; GNCA, gastric non-cardia adenocarcinoma.

Fig. 3. Forest plot for the inflammatory dietary patterns and gastric cancer risk studies. DII, Dietary Inflammatory Index.
For DII and gastric cancer risk, there were three case–control studies included in the meta-analysis. High DII dietary patterns showed significantly higher odds of gastric cancer risk than lower DII dietary patterns (OR 2·11 (95 % CI 1·41, 3·15), P = 0·0003. As there existed moderate heterogeneity (I 2 = 41 %), a sensitivity analysis was carried out. When Shivappa et al.’s study(Reference Shivappa, Hebert and Ferraroni17) was removed, the heterogeneity increased (I 2 = 65 %), while heterogeneity reduced when Lee et al.’s study or Vahid et al.’s study was removed (I 2 = 0 % or I 2 = 12 %). Since three studies were taken in different continents, and only Lee et al.’s study has subgroup analysis based on the intestinal type and diffuse type, the subgroup analysis was not able to be taken. According to NOS, all these studies were of high quality. Vahid et al.’s study quality was relatively lower; considering the result of sensitivity analysis, the heterogeneity might be caused by Vahid et al.’s study. The publication bias could not be assessed, as there were less than ten studies included.
Discussion
We retrieved studies on different types of index-based dietary patterns related to gastric cancer incidence. The study populations were from Asia, North America and Europe. The results indicated that the MDP has a preventing effect on gastric cancer, while inflammatory dietary pattern promoted gastric cancer. There was one study on the HEI, one study on the CHFP score and one study on the food index score.
We combined the HR or OR for different types of dietary patterns and obtained a general trend. However, the studies were separated into different types of dietary patterns; thus, each meta-analysis had a limited number of included studies. Our study showed all kinds of index-based dietary patterns in relation to gastric cancer and offered practical ways for gastric cancer prevention. However, as we mentioned, different dietary patterns were based on the geographic and cultural characteristics of the local population; thus, whether one particular dietary index could also predict gastric cancer risk in another population requires further verification. For example, the study on MDS and gastric cancer was based on American and European populations, and whether the index could be used for gastric cancer prevention in Asia needs to be verified.
The MDP was based on the dietary habits of residents in most parts of Greece and Southern Italy, where adults have a longer life expectancy and lower rates of chronic diseases. Characters of this dietary pattern are abundant vegetables and fresh fruit, low in saturated fat, with low to moderate amounts of dairy products, fish, poultry and wine(Reference Willett, Sacks and Trichopoulou42). A large variety of studies have indicated the positive roles of the Mediterranean diet in health status(Reference Sofi, Macchi and Abbate36,Reference Trichopoulou and Lagiou43) . In 1995, Trichopoulou et al. food index score first devised the scoring system, MDS, finding a significant protective effect against overall mortality (risk ratiofor 1 unit increasing = 0·83, 95 % CI 0·69, 0·99) in the Mediterranean region(Reference Trichopoulou, Kouris-Blazos and Wahlqvist32). Since then, numerous variations of this score have been proposed(Reference Buckland, Agudo and Luján13,Reference Sanchez-Villegas, Martinez and De Irala34–Reference Sofi, Dinu and Pagliai37) , which are suitable for different countries and areas.
According to the anatomical location, gastric adenocarcinoma is classified into two main types, gastric cardia (proximal) and gastric non-cardia (distal) adenocarcinoma(Reference Piazuelo and Correa44). Different types of gastric adenocarcinoma have different epidemiological characteristics and aetiology, for example, GCA is more susceptible in people with high BMI and obesity(Reference Chen, Liu and Wang45,Reference Cho, Lee and Oh46) , whereas gastric GNCA is more related to H. pylori infection(Reference Marqués-Lespier, González-Pons and Cruz-Correa47). Buckland et al.’s cohort study(Reference Buckland, Travier and Huerta14) indicated that high adherence to a Mediterranean diet was associated with a reduced risk of both GCA and GNCA in a European population, while Li et al. (Reference Li, Park and Wu15) found a protective effect of the Mediterranean diet in the American population, but only for gastric GNCA. Since Li et al.’s result was not statistically significant, further well-designed prospective studies with a larger population are needed. Different versions of the scores added to the heterogeneity. So, a more precise definition of the Mediterranean diet and a more unified standard should be developed(Reference Bach, Serra-Majem and Carrasco48,Reference Jacques and Tucker49) .
The DII was first proposed by Cavicchia through a literature search on foods and constituents related to IL-1β, IL-4, IL-6, IL-10, TNF-α and C-reactive protein(Reference Cavicchia, Steck and Hurley21). The scale was then validated by high-sensitivity C-reactive protein level from 494 healthy participants. The DII was improved by Shivappa et al., who developed a scale with forty-five parameters, including protein, total fat, carbohydrate, cholesterol and caffeine(Reference Shivappa, Steck and Hurley38), which is now widely used in different studies. DII was based on data collected from FFQ, and the data were converted into a Z score and centred percentiles for each component, according to the average and standard deviation derived from regionally representative world databases. The food parameter-specific DII was obtained by multiplying the percentiles of each component by its inflammatory effect score and eventually summed to create an overall DII for each individual. By using this approach, the problem of non-comparability of units was resolved; thus, DII could reflect the proinflammatory effects of diet worldwide.
Inflammation induces cancer in various ways, including DNA damage, avoidance of immune surveillance and synergistic effects with commensal microbiota(Reference Trinchieri50). Anti-inflammatory drugs can significantly reduce gastrointestinal cancer(Reference Rothwell, Fowkes and Belch51). However, the adverse effects of aspirin and non-steroidal anti-inflammatory drugs, such as peptic ulcer, cannot be neglected. Hence, avoiding an inflammatory diet and taking more anti-inflammatory food are a better choice.
There were also other types of dietary indices used in gastric cancer studies, which were the food score index(Reference Campbell, Sloan and Kreiger28), the HEI-2005(Reference Li, Park and Wu15) and the CHFP score(Reference Zhang, Zheng and Li27). In 2007, Campbell et al. (Reference Campbell, Sloan and Kreiger28) designed the food index score based on previous studies on dietary components and gastric cancer risk in order to avoid the data-driven problem from a posteriori approach. The result indicated that the food index score was an efficient tool for gastric cancer prevention, and this was the first study that we could find that used an a priori approach to study the association between dietary pattern and gastric cancer. However, as the food index score was not derived from dietary guidelines, it was not widely applied in further studies.
The HEI was designed by the US Department of Agriculture on the basis of local dietary guidelines and used to monitor dietary intake and quality(Reference Kennedy, Ohls and Carlson52). HEI-2005 was a revised version based on the 2005 American Dietary Guidelines, but with the same principle. There was only one study on the association between the HEI and gastric cancer incidence. Although not significant, the result showed both GCA and GNCA incidence were related to lower HEI-2005 score and further studies should be carried out to verify this conclusion.
In China, the first dietary guidelines were devised by the Chinese Nutrition Society in 1989, which consisted of eight entries(Reference Ge53). After several revisions, the newest version was published by the Chinese Nutrition Society in 2016. The Chinese Nutrition Society also published the new dietary pagoda, which showed the appropriate amount of food consumption(Reference Wang, Lay and Yu54). The CHFP scoring method is similar to the HEI(Reference Yu, Zhang and Xiang40). Zhang et al.’s cohort study showed that higher quantiles in CHFP score had lower gastric cancer risk in men, but after adjusting for age, education level, occupation, income, tea-drinking habits, smoking habits, physical exercise, BMI and alcohol consumption, the result became confused (risk ratio highest quantile v. lowest = 1·02, risk ratio middle quantile v. lowest = 0·9). Further studies should be carried out to resolve this problem.
There were several limitations to our meta-analysis. First, the studied populations were different (America, Europe and Asia). The prevalence of H. pylori infection was quite different(Reference Hooi, Lai and Ng55); however, only two studies(Reference Lee, Lee and Choi18,Reference Vahid, Shivappa and Faghfoori31) on DII considered this factor as a covariate. Second, as the dietary habits of different populations vary from each other, the dietary indices were calculated on the basis of each local food consumption database, collected by FFQ. Third, although the HR and OR were all from the highest quantile (taking the lowest as the referent), different studies divided the score range into different intervals. These caused substantial heterogeneity. Fourth, the data collection procedure was based on the self-report of participants. The participants may record what they believe the researchers want them to put rather than actually eat. Thus, inherent recall bias existed. What is more, the unexpected and non-significant association between index-based dietary indices and gastric cancer incidence may not be published and only published literature in English or Chinese was included in the present study, so there might exist publication bias.
Our meta-analysis indicated that MDS and DII were the most widely used dietary indices in gastric cancer prevention, and higher MDP consumption might reduce gastric cancer risk, while higher inflammatory diet pattern consumption might increase gastric cancer risk. Whether these indices could be applied in a worldwide population still remained to be verified in larger cohort studies. Future cohort and case–control studies should focus on the application of these dietary patterns in different populations, regions, cultures and the effects on gastric cancer prevention or progression.
Acknowledgements
The authors thank the editors and reviewers for their constructive and critical comments and suggestions, which helped them improve the manuscript.
This work was funded by a grant from the Chinese Natural Science Foundation (no. 81630080), the Chinese Natural Science Foundation (no. 91129714), the Chinese Natural Science Foundation (no. 81703931) and the Fundamental Research Funds for the Central Universities (no. 2018-JYB-XS165).
X. D. and S. D. formulated the research question. S. D. and Y. F. designed the study. S. D., Y. L., Z. S., X. S., N. J., P. L., Y. Z., Q. Z. and L. W. conducted the study and analysed the data. S. D. and X. Z. evaluated the quality of included studies. S. D., Y. L., X. D., Y. F., K. L. and Y. C. discussed the results and wrote the paper. All of the authors contributed to the revision of the manuscript and approved the final version.
None of the authors has any conflicts of interest to declare.