Falls and fractures are a major cause of morbidity and mortality, particularly in older adults. The Global Burden of Disease Study (2017) found that falls were the 18th leading cause of age-standardised rates of disability-adjusted life years and were the second leading cause of death due to unintentional injuries(Reference James, Lucchesi and Bisignano1). In those aged ≥70 years, falls were the leading cause of injury-related death. Approximately 30 % of people aged ≥65 years experience at least one fall per year, and in Australia in 2016/2017, there were over 125 000 hospitalisations for fall-related injury(Reference Pointer2). In addition to being a proximate cause of injury and death, falls lead to loneliness and social isolation(Reference Petersen, Konig and Hajek3), which are risk factors for poor quality of life and increased mortality.
Hip fracture is a common sequela of falls, particularly against a background of osteomalacia or osteoporosis. Hip fracture is the most serious of the fractures linked to osteoporosis due to the high mortality, disability and need for long-term institutional care. It has been estimated that by 2050, 6·3 million hip fractures will occur worldwide each year, and that in elderly populations from Europe and the USA, a hip fracture will result in an average loss of 2·7 % of healthy life expectancy(Reference Papadimitriou, Tsilidis and Orfanos4).
Vitamin D plays a critical role in calcium homeostasis and influences muscle mass and function(Reference Girgis, Clifton-Bligh and Hamrick5,Reference Girgis, Cha and So6) , and adequate vitamin D status is thus essential for maintaining musculoskeletal health. Vitamin D deficiency results in a lack of bone mineralisation, causing osteomalacia, which presents as rickets in children and causes bone pain and fractures in adults. Low serum 25 hydroxy vitamin D (25(OH)D – the marker used to measure vitamin D status) has also been consistently linked with increased risk of falls and hip fractures(Reference Annweiler and Beauchet7–Reference Lv, Gao and Liu9). Although the evidence that vitamin D supplementation prevents these outcomes in community-dwelling adults is not strong(Reference Bolland, Grey and Avenell10), a role for vitamin D in musculoskeletal health is accepted and informs policy regarding vitamin D testing and treatment of deficiency.
Vitamin D is produced in the skin upon exposure to ultraviolet B radiation. It is also found in some food sources, but intake from foods is insufficient to maintain adequate vitamin D status in most populations(Reference Nowson, McGrath and Ebeling11). Thus, in the absence of supplementation, sun exposure is the primary source of vitamin D. However, sun exposure also has harms, most notably skin cancers and premalignant lesions, which have a large disease burden in regions with high sun exposure and mostly light-skinned populations. Australia has the highest incidence of skin cancer in the world(Reference Fitzmaurice, Akinyemiju and Al Lami12), but the best available evidence suggests that nearly a quarter of people have inadequate vitamin D, according to Australian recommendations (25(OH)D <50 nmol/l)(13). Providing guidance on sun exposure requires contemporary evidence about the proportion and number of skin cancers attributable to excess sun exposure, alongside an understanding of the amount of ill-health that is attributable to low vitamin D status. We thus aimed to calculate the proportions of hip fractures and hospitalisations due to falls in Australia that can be attributed to low vitamin D. A similar approach applied to other populations will help to inform public health policy.
Methods
We calculated the proportion and number of hospitalisations annually for hip fractures and falls in adults ≥65 years that can be attributed to vitamin D deficiency. We used routinely available Australian data on the prevalence of vitamin D deficiency, the number of hospitalisations for hip fractures and falls, and relative risk (RR) estimates for the association between vitamin D deficiency and these outcomes from published meta-analyses.
Ethical approval was not required for this study, which uses publicly available data. The Australian Bureau of Statistics approved the release of vitamin D deficiency prevalence data.
Prevalence of vitamin D deficiency
We obtained estimates of the prevalence of 25(OH)D <50 nmol/l from the Australian National Health Measures Survey (NHMS) which formed part of the 2011/12 Australian Health Survey (AHS). Detailed methods of the AHS can be found elsewhere(14). Participation in the NHMS was voluntary, and 10 401 respondents (32 % of the total AHS sample) provided biomedical samples. The sample was weighted to represent the Australian population(15). Serum 25(OH)D was measured using liquid chromatography tandem mass spectroscopy (LC-MS/MS) by a laboratory (Douglass Hanley Moir) that was taking part in the National Institute of Health Vitamin D Standardisation Programme(Reference Wise, Tai and Burdette16).
We calculated prevalence within two age categories (65–74 years; ≥75 years) using data from the 2011–12 AHS Confidentialised Unit Record File, which contains deidentified unit record data(17).
Relative risk estimates
We obtained the estimate of the association between 25(OH)D <50 nmol/l and the risk of falling from a meta-analysis of observational cohort studies published in 2014 (RR 1·44; 95 % CI 1·17, 1·76)(Reference Annweiler and Beauchet7). In addition to the main effect estimates, we also applied the upper and lower bounds of the 95 % CI.
We used a meta-analysis published in 2019 as the source of RR estimates for hip fracture(Reference Yao, Bennett and Mafham18). The meta-analysis presented the RR per 25 nmol/l increase in 25(OH)D concentration. To calculate the RR of having 25(OH)D <50 nmol/l compared with ≥50 nmol/l, we first converted this to the RR per 1 nmol/l decrease in 25(OH)D concentration. We then calculated the difference between the mean 25(OH)D concentration among participants in the <50 and ≥50 nmol/l subgroups in the NHMS data (these were 38 and 75 nmol/l, respectively, i.e., a difference of 37 nmol/l). We multiplied the risk per 1 nmol/l decrease by this difference (i.e. by 37). This resulted in an RR estimate of 1·39 (95 % CI 1·25, 1·53).
Number of hospitalisations for falls and hip fracture in Australia
We obtained data, by age and sex, on the number of hospitalisations for falls (ICD-AM injury diagnosis S00–T75 or T79, and external cause code W00–W19) and hip fractures (ICD10-AM, Ninth Edition codes S72.0, S72.1, S72.2) reported in the Australian Institute of Health and Welfare National Hospital Morbidity Database. We used data for falls from 2011/12(Reference Pointer19) as this was the time period over which vitamin D status was assessed. The earliest hip fracture data available were from 2015/16(20). We restricted all analyses to people aged ≥65 years as this is the age group most frequently included in the studies investigating the association between vitamin D and these outcomes.
Calculation of population-attributable fraction
The population-attributable fraction (PAF) for each age–sex group was calculated using the following formula:
where page-sex is the proportion of the population in a given age–sex group that is vitamin D-deficient, and ERR is the excess RR (RR–1) associated with being deficient. We then multiplied the number of falls and hip fractures in each age and sex category by the age- and sex-specific PAFs to estimate the number of events in each group attributable to vitamin D deficiency (i.e. the total excess events). To calculate the overall PAF, we divided the total number of excess events, summed across all age and sex groups, by the total number of events.
Results
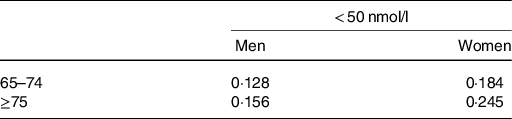
The percentage of people with 25(OH)D <50 nmol/l varied from 12·8 % in men 65–74 years to 24·5 % in women aged ≥75 years (Table 1).
Table 1. Survey-weighted estimates of prevalence of 25 hydroxy D concentration <50 nmol/L by age and sex
In men and women combined, 8·3 % of hospitalisations for falls were attributable to 25(OH)D concentration <50 nmol/l, accounting for 7991 excess events (Table 2). Applying the lower and upper bounds of the 95 % CI resulted in PAFs of 3·4 % and 13·5 %, respectively (excess events ranging from 3261 to 12 989) (see online supplementary material, Supplemental Table S1). The PAF was higher for women than for men (9·3 % v. 6·1 %); this combined with the higher number of falls in women resulted in >3 times as many falls being attributable to vitamin D deficiency in women compared with men.
Table 2. PAF and excess hospitalisations for falls attributable to 25 hydroxy D (25(OH)D) concentration <50 nmol/l
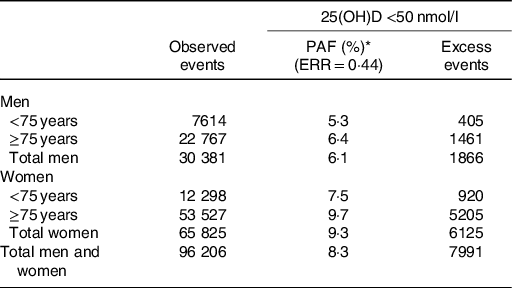
Abbreviations: PAF = population-attributable fraction; ERR = excess relative risk.
* PAF rounded for presentation and presented as percentage.
Almost 8 % of hospitalisations for hip fractures were attributable to 25(OH)D <50 nmol/l (1315 excess events) (Table 3). Applying the bounds of the 95 % CIs, the PAF ranged from 5·0 % to 10·1 % (excess events 865–1735) (see online supplementary material, Supplemental Table S2). As for falls, the PAF and number of falls attributable to vitamin D deficiency was markedly higher in women than in men.
Table 3. PAF and excess hospitalisations for hip fractures attributable to vitamin D deficiency
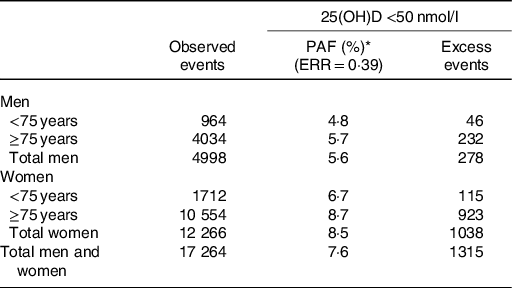
Abbreviations: 25(OH)D = 25 hydroxy D; PAF = population-attributable fraction; ERR = excess relative risk.
* PAF rounded for presentation and presented as percentage.
Discussion
Our primary estimates show that ˜8 % of hospitalisations for falls and hip fractures in older adults may be attributable to vitamin D deficiency, defined as a 25(OH)D concentration of <50 nmol/l, accounting for a total of >9000 events annually. This suggests that mitigating vitamin D deficiency may have a significant impact on these outcomes in the Australian population.
These conclusions are predicated on the assumption that the link between having low vitamin D status and falls/hip fractures is causal and has not arisen due to uncontrolled confounding or reverse causation; this notion has been contested. While the associations between vitamin D and these musculoskeletal health outcomes are well established in observational studies, a 2018 meta-analysis and trial sequential analysis of RCTs concluded that vitamin D supplementation does not reduce the risk of falls or hip fractures(Reference Bolland, Grey and Avenell10). This conclusion is supported by findings from the large Vital Trial in the USA that found supplementing adults with 50 mcg of vitamin D per day did not reduce the risk of ≥2 falls per year, including in subgroups with low vitamin D status(Reference LeBoff, Murata and Cook21). This discrepancy between observational studies and randomised controlled trials has several possible explanations. It may be that the significant association in the observational studies is due to uncontrolled confounding, particularly by factors such as visual impairment and frailty which are rarely adjusted for. However, complex temporal links may come into play, in which vitamin D deficiency may still increase the risk of falls and fractures. Vitamin D has been implicated in the pathogenesis of frailty(Reference Clegg and Hassan-Smith22), so low 25(OH)D concentration may lead to frailty, which would further decrease 25(OH)D concentration while also increasing the risk of falls and fractures. Alternatively, the lack of effect in the trials may reflect features of trial design, although the meta-analysis did not find differences according to vitamin D dose or the length of supplementation(Reference Bolland, Grey and Avenell10).
It is plausible that the risk of falls and fractures does not increase until 25(OH)D drops <25–30 nmol/l. However, most trials have had few participants with baseline 25(OH)D this low. In the meta-analysis described above and the Vital Trial, the total number of participants with this concentration was 1377, resulting in limited statistical power to detect an effect, particularly when features of trial design (such as dosing regimen) are also taken into consideration. We have not presented PAFs for this cut-point because both the prevalence and RR estimates are very imprecise. However, in the Australian Health Survey, the prevalence of 25(OH)D <30 nmol/l was 7 %, suggesting that this would make only a small contribution to hospitalisations for hip fracture and falls in Australia.
The RRs used in these analyses should be considered estimates only and are unlikely to be precise. Apart from the key issues of confounding and possible misclassification of outcomes (particularly falls), the measurement of 25(OH)D concentration has been historically unreliable, potentially resulting in misclassification of exposure(Reference Lucas, Gorman and Black23). The results pooled in meta-analyses were based on studies that used a range of different assays. Most did not use a standardised LC-MS/MS assay such as that used in the Australian Health Survey, so there is a disconnect between the assays used to generate the RRs and those used to estimate the prevalence of vitamin D deficiency. Further, the appropriate year to measure the prevalence of vitamin D deficiency relative to the year during which outcomes were captured is unclear as no study has examined serial measures of 25(OH)D concentration in association with falls or fractures.
We have analysed hospitalisations for falls and hip fractures as separate outcomes. However, a proportion of falls hospitalisations will have been for hip fracture, so some hip fractures will have been included in both datasets and the actual number of events attributable to low vitamin D status may be an overestimate. The RR estimates for falls came from studies that included all falls and not just those that resulted in hospitalisation. If low vitamin D status has a greater impact on harmful falls, the RRs for hospitalisations due to falls may be an underestimate. Further, we have not included falls that did not result in a hospital inpatient admission due to the lack of available data, and these do have deleterious consequences. On balance it seems most likely that we have underestimated, rather than overestimate, the impact of low vitamin D status on falls.
The prevalence of vitamin D deficiency is much higher in winter and spring than in summer and autumn, and there is evidence that the incidence of hip fracture is also higher in winter(Reference Pasco, Henry and Kotowicz24,Reference Lara Alvarez, Bell and Ward25) . Our analyses do not account for season, as the hospital morbidity data do not present data stratified by season, but the proportion of winter hip fractures and falls hospitalisations attributable to vitamin D deficiency may be greater than that estimated here.
Many other diseases have been linked to low 25(OH)D concentrations. For example, observational studies have consistently shown an increased risk of colorectal cancer and heart disease in people with low 25(OH)D(Reference Fatemeh, Ghobad and Bushra26,Reference Ekmekcioglu, Haluza and Kundi27) . We have not included these in this analysis due to an even greater uncertainty about whether the link is causal than that existing for falls and hip fractures, but if these associations are causal, the burden of disease attributable to low vitamin D status may be greater than we have estimated.
Notwithstanding the limitations of this analysis, our results suggest that a meaningful proportion of hospitalisations for falls and hip fractures may be attributable to low vitamin D status, even in a sunny country such as Australia. In theory, vitamin D deficiency should be avoidable for most Australians without the need for supplementation, other than for those who are unable to go outdoors or who routinely cover most of their skin with clothing. The relatively high proportion of people with low vitamin D status suggests that guidance may need to be given about optimal sun exposure for vitamin D production, but such advice needs to balance the risks and benefits of exposure. Our analyses will provide useful inputs into the models that are needed to underpin evidence-based policy and practice in Australia. It would be of value to apply similar approaches to other countries, particularly those where the prevalence of vitamin D deficiency is high.
Acknowledgements
L. F. W. is supported by an Australian National Health and Medical Research Council (NHMRC) Centres for Research Excellence grant (APP1153420). L. J. B. is supported by an MS Research Australia Postdoctoral Fellowship (18-0452) and a Curtin University Research Fellowship. R. M. L. is supported by an NHMRC Senior Research Fellowship (APP1107343).
R. E. N. conceived the study and performed the statistical analysis. L. J. B. provided the vitamin D deficiency data by accessing the publicly available dataset. All authors provided critical input into interpreting the results and preparing the manuscript.
No authors have any conflicts of interest to declare.
Supplementary material
For supplementary material/s referred to in this article, please visit https://doi.org/10.1017/S0007114521000416






