Fruits and vegetables have been widely considered as the essential components of a healthy diet, and their protective effects against CHD have been evaluated in many epidemiological studies( Reference Dauchet, Amouyel and Dallongeville 1 ). In a recent meta-analysis of prospective studies, daily consumption of more than five portions (about 400 g) of fruits and vegetables has been reported to be related to a 17 % lower risk of CHD when compared with the consumption of less than three portions per d( Reference He, Nowson and Lucas 2 ). In an earlier meta-analysis, a 4 % decrease in the risk of CHD has been found to be associated with each portion increase in fruit and vegetable intake( Reference Dauchet, Amouyel and Hercberg 3 ). However, substantial heterogeneities across studies were found in both reports, especially with regard to the association of vegetable intake with CHD risk. One possible explanation is that the types of fruits and vegetables commonly consumed and the processing methods used vary across study populations. Some specific groups of fruits and vegetables might have more benefits than others( Reference Hung, Joshipura and Jiang 4 , Reference Oude Griep, Verschuren and Kromhout 5 ). The nutrient contents may differ in cooked v. raw vegetables( Reference Oude Griep, Geleijnse and Kromhout 6 ). Furthermore, other dietary as well as lifestyle factors, such as saturated fat intake and smoking, which are correlated with fruit and vegetable intake, may modify the associations of fruit and vegetable intake with CHD risk( Reference Hung, Joshipura and Jiang 4 , Reference Tucker, Hallfrisch and Qiao 7 , Reference Joshipura, Hung and Li 8 ).
To date, most studies evaluating the association between fruit and vegetable intake and CHD risk have been conducted in the USA and Europe( Reference He, Nowson and Lucas 2 , Reference Boeing, Bechthold and Bub 9 ). It remains unclear as to whether fruit and vegetable consumption is associated with CHD risk in Asian populations who generally have dietary patterns and cooking practices different from those of Western populations. In the present study, we investigated the association of fruit and vegetable consumption with CHD risk in two prospective cohorts of middle-aged and older Chinese men and women.
Subjects and methods
Participants of the Shanghai Women's Health Study (SWHS) and the Shanghai Men's Health Study (SMHS), two population-based prospective studies, were included in the present analysis. The designs and methods have been described previously( Reference Zheng, Chow and Yang 10 , Reference Cai, Zheng and Xiang 11 ). In brief, 74 941 women aged 40–70 years were recruited from 1996 to 2000 and 61 482 men aged 40–74 years were recruited from 2002 to 2006 in urban communities in Shanghai, China. Participation rates were 92·7 and 74·1 %, respectively. In both studies, in-person interviews were conducted by trained staff using structured questionnaires to collect information on sociodemographics, diet and lifestyle habits, physical activities and medical history. Anthropometric measurements, including height and weight, were also taken at baseline. The present study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving human subjects were approved by the Institute Review Board of all institutes involved. Written informed consent was obtained from all the participants.
Dietary assessment
Food intakes were assessed using semi-quantitative FFQ in each cohort. The participants were asked, on average, how often they had consumed a specific food or food group during the preceding year and then how much they had consumed in grams per unit of time. Frequencies and amounts were converted into daily intake of each food. Total energy and nutrient intakes were calculated according to the 2002 Chinese Food Composition Tables( Reference Zhai and Yang 12 ).
The validity and reproducibility of the questionnaires used for both cohorts were evaluated and found to be fairly high. Compared with twenty-four biweekly 24 h dietary recalls, the FFQ used in the SWHS covered 86 % of the commonly consumed foods in the study population; the correlation coefficients between the estimates from the dietary recalls and those from the FFQ were 0·55 for total fruit intake and 0·41 for total vegetable intake( Reference Shu, Yang and Jin 13 ). Similarly, the FFQ used in the SMHS covered 89 % of the recorded foods, and the correlation coefficients of dietary intake estimates derived from the FFQ and the average of twelve 24 h dietary recalls were 0·72 for total fruit intake and 0·42 for total vegetable intake( Reference Villegas, Yang and Liu 14 ).
Total fruit and vegetable intake was estimated by summing the intakes of all fruit and vegetable items. Fruit items listed in the FFQ in both the SMHS and SWHS included apple, pear, citrus fruit, banana, watermelon, peach, grape and other fruits (e.g. strawberry and cantaloupe). There were thirty-three vegetable items in the SWHS FFQ, including cruciferous vegetables (bok choy, cabbage, napa cabbage, cauliflower and white turnip), allium (garlic and garlic shoots, garlic bulb, onions, green onions and Chinese chives), legumes (fresh peas, fresh soyabeans, broad beans, Chinese long beans, green beans and snow peas) and other vegetables (celery, eggplant, cucumber, mushroom, tomato, sweet potato and bean sprouts). An expanded version of the SWHS FFQ was used in the SMHS, with the addition of four cruciferous vegetable items: garland chrysanthemum; shepherd's purse; clover; amaranth. Potatoes and dried beans were not included as vegetables due to their starchy content as suggested by the World Health Organization( 15 ).
Outcome ascertainment
Both cohorts were actively followed by in-person home visits, which took place every 2–3 years, and annual linkage to vital statistics records. The overall follow-up rate was 96 % for both cohorts. Very few cohort members moved out of the study area, and these participants were treated as censored observations, using date of the last contact as the censoring date. Our primary end point was incident CHD, comprising non-fatal myocardial infarction (MI) and fatal CHD. Self-reported diagnosis of MI was further confirmed through review of the participants' medical records by physicians who were unaware of their exposure status. Cases of MI were defined according to the WHO criteria: symptoms plus either diagnostic electrocardiographic changes or elevated levels of cardiac enzymes( Reference Rose and Blackburn 16 ).
In both cohorts, almost all the participants (99·9 %) were successfully followed for their vital status. Death due to CHD was determined by medical record review whenever possible and death certificates with CHD listed as the underlying cause of death (the International Classification of Diseases, 9th Revision, ICD-9 codes 410–414). In both the SWHS and SMHS, follow-up time was calculated from the date of baseline interview to the date of incident CHD, death, loss to follow-up or 31 December 2009, whichever was first.
Statistical analyses
From the present study, we excluded 7618 women and 5804 men who reported a history of CHD, stroke or cancer at baseline (a history of cancer was an exclusion criterion for enrolment in the SMHS). We further excluded individuals with extreme energy intakes ( < 2092 or >14 644 kJ/d for women (n 112) and < 3347 or >17 573 kJ/d for men (n 204)). A total of 67 211 women and 55 474 men were included in the present analysis.
Analyses were carried out separately for each cohort in consideration of differences between the two cohorts in baseline characteristics of the participants, time period of recruitment and the duration of follow-up. Dietary intakes were adjusted for total energy using the residual method to control for confounding by total energy intake and reduce extraneous variations( Reference Willett, Howe and Kushi 17 ). Pearson's partial correlation coefficients between total fruit and vegetable intake and related nutrients were calculated with adjustment for age, sex and energy intake. The participants were then classified by quartiles of energy-adjusted intakes of total fruits and vegetables. Baseline characteristics were compared using a χ2 test for categorical variables or linear regression for continuous variables. Hazard ratios (HR) and 95 % CI were estimated by Cox proportional hazards regression models using age as timescale and stratified by birth cohort (5-year interval). In the SWHS, a multivariate model was adjusted for baseline age (continuous), BMI (kg/m2, continuous), family income (four categories), education level (four categories), smoking (since very few women ever smoked, dichotomous variable never/ever was used), alcohol consumption (never or ever, few women ever drank), physical activity level (quartiles of metabolic equivalent score, h/week)( Reference Matthews, Shu and Yang 18 ), use of aspirin and vitamin E and multivitamin supplements, menopausal status and hormone therapy (yes or no), total energy intake (kJ/d, continuous) and energy-adjusted intakes of red meat and fish/shellfish (g/d, continuous). In additional analyses, we further controlled for prior diagnoses of diabetes, hypertension or dyslipidaemia and nutrient intake (fibre, vitamin C, K or Mg). Similar covariates were included in multivariate analyses of the SMHS cohort with refined categories for smoking (never, past or current: 1–9, 10–19 and ≥ 20 cigarettes/d) and alcohol consumption (never, past or current: < 2 and ≥ 2 drinks/d). P value for trend was assessed by treating the median value of each quartile as a continuous variable.
We also evaluated the HR of CHD associated with each portion increment in daily intake of fruits and vegetables, with a portion being defined as 80 g as suggested by the WHO and previous studies( 15 , Reference Crowe, Roddam and Key 19 ). In addition, we applied restricted cubic spline regression with five knots (10th, 25th, 50th, 75th and 90th percentiles) to explore the dose–response relationships and potential optimal intakes( Reference Desquilbet and Mariotti 20 ).
In addition, we examined the HR of CHD associated with specific types of fruits and vegetables, including apples and pears, bananas, citrus fruits, watermelon, other fruits, cruciferous vegetables, allium, legumes and other vegetables. A stratified analysis was carried out based on obesity status, physical activity level, smoking and the history of hypertension and diabetes. A sensitivity analysis was carried out by excluding the first 2 years of follow-up. Proportional hazards assumption was tested using the Schoenfeld residuals, and no significant violation was found. All statistical analyses were carried out using the SAS software (version 9.3; SAS Institute, Inc.), with a two-sided P value < 0·05 being considered statistically significant.
Results
The median intakes of total fruits and vegetables were 502 (interquartile range 360–673) g/d in the SWHS and 440 (interquartile range 315–590) g/d in the SMHS. Generally, women consumed more fruits but a slightly lower amount of vegetables than men (fruit median intake: 235 v. 125 g/d; vegetable median intake: 250 v. 295 g/d). In both studies, individuals who consumed more fruits and vegetables had higher income and education, were less likely to smoke and more likely to use aspirin or vitamin supplements (Table 1). They also had greater levels of physical activity, BMI and fish/shellfish intake. The prevalence of diabetes and hypertension decreased across increasing quartiles of total fruit and vegetable intake in women but not in men. The intakes of several nutrients were highly correlated with total fruit and vegetable intake; partial Pearson's correlation coefficients were 0·81 for dietary fibre, 0·92 for vitamin C, 0·88 for K and 0·74 for Mg.
Table 1 Baseline characteristics of the participants by quartiles of total fruit and vegetable intake* (Mean values or percentages)

MET, metabolic equivalents.
* Intake values were energy adjusted using the residual method. P values were all < 0·005 (except for alcohol consumption in women (P= 0·14), age in men (P= 0·71) and diabetes in men (P= 0·36)).
† High income was defined as family income ≥ 30 000 yuan per year for women or personal income ≥ 2000 yuan per month for men.
‡ High education was defined as professional or college education or more.
During an average follow-up period of 9·8 years, 148 self-reported cases of CHD among women were confirmed by medical record review. After adjustment for potential confounding factors, including sociodemographic status, lifestyle and BMI, as well as total energy and red meat and fish intake, women in the highest quartile of total fruit and vegetable intake had a HR of 0·62 (95 % CI 0·38, 1·02) for CHD (P for trend = 0·04) compared with those in the lowest quartile (Table 2). The corresponding HR were 0·62 (95 % CI 0·37, 1·03) for fruit intake and 0·94 (95 % CI 0·59, 1·50) for vegetable intake. When we further controlled for prior history of diabetes, hypertension or dyslipidaemia, these inverse associations were attenuated with a HR of 0·67 (95 % CI 0·41, 1·10; P for trend = 0·09) comparing the extreme quartiles of total fruit and vegetable intake. Additional adjustment for dietary K or Mg, but not for fibre or vitamin C, also attenuated the inverse association (data not shown in the table).
Table 2 Hazard ratios (HR) of incident CHD by fruit and vegetable intake (Hazard ratios and 95 % confidence intervals)
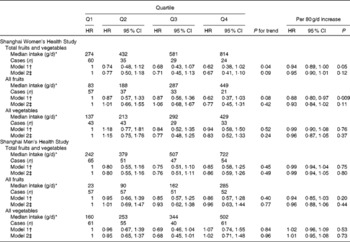
* Intake values were energy adjusted using the residual method.
† Model was stratified by birth cohort (5-year interval) and adjusted for baseline age, BMI, income, education, smoking, alcohol consumption, physical activity, use of aspirin and vitamin E and multivitamin supplements (in only women: menopause and hormone replacement therapy), total energy, and red meat and fish/shellfish intake.
‡ Further adjusted for history of diabetes, hypertension or dyslipidaemia.
In the SMHS, 217 cases were verified after a mean follow-up period of 5·4 years. No statistically significant association with CHD risk was found for fruits and vegetables when analysed either together or separately (Table 2).
To make a comparison with results of previous studies, we estimated standard portions of intake with one portion defined as 80 g. Each portion increment in total fruit and vegetable intake was associated with a 6 % reduction of incident CHD among women (HR 0·94, 95 % CI 0·89, 1·00, P= 0·05; Table 2). The spline dose–response curves also suggested that the HR for CHD decreased with each portion increment in total fruit and vegetable intake for women (Fig. 1(a)). Compared with the consumption of three portions/d, the inverse association appeared to be evident only when the intake level reached at least eight portions/d (HR 0·69, 95 % CI 0·45, 1·06). For men, the lowest HR for CHD occurred at approximately six portions per d (Fig. 1(b)).

Fig. 1 Dose–response relationships between total fruit and vegetable intake and CHD risk by restricted cubic spline analysis in Chinese (a) women and (b) men (![]() , hazard ratio;
, hazard ratio; ![]() , 95 % CI; reference: three portions/d).
, 95 % CI; reference: three portions/d).
Tables 3 and 4 report the HR of CHD associated with the major types of fruits and vegetables consumed by women and men, respectively. Higher banana intake was significantly associated with a lower risk of CHD in women, with a HR comparing the extreme quartiles of 0·48 (95 % CI 0·30, 0·78; P for trend = 0·006). Although other types of fruits also exhibited inverse associations with CHD risk, none of these associations reached statistical significance. Similar to total vegetables, no significant association was found for specific types of vegetables evaluated in either women or men.
Table 3 Hazard ratios (HR) of incident CHD by types of fruits and vegetables in the Shanghai Women's Health Study (Hazard ratios and 95 % confidence intervals)

* Intake values were energy adjusted using the residual method.
† Model was stratified by birth cohort (5-year interval) and adjusted for baseline age, BMI, income, education, smoking, alcohol consumption, physical activity, use of aspirin and vitamin E and multivitamin supplements (in only women: menopause and hormone replacement therapy), total energy, and red meat and fish/shellfish intake.
‡ Further adjusted for history of diabetes, hypertension or dyslipidaemia.
Table 4 Hazard ratios (HR) of incident CHD by types of fruits and vegetables in the Shanghai Men's Health Study (Hazard ratios and 95 % confidence intervals)

* Intake values were energy adjusted using the residual method.
† Model was stratified by birth cohort (5-year interval) and adjusted for baseline age, BMI, income, education, smoking, alcohol consumption, physical activity, use of aspirin and vitamin E and multivitamin supplements (in only women: menopause and hormone replacement therapy), total energy, and red meat and fish/shellfish intake.
‡ Further adjusted for history of diabetes, hypertension or dyslipidaemia.
In the stratified analysis, the inverse association between total fruit and vegetable intake and CHD risk seemed to be stronger in overweight and physically inactive women. The HR for each portion (80 g) increment were 0·93 (95 % CI 0·86, 1·00) and 0·98 (95 % CI 0·88, 1·09) for women with BMI ≥ 24 v. < 24 kg/m2 and 0·92 (95 % CI 0·84, 1·02) and 0·96 (95 % CI 0·89, 1·04) for physically inactive v. active women. However, none of the interactions was significant. For men, no difference in the association due to BMI or physical activity was observed. For both men and women, no effect modification by smoking or history of hypertension or diabetes was found. The sensitivity analysis indicated no material changes in the results when the first 2 years of follow-up in both cohorts were omitted.
Discussion
In these two prospective cohorts of middle-aged and older Chinese adults, we evaluated the association between fruit and vegetable intake and CHD risk. We found that each 80 g/d increase in total fruit and vegetable consumption was associated with a 6 % decrease in CHD incidence in women; this inverse association was primarily driven by fruit intake. In men, the link between fruit or vegetable intake and reduced risk of CHD was less evident.
The cardioprotective effect of fruits and vegetables might be mediated through several established CVD risk factors, such as hypertension, hypercholesterolaemia and diabetes( Reference Dauchet, Amouyel and Dallongeville 1 ). This is suggested by the findings of the present study and previous studies that the inverse associations between fruit and vegetable intake and CHD risk are attenuated when history of hypertension or diabetes is controlled for( Reference Liu, Manson and Lee 21 ). Randomised controlled trials have shown that an increased consumption of fruits and vegetables significantly reduces blood pressure( Reference Appel, Moore and Obarzanek 22 , Reference John, Ziebland and Yudkin 23 ), perhaps due to the high K and Mg contents of fruits and vegetables. Also, the high levels of fibre( Reference Brown, Rosner and Willett 24 ), plant phytosterols( Reference Thompson and Grundy 25 ) and vitamins( Reference Hamer and Chida 26 ) present in fruits and vegetables may reduce blood cholesterol levels, oxidative stress and inflammation. In the study population, the intakes of K, Mg, dietary fibre and vitamin C were highly correlated with total fruit and vegetable intake. Additional adjustment for K or Mg largely diminished the inverse association of total fruit and vegetable intake with CHD risk observed in the present study. It is plausible that the high K and Mg contents in bananas might partially explain our finding of an inverse association between banana intake and CHD risk in women and a recent report of an inverse association of banana intake with blood pressure in Asian adults( Reference Oude Griep, Stamler and Chan 27 ).
The association of fruit and vegetable intake with CHD risk observed in the SWHS is consistent with previous results in both direction and magnitude. So far, many prospective studies have been conducted among Western populations. In the Women's Health Study of 39 127 middle-aged US female health professionals, the relative risks of MI across extreme quintiles were 0·62 (95 % CI 0·37, 1·04) for total fruits and vegetables and 0·57 (95 % CI 0·34, 0·98) for all fruits( Reference Liu, Manson and Lee 21 ). Similar to that observed in the present study, after additional adjustment for CHD risk factors, including history of diabetes, hypertension and high cholesterol levels, the inverse associations became statistically non-significant. In the Nurses' Health Study, Joshipura et al. ( Reference Joshipura, Hu and Manson 28 ) found that one serving/d increase in fruit and vegetable intake was associated with a 4 % decreased risk of CHD. Data from Asian populations are limited. In the Japan Public Health Center-based Prospective Study, the consumption of fruits, but not of vegetables, was inversely associated with CVD incidence (including MI and stroke)( Reference Takachi, Inoue and Ishihara 29 ). In another Japanese cohort, a higher intake of fruits and vegetables was associated with a lower risk of death from CVD only in Japanese women but not in men( Reference Nakamura, Nagata and Oba 30 ).
As indicated in the present study and some previous studies, the inverse association with CHD risk was less consistent for vegetable intake than for fruit intake( Reference He, Nowson and Lucas 2 , Reference Dauchet, Amouyel and Hercberg 3 ). For example, total vegetable intake was not associated with MI incidence among US male physicians( Reference Liu, Lee and Ajani 31 ) or Italian women( Reference Bendinelli, Masala and Saieva 32 ), although leafy vegetables and olive oil exhibited significant inverse associations in the latter study. In Finnish male smokers( Reference Hirvonen, Pietinen and Virtanen 33 ) and in Japanese women, but not in men( Reference Nakamura, Nagata and Oba 30 ), higher vegetable intake was associated with a lower risk of non-fatal MI or CHD death. The heterogeneity might arise from differences in commonly consumed vegetables and other dietary factors and variation in traditional cooking methods across nations. In general, Chinese people, particularly the older generation such as the participants in the present study, prefer cooked vegetables rather than raw vegetables, and the most commonly used cooking methods are stir-frying and boiling. Such methods of processing vegetables may lead to the loss of water-soluble, heat-sensitive and oxygen-labile nutrients( Reference Rickman, Barrett and Bruhn 34 ). In addition, salt is typically added during home cooking, and this may offset the benefits of vegetables( Reference Anderson, Appel and Okuda 35 ). Fruits are typically eaten raw by the study population and fruit juice consumption is likely to be negligible( Reference Oude Griep, Stamler and Chan 27 ). The association of vegetable intake with CHD risk might also be modified by other dietary factors. Some studies have suggested that the cardioprotective effect of vegetables is more pronounced when combined with a diet low in carbohydrates( Reference Joshipura, Hung and Li 8 ) or high in fats( Reference Tucker, Hallfrisch and Qiao 7 , Reference Holmberg, Thelin and Stiernstrom 36 ). However, the traditional Chinese diet is featured by a high-carbohydrate and low-fat composition. In the study population, carbohydrate, total fat and saturated fat, respectively, accounted for 68, 15 and 4·5 % of total energy, compared with approximately 45, 35 and 10 % of total energy in a US population( Reference Halton, Willett and Liu 37 ). Vegetable intake was relatively high in the study population (median: 3·5 portions/d v. < 2 portions/d in the USA and North Europe( Reference Boeing, Bechthold and Bub 9 , Reference Blanck, Gillespie and Kimmons 38 ); the median for the lowest quartile in the present study was approximately two portions/d). The overall high consumption, limited consumption variability and relatively low incidence of CHD might have contributed to the less consistent association between vegetable intake and CHD risk in the present study( Reference Dauchet, Ferrieres and Arveiler 39 ).
As with most nutritional epidemiological studies, dietary assessment error is the main concern of the present study. Compared with the assessment of fruit intake, that of vegetable intake is more challenging because of the large variety of vegetables and the difficulty in estimating portions. As indicated in our validation studies, vegetable intake was assessed less accurately than fruit intake( Reference Shu, Yang and Jin 13 , Reference Villegas, Yang and Liu 14 ), and this may further explain the less consistent results that we obtained for vegetables. A Japanese cohort study has also suggested that men might report their intake less accurately than women( Reference Nakamura, Nagata and Oba 30 ). In addition to measurement error, the relatively short follow-up duration in the men's cohort could also have reduced our ability to detect significant associations. Because of the shorter follow-up period, changes in diets due to the presence of risk factors or subclinical diseases (reverse causation bias) might have had a greater influence on the results of men than on those of women. Another concern of the study is residual confounding, even though we extensively controlled for potential confounders, including socio-economic status, BMI, physical activity, smoking and other established risk factors of CHD. Fruit and vegetable intake is, in general, associated with a healthy lifestyle and likely to be included as part of a healthy dietary pattern. We adjusted for several important lifestyle and dietary variables in multivariable analyses and conducted analyses stratified by smoking, physical activity and BMI to further evaluate the independent association between fruit and vegetable intake and CHD risk and potential effect modifications. We found no evidence of significant effect modifications. Nevertheless, we cannot exclude the possibility of residual confounding or effect modifications by other unmeasured covariates. Finally, the participants were recruited from urban Shanghai, the most developed region in China, so the results may not be entirely generalisable to Chinese people living in other areas or other countries around the world. Nevertheless, to our knowledge, this is the first report on the associations of fruit and vegetable intake with CHD risk among Chinese adults with a population-based prospective design and medical record-confirmed cases.
In conclusion, the present results suggest that a higher intake of fruits may be associated with a lower risk of incident CHD in Chinese adults, particularly in women.
Acknowledgements
The present study was supported by research grants R01HL079123, R37CA070867 and R01CA082729 from the US National Institutes of Health. J. H. was a former trainee of the Vanderbilt-Shanghai Chronic Disease Research Program supported by a grant from the Fogarty International Center (D43TW008313). The US National Institutes of Health had no role in the design, analysis or writing of this article.
The authors' contributions are as follows: X. Z., Y.-T. G., G. Y., W. Z., Y.-B. X. and X.-O. S. designed the research; X. Z., Y.-T. G., H. L., G. Y., W. Z., Y.-B. X. and X.-O. S. contributed to the study implementation and data collection; D. Y. and J. H. conducted the statistical analyses and drafted the manuscript. All authors contributed to the revision of the manuscript, and read and approved the final manuscript. The authors have no conflicts of interest to declare.







